With advances in diagnostic technology, it is now accepted that in the field of functional bowel disorders, symptom-based assessment is unsatisfactory as the sole means of directing therapy. A robust taxonomy based on underlying pathophysiology has been suggested, highlighting a crucial role for physiologic testing in clinical practice. A wide number of complementary investigations currently exist for the assessment of anorectal structure and function, some of which have a clinical impact in patients with functional disorders of evacuation and continence by markedly improving diagnostic yield and altering management. The techniques, limitations, measurements, and clinical use of manometric, sensorimotor, and neurophysiologic tests of anorectal function are presented.
The two major functions of the anorectum are preservation of continence and regulation of defecation. Multiple factors are involved in the control of these processes, involving both physiologic and psychobehavioral mechanisms. Investigation of the anorectum should be performed in the context of a global pelvic floor evaluation, aimed at both morphology and anatomy, and function. With advances in diagnostic technology, it is now accepted that in the field of functional bowel disorders, symptom-based assessment, although important, is unsatisfactory as the sole means of directing therapy. The symptom repertoire of the gut is limited and relatively nonspecific, such that similar symptom profiles may reside in differing pathoetiologies and pathophysiologies. In a field of practice in which normal physiologic function is so complex, reliance on clinical symptoms alone as a basis for taxonomy is now obsolete. A robust taxonomy based on underlying pathophysiology must be paramount.
A wide number of complementary investigations currently exist for the assessment of anorectal structure and function ( Table 1 ). Ideally, a comprehensive assessment of all understood and measurable components that contribute toward continence or defecation should be performed, although in clinical practice only a limited number of factors are routinely assessed. Nevertheless, the diagnostic yield undoubtedly improves the broader the series of tests performed, and all patients should undergo as thorough an assessment as is available, performed in a structured and systematic manner. This article focuses on contemporary tests of motor and sensory function of the anorectum, and neurophysiologic assessment of the pelvic floor, with an aim to highlight their presently accepted clinical use.
| Investigation | Modality Assessed | Clinical Use |
|---|---|---|
| Anorectal manometry | (1) Anal sphincter function | Established, limited value |
| Traditional | (2) Rectoanal reflexes | Established, limited value |
| (3) Rectal sensation (balloon) | Established | |
| (4) Rectal compliance | Established, limited value | |
| (5) Defecatory maneuvers | Established | |
| (6) Saline continence test | Obsolete | |
| High resolution | See (1, 2, and 5 above) | Research |
| Vector volume | Anal sphincter function, pressure profile | Obsolete |
| Prolonged ambulatory | Anorectal/rectosigmoid motility | Research |
| Perineometer | Pelvic floor descent | Obsolete |
| Perineal dynamometer | Puborectalis function | Research |
| Barostat studies | (1) Rectal sensation | Established |
| (2) Rectal compliance | Established | |
| (3) Rectal tone, tension | Research | |
| (4) Rectal capacity | Research | |
| (5) Rectal motility | Research | |
| Impedance planimetry | Rectal biomechanical properties | Research |
| Endoanal ultrasound | Two-dimensional imaging of the anal sphincters | Established |
| Three-dimensional imaging of the anal sphincters | Research | |
| Endoanal MRI | Imaging of the anal sphincters | Research |
| Neurophysiologic | ||
| Nerve conduction | Pudendal nerve terminal motor latency | Established, limited value |
| Electromyography | (1) Motor unit action potentials | Established, limited value |
| (2) Fiber density | Established, limited value | |
| (3) Jitter | Research | |
| Evoked potentials | (1) Motor | Research |
| (2) Somatosensory | Research | |
| Other | Anocutaneous reflex | Established, limited value |
| Strength-duration test | Research | |
| Anorectal sensation | ||
| Electrostimulation | (1) Mucosal electrosensitivity | Established, limited value |
| Thermal stimulation | (2) Mucosal thermosensitivity | Research |
| Rectal evacuation | ||
| Balloon expulsion test | Rectal evacuatory function | Established |
| Evacuation proctography | Rectal evacuatory function | Established |
| Scintigraphic proctography | Rectal evacuatory function | Obsolete |
| Dynamic MRI proctography | Rectal evacuatory function, pelvic organ movement | Research |
| Colonic transit studies | ||
| Radiopaque markers | Global colonic transit | Established |
| Scintigraphy | Segmental colonic transit | Established, limited value |
Manometric evaluation
Anorectal Manometry
This is the most established and widely available investigative tool, and provides a means of evaluating various parameters of both anal and rectal function, and rectoanal coordinated activity. It is best performed in a laboratory with the necessary technical and interpretative expertise. A manometric evaluation commonly encompasses a series of measurements designed to test for (1) deficits in anal sphincter function; (2) presence or absence of rectoanal reflexes; and (3) rectal sensory function and compliance (see the section on sensorimotor evaluation). In addition, a manometric assessment may also include components designed to assess defecatory function, namely rectoanal pressure relationships during bearing down and straining maneuvers, and expulsion of a rectal balloon.
The selection (and order) of measurements to be performed depends on a number of issues, including the presenting symptoms and reason for referral. The principal indications are fecal incontinence and constipation, and certain components of a manometric investigation may be considered more useful in the former (eg, evaluation of sphincter function), whereas others may be more valuable in the latter (eg, defecatory maneuvers); however, these disorders frequently coexist and there is an increasing body of literature supporting the concept that fecal (often overflow) incontinence is frequently secondary to incomplete rectal evacuation or fecal impaction caused by disordered defecation. Consequently, a comprehensive manometric assessment incorporating all components should often be performed. Anorectal manometry may also be useful to (1) facilitate biofeedback training; (2) assess patients before surgery (eg, as a prognostic indicator of continence prior to pouch construction); (3) allow an objective assessment of therapeutic efficacy; and (4) assess patients with functional anorectal pain, particularly if this is suspected to be secondary to pelvic floor dysfunction.
Equipment
This consists of four major components: (1) a thin, flexible intraluminal pressure-sensing catheter; (2) pressure transducers; (3) a balloon for inflation within the rectum (either integral to the catheter assembly or fixed to an independent catheter); and (4) the amplification-recording-display system. Currently, a six-sensor catheter (be it either water-perfused or solid-state) of less than 5 mm diameter, configured to enable recordings from both the longitudinal and radial axis is recommended. A balloon (preferably nonlatex) of not less than 4 cm should ideally be tied to the end. One pressure sensor, and a lumen opening to allow for inflation, should be located inside the balloon. The remaining five sensors should be arranged radially and spaced 1 cm apart. Various computerized amplification and recording systems are commercially available, complete with dedicated online display, review, and analysis software. All allow large-volume data storage, with database functionality. Small, portable recorders are also available, which enable ambulatory measurements. Calibration of the manometric system is essential to yield accurate, reliable, and clinically helpful manometric data. This should be done in accordance with the manufacturer’s recommended guidelines.
Limitations
Recorded pressures depend on the technique used to measure them, and are influenced by a number of factors, including the pressure sensor itself; the recording technique; catheter diameter; orientation of the recording ports and sensors; perfusion rate (for perfused-tube catheters); patient posture; and patient compliance. All of these factors must be borne in mind when both performing and interpreting these tests.
Unfortunately, the biggest pitfall with anorectal manometry is the lack of uniformity regarding equipment and technique, consequently, large and robust normative reference data sets, obtained in age- and gender-matched subjects, are generally lacking from the literature. Although several working party or position papers have been published, they fail to reach consensus opinion as to the optimal method for performing a manometric assessment. As a consequence, comparison of results between centers is problematic. Each individual institution is encouraged to develop its own control values (preferably gender and age stratified) or, if using normative data from the literature, adopt similar methodology, such that a particular result may be compared with the appropriate normal range.
Patient preparation
Because of the minimal risks associated with manometry, written consent is considered optional. The patient should be fully informed about the details of the procedure, however, which enhances subject cooperation and comfort. Bowel preparation is also optional, and should only be required if fecal loading is detected on digital rectal examination; either a 500-mL tap water enema or phosphate enema have been advocated. Tests should be performed with the patient in the left-lateral position with knees and hips flexed.
Anal Sphincter Function
Technique
The objectives of assessment are to (1) identify the functional anal canal length; (2) record maximum resting anal canal tone, which predominantly reflects internal anal sphincter (IAS) function; and (3) record voluntary anal squeeze pressures, which reflects external anal sphincter (EAS) function.
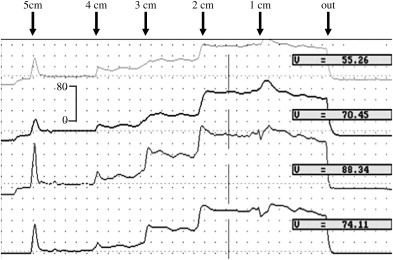
Two methods can be used: station or manual pull-through of the catheter, or stationary. The former is recommended, and the most commonly used technique. The manometry catheter is advanced into the rectum, and then withdrawn manually by 0.5- or 1-cm increments, or “stations.” For each station, the pressure should be allowed to stabilize. When the recording sensors pass into the high-pressure zone, there is an increase in pressure. The maximal resting anal pressures at each station should be recorded, as should the longitudinal position of the peak resting pressure. For evaluation of anal squeeze pressures, the procedure should be repeated; once the pressure has stabilized at each station, the patient is instructed to squeeze their anus as hard as possible. It is important to limit gluteal muscle involvement. The squeeze should be sustained for 30 seconds, which gives a measure of fatigability of the EAS. The maximal pressure obtained at each station during the squeeze maneuver and longitudinal position of the peak squeeze pressure are recorded.
Others advocate the use of a stationary technique, which is more time-efficient. Basal anal pressures are measured along the anal canal by averaging recordings at each longitudinal recording site over a 1-minute segment at rest. Squeeze pressures are evaluated by asking the patient to squeeze their anal canal two or three times, as above.
Measurements and clinical use
Functional anal canal length
This is defined as the length of the anal canal over which resting pressure exceeds that of the rectum by greater than 5 mm Hg, or alternatively, as the length of the anal canal over which pressures are greater than half of the maximal pressure at rest. The length of the functional anal canal is usually shorter in incontinent patients than normal control subjects, although the clinical significance of this measure has recently been questioned.
Anal resting pressures
Maximal resting anal pressure is defined as the difference between intrarectal pressure and the highest recorded anal sphincter pressure at rest, and is generally recorded 1 to 2 cm cephalad to the anal verge, which corresponds to the condensation of smooth muscle fibers of the IAS; pressure at the level of the anal margin can alternatively be used as the zero baseline ( Fig. 1 ). Anal resting tone is subject to pressure oscillations caused by slow waves, of amplitude 5 to 25 mm Hg, occurring at a frequency of 6 to 20 min −1 , or high-amplitude ultraslow waves, 30 to 100 mm Hg in magnitude, occurring at 0.5 to 2 min −1 (although the latter are rarely observed in patients with low resting pressures).
The primary component contributing to anal resting tone is IAS activity (55%–80%, of which most is nerve-induced, and the remainder is purely myogenic). Symptoms of passive fecal incontinence correlate with low resting anal tone and often a reversal of the anal pressure gradient; this implies IAS weakness, typically caused by rupture of the smooth muscle ring, or secondary to IAS degeneration. Patients with very low basal pressures may be fully continent, and conversely those with normal resting tone may be incontinent. Consequently, measurement of resting tone, although of pathophysiologic significance in patients with incontinence, must be considered in combination with other functional findings. Indeed, one large study showed that maximal anal resting tone had a sensitivity of only 32% for discriminating continent from incontinent patients; this emphasizes the multifactorial nature of incontinence.
Anal squeeze pressures
The measure of a patient’s ability to squeeze their striated anal musculature can be calculated as the maximal voluntary anal squeeze pressure (the difference between intrarectal pressure, or the pressure at the level of the anal margin, and the highest recorded pressure during anal squeeze), or the maximal voluntary anal squeeze increment (the difference between resting pressure at any given level of the anal canal, and the highest recorded pressure during anal squeeze); the latter is probably a better determinant of anal squeeze function. The duration of the sustained squeeze can be defined as the time interval at which the subject can maintain squeeze pressure at greater than or equal to 50% of the maximum squeeze pressure.
The squeeze increment is essentially contributed by the EAS, and also by contraction of the puborectalis sling. Low or poorly sustained squeeze pressures implies EAS weakness. Standard manometry cannot differentiate, however, between compromised muscle integrity or impaired innervation, or both (or indeed a poorly compliant patient ) as a cause of that weakness.
Symptoms of urge or stress fecal incontinence often correlate with low anal squeeze pressures, with the major causative factor being obstetric injury. In addition, squeeze duration is reduced and fatigue rate is significantly shortened in incontinent patients compared with controls. Of all standard measures of anorectal function, anal squeeze pressure has been shown to have the greatest sensitivity and specificity for discriminating patients with fecal incontinence from continent patients and controls; nevertheless, the correlation between anal canal pressures and incontinence is not perfect, given the wide range of normal values and the contribution of those various other factors crucial to anorectal continence.
An exciting recent technologic development is the advent of so-called “high-resolution manometry,” which uses multiple closely spaced sensors simultaneously to measure circumferential pressures. By interpolating between adjacent sensors, intraluminal pressure becomes a spatial continuum; recorded data are displayed as pressure topography plots, rather than overlapping line traces, with pressure magnitude indicated by color intensity. As is happening in the field of esophageal function testing, it is feasible that high-resolution manometry may challenge conventional anorectal manometry, which has been in clinical use for 30 years, as the principal tool for the evaluation of anal sphincter function. Vector manometry, which was designed to assess the circumferential symmetry of anal canal pressures and permit the identification of localized pressure defects, has been superseded by endoanal ultrasound.
Rectoanal Reflex Activity
Rapid distention of the rectum, mimicking the sudden arrival of a fecal bolus, induces a sequence of events: (1) a transient increase in rectal pressure, probably caused by secondary rectal contractions, followed by; (2) a transient increase in anal pressure, associated with EAS contraction (the rectoanal contractile reflex), followed in turn by; (3) a more prolonged reduction in anal pressure, associated with relaxation of the IAS (the rectoanal inhibitory reflex). The rectoanal inhibitory reflex is thought to allow rectal contents to be sampled by the sensory area of the anal canal, allowing discrimination between flatus and fecal matter (ie, fine-tuning of the continence mechanism). By contrast, the rectoanal contractile reflex is a compensatory guarding mechanism that allows a positive anal-to-rectal pressure gradient to be maintained during transient increases in intra-abdominal or intrarectal pressure (eg, coughing), which is essential for preservation of continence.
Technique
The rectoanal inhibitory reflex can be simply measured by concomitantly recording resting anal pressures during inflation of the rectal balloon with air, using a rapid intermittent distention technique (incrementally in 10-mL or 50-mL aliquots). The threshold volume needed to elicit the reflex and the duration of the response at each distention volume should be recorded. The rectoanal contractile reflex can be measured simultaneously during the same procedure. Alternatively, this can be evaluated by instructing the patient to blow up a party balloon, blow against a fixed pressure level into a manometer, or cough strongly (the cough reflex). The aim is to determine whether a positive anal-to-rectal pressure differential is maintained. This test is also useful for further evaluation of EAS function, especially in those patients with apparently attenuated voluntary anal squeeze pressures in whom poor compliance is suspected.
Measurements and clinical use
The rectoanal inhibitory reflex is an intramural reflex mediated by the myenteric plexus, and modulated by the spinal cord. The amplitude and duration of relaxation are correlated with the distending volume. Classically, the rectoanal inhibitory reflex is absent in patients with Hirschsprung’s disease, although the clinical use of this observation is negligible in an adult gastroenterologic practice, because undiagnosed Hirschsprung’s disease in this population is exceptionally rare. Differences in reflex parameters have been shown between incontinent patients and healthy subjects, but the clinical significance of these findings is unclear.
The rectoanal contractile reflex is a polysynaptic sacral reflex, which results in a contraction of the EAS. Under normal circumstances, intra-anal pressure should exceed intrarectal pressure, and the duration of the reflex anal contraction should be longer than the intra-abdominal pressure peak. An abnormal reflex response, along with attenuated voluntary squeeze pressures, indicates neural damage of the sacral arc, either of the spinal sacral segments or the pudendal nerves; such patients usually suffer from urge incontinence, and may have a lesion of the cauda equina or sacral plexus, a pudendal neuropathy, or more generalized peripheral neuropathy (eg, diabetes). The reflex is preserved in patients with a supraconal spinal cord lesion, but in such individuals, voluntary squeeze pressures are impaired or absent. There are no data on the specificity of this reflex. In clinical practice, it may be most useful to check a patient’s compliance with instructions to squeeze, but in those without overt neurologic signs or evidence of spinal damage, an abnormal reflex may be interpreted as a subclinical neuropathy.
Rectoanal Pressure Relationships During Defecatory Maneuvers
In patients with symptoms of disordered rectal evacuation, which are suspected to be caused by pelvic floor dysfunction, simple manometric assessment of rectoanal coordination during defecatory maneuvers, such as bearing down or straining, can be performed. Normally, these result in an increase in intrarectal pressure caused by the Valsalva maneuver, associated with a decrease in intra-anal pressure, caused by coordinated relaxation of the EAS. This process is under voluntary control, and is most likely a learned response. The cough reflex is likely inhibited concomitantly by descending inhibitory pathways. These mechanisms facilitate the process of defecation. An inability to perform this coordinated movement has been proposed to represent the principal pathophysiologic mechanism in patients with a functional defecation disorder, variably termed “dyssynergic defecation,” “anismus,” “outlet dysfunction,” “functional outlet obstruction,” or “pelvic floor dyssynergia”.
Technique
Intra-anal and intrarectal pressures (from within the rectal balloon, which may or may not be distended ) should be recorded simultaneously while the patient is asked to strain as if to defecate. There is no agreed method for this technique. It is important to limit movement of the pressure-sensing device within the anal canal.
Measurements and clinical use
Straining should induce a relaxation of the anal canal in asymptomatic subjects ( Fig. 2 A ). Three dyssynergic patterns of defecation, however, may be evidenced (see Fig. 2 B): (1) type 1, a paradoxic increase in intra-anal pressure in the presence of adequate expulsive forces (increase in intrarectal pressure); (2) type 2, an inability to generate adequate expulsive forces (no increase in intrarectal pressure), together with a paradoxic increase in intra-anal pressure; and (3) type 3, generation of adequate expulsive forces (increase in intrarectal pressure), but absent or incomplete (<20%) reduction in intra-anal pressure. These findings alone, however, are not diagnostic for a functional defecation disorder, which requires further supportive clinical evidence. Nevertheless, the test may be useful in identifying patients who are amenable to biofeedback therapy.
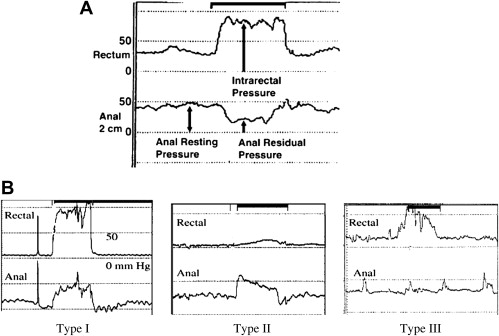
In constipated patients, a positive yield for dyssynergia using anorectal manometry has been shown to vary between 20% and 75%. The test has been criticized, however, on a number of fronts: notably, manometry is conducted in the horizontal position, and expulsion efforts do not mimic normal defecation; patient cooperation is the key component, and some patients’ embarrassment at the nature of this test may inhibit normal evacuation. Taken together, these factors likely lead to an overdiagnosis of dyssynergia.
Balloon Expulsion Test
This represents an extension to the previously mentioned method of assessing rectoanal co-ordination during defecatory maneuvers. The test evaluates a patient’s ability to expel a filled balloon from the rectum, providing a simple and more physiologic assessment of (simulated) defecation dynamics.
Technique
After inflation of the catheter-mounted balloon with either water at 37°C or air, the patient can be transferred to a commode and instructed to expel the balloon. The time taken for expulsion should be recorded and intraballoon pressure monitored concomitantly to evaluate changes in intrarectal pressure. Inflation volume is typically 50 mL; however, a recent study advocated the individualization of volumes dependent on sensation thresholds, because a sustained desire to defecate is fundamental to initiate a defecatory maneuver.
Measurements and clinical use
Asymptomatic subjects can expel the balloon in a median of 50 seconds (range, 10–300) with an increase in intra-abdominal pressure of greater than 80 mm Hg. Despite generating similar increases in intra-abdominal and pelvic pressure on straining as normal subjects, patients with constipation are often unable to expel a filled balloon, which may be secondary to functional or mechanic outlet obstruction. In others, expulsive forces are inadequate to facilitate passage of the balloon. In a recent large study, the balloon expulsion test was shown to have a sensitivity of 88% and positive predictive value of 64% for diagnosing pelvic floor dysfunction and dyssynergic defecation; the specificity was 89%, with a negative predictive value of 97%. Although balloon expulsion represents a simple, useful screening test for a functional defecation disorder, results should be interpreted alongside those of other tests of anorectal function. Evacuation proctography remains the gold standard method for investigating the process of rectal evacuation.
In patients with fecal incontinence, most have no problems expelling the balloon. In those presenting with fecal seepage, however, many demonstrate impaired evacuation, suggesting that a disorder of defecation may underlie their symptoms, and this may be allied to blunted perception of rectal sensation (hyposensitivity).
Ambulatory Anorectal Manometry
Prolonged assessment of intraluminal motor activity from the anorectum, using a manometric catheter incorporating several solid-state pressure microtransducers, connected to a portable solid-state recorder, may provide further invaluable information regarding the pathophysiology of colorectal disorders; such techniques are gaining more widespread use. The test is designed to monitor intraluminal pressure changes under normal physiologic conditions, over prolonged periods, in ambulant subjects. This is particularly useful in patients in whom symptoms are intermittent, where an extended recording period may enable symptom episodes (eg, urgency, incontinence ) to be correlated with motor events (ie, contraction or relaxation). Such studies are time-intensive and technologically challenging, however, notably in terms of data interpretation and analysis. In addition, there is a relative paucity of data on normal motor function. The clinical value of prolonged ambulatory anorectal manometry remains unproved.
Sensorimotor evaluation
The anal canal and rectum, together with the surrounding pelvic floor musculature, form an integrated functional unit. The anorectum is richly innervated by extrinsic sensory, motor, and autonomic nerves, and by the intrinsic enteric nervous system. Accordingly, comprehensive evaluation of both sensory and motor function necessitates the use of various complementary and integrated tests. This assessment is further complicated because the innervation of the anal canal and rectum is distinct neuroanatomically, with the somatic nervous system innervating the anal canal and the rectum receiving predominantly autonomic innervation ( Table 2 ). Measurement of sensory and motor function of the somatic nervous system is relatively straightforward, but this is not the case with respect to the autonomic nervous system. For the description that follows, tests of anorectal sensorimotor function are considered in isolation, although it should be remembered that they are frequently performed as part of the overall objective evaluation of anorectal function in conjunction with the other complementary physiologic investigations described in this article.
| Structure | Innervation | Sensory Component | Motor Component |
|---|---|---|---|
| Anus | PNS | Pudendal (somatic) afferents | Inferior rectal (hemorrhoidal) nerve |
| Rectum | ANS | Rectospinal (visceral) afferents | Superior-inferior mesenteric (pelvic) plexus |
Assessment of Anal Sensorimotor Function
Anal sensation
The epithelium of anal canal has a rich somatic sensory nerve supply made up of both free and organized nerve endings. The modalities of anal sensation can be precisely defined, with stimuli, such as touch, pain, and temperature, being readily appreciated.
Technique
Anal sensation to touch may be assessed using von Frey hairs, although this only provides qualitative data, and thus assessment using mucosal electrosensitivity and temperature sensation is preferred because these yield quantitative measurements. Anal mucosal electrosensitivity can be quantified using a catheter-mounted bipolar ring electrode inserted into the anal canal. A current is passed through the electrode and steadily increased until sensation threshold (usually reported as a prickling feeling) is noted by the patient. An alternative measure for anal sensation is using thermal stimulation by specialized thermoprobes, which provide both hot and cold stimuli.
Measurements and clinical use
Normal ranges for mucosal electrosensitivity have been defined; the threshold for mucosal electrosensitivity increases with age (indicating reduced anal sensitivity), and the upper anal canal seems to be less sensitive to stimulation than the distal anal canal. With thermal stimulation, normal individuals can detect median temperature changes of around 1°C. Diminished anal mucosal sensitivity (ie, elevated mucosal electrosensitivity and thermal thresholds) has been reported in patients with fecal incontinence, diabetes mellitus, marked perineal descent, constipation, hemorrhoids, and mucosal prolapse. Assessment of anal canal sensation, however, is not of established clinical value.
Anal motor function
This is covered in the previous section on anal sphincter function and the later section on pudendal nerve terminal motor latencies (PNTML) and electromyography (EMG).
Evaluation of Rectal Sensorimotor Function
Evaluation of rectal sensitivity involves the presentation of a stimulus and the measurement of the perceived response to the stimulus. The available techniques are shown in Table 3 . For the assessment of rectal (efferent) motor function ( Table 4 ), manometry and balloon expulsion are discussed previously; consequently, this section concentrates on the evaluation of rectal biomechanic properties.
| Stimulation | Response |
|---|---|
| Mechanical Distention | Subjective Assessment of Conscious Perception |
| Latex balloon with hand-held syringe | Quantification of sensory thresholds |
| Polyethylene bag attached to a barostat | Verbal descriptive (Likert) scales |
| Visual analog scales | |
| Direct stimulation of rectal mucosa | Quantification of reflex response |
| Electrical | RIII reflex |
| Thermal | |
| Multimodal | Objective central representation |
| Mechanical, thermal, electrical, impedance planimetry | Cortical evoked potentials |
| Functional MRI |
| Method | Measurement | Rationale |
|---|---|---|
| Static / ambulatory manometry | Intraluminal pressure changes | Reflects rectal contractile activity |
| Barostat / impedance planimetry | Rectal biomechanical properties (tone, compliance, strain, stress, and so forth) | Reflects, in part, neurogenic function of rectal smooth muscle |
| Evacuation proctography, balloon expulsion | Rectal evacuatory function | Summated end-product of motor function |
Equipment
Latex balloon distention
For simplicity and economy, rectal sensorimotor function can be assessed using a latex balloon secured to a catheter that is distended (manually or pump-assisted) with air or water, . Incorporating water-perfused catheters or microtransducers within the rectal balloon allows the simultaneous acquisition of intraballoon (rectal) pressures and distending volumes, and thus calculation of rectal compliance (see later).
Barostat assembly
The barostat is a computer-driven device that consists of a pressure transducer coupled through an electronic relay servomechanism and an electric motor to a pneumatic pump. The assembly required to study rectal sensorimotor function consists of an oversized polyethylene bag (infinitely compliant within the range of distention) connected to the barostat by means of a closed-tip double-lumen polyvinyl tube rectal catheter. One lumen is used for inflation, whereas the other is connected to the pressure transducer port of the barostat and is used to monitor pressure directly within the barostat bag. The use of this equipment has certain advantages over the use of latex balloon that is manually distended: (1) the bag is secured at both ends to the catheter, which ensures distention in the circumferential axis by eliminating axial migration into the sigmoid colon; (2) simultaneous acquisition of volume and pressure data is possible, and it is not subject to the same limitations as volume-based (simple balloon) distention techniques; and (3) the distention is computerized, which allows distention parameters known to affect visceral sensitivity (see later), such as rate and pattern of inflation, to be tightly controlled and standardized using the barostat computer software. In addition, the influence of response bias may be minimized.
Patient preparation
To enable accurate evaluation, all variables that may influence measurements should be kept constant between studies. Certain guidelines have been detailed in the report of an international working group. Whether subjects should receive bowel preparation remains a contentious issue; cleansing the studied segment of gut is preferable, but the use of bowel preparation may influence the sensorimotor properties of that segment. The subject should be positioned prone.
Rectal Sensation
The importance of rectal sensory dysfunction is increasingly recognized in the development of functional bowel disorders. Although the rectum is sensitive to electrical and thermal stimulation, mechanical distention is the most reliable and physiologic stimulus for the assessment of sensation.
Technique
Simple balloon distention
Rectal sensation is most effectively and conveniently quantified in everyday clinical practice by manually distending a latex balloon with air, using a hand-held syringe. Two techniques are used for inflation: ramp (continual) or intermittent, which can be either phasic (volumes injected and then withdrawn) or stepwise (volumes maintained between inflations). Sensory responses are altered by (1) the type of inflation; (2) the distending medium (air or water); (3) speed of inflation; (4) the distance of the balloon from the anal verge; (5) the position of the patient; and (6) the biomechanic and structural properties of the rectum.
Barostat distention
The computerized barostat is now the method of choice for the evaluation of various components of rectal sensorimotor function. For assessment of rectal sensitivity, either phasic or stepwise isobaric distention paradigms may be used with good reproducibility for both being reported. The “ascending method of limits,” which involves the presentation of an increasing stimulus until perceived by the subject, is usually used to measure sensory thresholds during distention. The use of such a predictable protocol, however, may incur response bias. Various approaches have been adopted to reduce this. Recently, the Mayo group has assessed visceral sensitivity using stepwise distention from 0 to 60 mm Hg in 4–mm Hg steps every 1 minute (ascending method of limits) and four random-order phasic distentions of pressures set at 12, 24, 36, and 48 mm Hg above the basal operating pressure. Measurement of rectal sensitivity (and compliance and tone) are only reproducible after a conditioning distention, however, which usually involves distention from 0 to 36 mm Hg (or to maximum toleration) in 4–mm Hg increments at 30-second intervals.
Direct stimulation of the rectal mucosa (nonmechanical distention): thermal and electrostimulation
The application of an electrical stimulus of 500-μs duration and 10-Hz frequency to the rectal mucosa has been successfully used to assess rectal sensory function. Similarly, thermal (cold or warm) stimulation may be applied to the rectum using intraluminal water-filled bags or thermal probes. A specifically designed thermal probe, capable of achieving temperatures from 38°C to 51°C, has proved useful in the investigation of rectal sensory function.
Measurements and clinical use
Simple balloon distention
During distention, subjects are instructed to volunteer a range of sensations: first sensation; constant (flatus) sensation (optional); desire to defecate; and maximum toleration. The distending volume (or pressure) at each of these sensory thresholds is then recorded. Despite large intersubject variation, several studies have reported a high degree of reproducibility with regard to recorded sensory thresholds, notably for maximum tolerable volume. In recent years, consensus statements and technical and performance reviews have acknowledged that evaluation of rectal sensory function using simple balloon distention is useful in the assessment of functional gastrointestinal disorders, has an accepted place in the clinical management of patients with anorectal disorders, and is of established value in terms of diagnostic potential. It is important, however, to consider that this technique measures “rectal perception of distention” and not (necessarily) “afferent nerve function.”
Barostat distention
Conscious perception can be measured by recording the volumes or pressures required to trigger rectal sensations, as with simple balloon distention. Alternatively, perception can be recorded using a rating scales, such as verbal descriptive (Likert) scales and visual analog scales. The Mayo group has evaluated rectal sensitivity by recording sensory pressure thresholds during an “ascending method of limits” stepwise distention and by recording symptom ratings for gas, urgency, discomfort, and pain during four random order phasic distentions.
Direct stimulation of the rectal mucosa (nonmechanical distention): thermal and electrostimulation
Electrical stimulation of the rectal mucosa results in the perception of a discomfort, tingling or burning. Previously, it has been shown that it is safe and reproducible, and that the results correlate well with the findings of simple balloon distention. It has been criticized, however, because results may be influenced by loss of contact with the rectal mucosa, and the presence of feces in the rectum. Thermal stimulation is most commonly described by subjects as a prickling or sharp feeling, or an aching or throbbing sensation. A recent study has confirmed that a sensory response is perceived by all subjects at temperatures above 43°C, and that heat stimulation is a reproducible, simple technique that agrees well with simple balloon distention in the assessment of rectal sensitivity in healthy volunteers. At the current time, the value of both these techniques is yet to be established and they remain confined to the research setting.
Overall, irrespective of stimulation technique used, once normal ranges have been determined in healthy control subjects, abnormalities of rectal sensitivity may be defined. Heightened sensory awareness (rectal hypersensitivity) is suggested by sensory threshold volumes (or pressures) reduced below the normal range or verbal descriptive or visual analog scale scores elevated above the normal range. By contrast, impaired or blunted rectal sensitivity (rectal hyposensitivity) is suggested by the presence of elevated sensory threshold volumes (or pressures) or reduced verbal descriptive or visual analog scale scores compared with the normal range. Both rectal hypersensitivity and hyposensitivity have been reported in functional bowel disorders.
Limitations and implications for the assessment of rectal sensitivity in clinical practice
Traditionally, it has been considered that alteration of perception of rectal distention automatically indicates afferent nerve dysfunction, such as that which may occur following nerve or spinal injury. Abnormal sensory threshold volumes during simple balloon distention may not accurately reflect the function of visceral afferents under certain circumstances, however, because such volumes may be influenced by structural or biomechanic properties of the rectum. For example, in the presence of increased rectal diameter or compliance, greater volumes are required to distend and stimulate the rectum, and elevated sensory threshold volumes may conceivably reflect increased rectal size and inadequate stimulation, rather than dysfunction of the rectal afferent pathway itself.
Some advocate the measurement of sensory threshold pressures rather than volumes. Changes in pressure are not the direct stimulus for rectal perception, however, because rectal mechanoreceptors are stimulated by forces (strains) and deformations (stresses) acting in the rectal wall. Isobaric distention is not guaranteed to control adequately for differing biomechanic properties. Furthermore, the measurement of threshold pressures in the evaluation of rectal sensitivity is less practical in the clinical setting.
Techniques that involve direct stimulation of the rectal mucosa have the advantage of not being influenced by abnormal rectal wall properties, because they rely solely on direct contact with the mucosa, and they offer more accurate evaluation of the rectal afferent nerve pathway. Their impact on clinical management, however, remains less certain. In patients with abnormal sensory threshold volumes to balloon distention, however, the use of such complementary techniques may be indicated.
Rectal Compliance
Rectal compliance refers to the ability of the rectum to distend, and is defined as the “volume response to an imposed pressure”. The rectum initially actively relaxes in response to distention, and this “adaptive relaxation,” facilitated by its viscoelastic properties, allows accommodation of significant increases in volume while maintaining low intraluminal pressures, so that continence is not threatened. With continued distention, the rectal wall becomes more resistant to stretch as its elastic limit is approached, and there are regular contractions of the rectal wall, causing intrarectal pressure to rise.
Technique
Although feasible using conventional latex balloon distention, rectal compliance can be most accurately assessed using the barostat, which minimizes both observer bias and error. Measurement by means of latex (or equivalent) balloons requires correction to account for their intrinsic elasticity. Oversized polyethylene bags are favored; provided that the range of volumes used for the study remains below 90% of the maximum volume of the bag, polyethylene can be regarded as infinitely compliant, in that its own properties have no influence on the internal pressure. Using an intermittent balloon distention technique, intrabag (intrarectal) volumes and pressures are recorded concomitantly. The pressure-volume relationship of the rectum during distention, necessary for the calculation of rectal compliance, can be evaluated using a variety of paradigms, although phasic distention is most commonly used, often with simultaneous assessment of sensitivity. It is important that each distending level is maintained for some time (typically 30–60 seconds) to enable the rectum to adapt to a steady state and for accurate measurements to be obtained. A typical recording of pressures and volumes during phasic isobaric distention using a barostat is shown in Fig. 3 A .









