Restorative proctocol ectomy is the elective surgical procedure of choice for most patients who have ulcerative colitis or familial adenomatous polyposis. This major advance has offered an alternative to permanent ileostomy in these patients.
Restorative proctocolectomy (RPC) is the elective surgical procedure of choice for most patients who have ulcerative colitis or familial adenomatous polyposis. RPC involves removal of the colon and rectum, construction of a reservoir or pouch from the last 30 to 40 cm of ileum, followed by an ileoanal anastomosis. Today, most surgeons use a J pouch or two-loop pouch configuration, owing to the ease of construction, although other designs such as the W pouch or four-loop pouch may result in lower frequency of defecation. It is, however, technically more difficult to construct. In forming the ileoanal anastomosis, the surgeon either can staple or hand-sew the pouch to the anal canal. This is an important difference, because stapling leaves a 1 to 2 cm cuff of residual rectum in situ, which may become symptomatic and is at risk of dysplasia. The hand sewn technique includes a mucosectomy to remove virtually all anorectal mucosa and places the anastomosis just above the dentate line, but it may be associated with a higher incidence of minor anal leakage. When an ileostomy is performed, it is closed at about 8 weeks, provided the anastomosis has healed as judged by digital examination and a contrast enema.
RPC results in good functional outcomes and quality of life in most patients but fails in between 3.5% and 17% per cent, necessitating excision of the pouch or indefinite fecal diversion. The failure rate increases with the duration of follow-up and may occur early, within the first postoperative year, or at any time thereafter. The overall cumulative failure taking all patients irrespective of diagnosis is approximately 5% at 5 years, 10% at 10 years and 15% at 15 years.
Reports of long-term function over 10 to 20 years have demonstrated a median stool frequency per 24 hours of four to eight, with about half of patients needing to evacuate at night. This is stable over 25 years. Urgency is uncommon (5%), although there is some evidence that it increases with time. Fecal leakage during the day occurs in less than 4% of patients and is stable over 25 years. At night, these rates are 4% at 10 years, rising to 9% at 25 years. Seepage during the day and at night occurs in 7% and 9% of patients, rising to 11% and 18% of patients, respectively, at 25 years. Antidiarrheal medication is required in about a third of patients at 10 years and in 45% of patients at 25 years.
For patients in whom failure is threatened, revisional or redo surgery may be indicated. There are four causes of ileal pouch failure: (1) acute and chronic sepsis, (2) poor function for mechanical or functional reasons, (3) mucosal inflammation (pouchitis), and (4) neoplastic transformation. Of these, sepsis is the most common, being responsible for over 50% of all failures. Poor function accounts for about a third of failures and pouchitis for 10%. Neoplastic transformation is uncommon, and in these patients excision of the pouch is indicated. For the larger group of patients without neoplastic transformation in whom failure is threatened, various factors need to be considered when advising revisional pouch surgery. These include the feasibility of success, the magnitude of the proposed operation, the overall duration of treatment, and the patient’s wishes. The potential morbidity of excision of the reservoir resulting in a permanent ileostomy also should be discussed, including the possibility of a high-output ileostomy, pelvic nerve damage, and an unhealed perineal wound. These complications occur in 50% or more of patients undergoing excision of the pouch.
Sepsis
Pelvic sepsis after restorative proctocolectomy occurs in 3% to 25% of cases and its incidence appears to decrease as surgical experience increases. Pelvic sepsis may present in the early postoperative period, or it may be delayed, manifesting as abscess formation (usually presacral) or fistulation (in females usually into the vagina), often with a history of an anastomotic complication.
Early Sepsis
Patients who develop sepsis in the early postoperative period have a cumulative incidence of subsequent failure five times that of the whole population of patients undergoing restorative proctocolectomy. Symptoms of early pelvic sepsis include fever, anal pain, tenesmus, and discharge of pus or secondary hemorrhage through the anus. The diagnosis is established by digital examination (under anesthesia if necessary), combined with imaging, including contrast pouchography, CT, and MRI.
Management
In a proportion of patients the condition resolves spontaneously. Others need operative endoanal, or imaging-guided percutaneous, drainage. If drainage of the cavity is unsatisfactory, an attempt can be made to deroof the abscess and curette the cavity through the anus, creating a large communication between the abscess and the reservoir. Sometimes several local procedures are needed to eradicate sepsis. Rarely, an abdominal approach is indicated. When sepsis is severe enough to warrant a laparotomy, the functional outcome is poor, often followed by failure.
When anastomotic disruption is the cause of pelvic sepsis, after drainage and curettage, transanal repair of the anastomosis or advancement of the ileum and resuturing of the ileoanal anastomosis have been advocated. In a report of 15 patients who were found to have partial anastomotic disruption between 7 and 90 days after surgery, seven were treated by resuturing of the anastomotic defect and counter drainage, with success in three. Seven others underwent a pouch advancement procedure, with success in five. Thus, over a follow-up of 1 to 22 months, successful salvage was achieved in eight of the 15 patients.
Severe acute pelvic sepsis with extensive anastomotic breakdown occurs in 5% to 15% of patients and results in early failure in around 30% of patients, despite adequate drainage. Attempts at salvage by direct suture may work for some patients. The occurrence of early sepsis renders the patient at increased risk of subsequent failure compared with the total population. In a report by Heuschen and colleagues, only 16.8% of the 131 patients who had sepsis could be managed conservatively, the rest requiring some form of surgical procedure. Patients who had early postoperative sepsis, however, were not distinguished from those in whom sepsis developed during subsequent follow-up, although there was no significant difference in the failure rate when salvage surgery was undertaken within or beyond 6 months of restorative proctocolectomy. As might be expected, failure was related to the magnitude of the procedure, 6.1% per cent after minor intervention (33 patients) compared with 47.3% after major surgery (74 patients).
Delayed Sepsis
Delayed abdominal or pelvic sepsis presents as chronic abscess formation with or without fistulation. MRI using short-tau inversion recovery (STIR) settings may make the diagnosis in some patients in whom clinical examination, contrast radiography, or CT has not been successful. When sepsis is limited, there is a good chance of healing, provided that drainage is adequate. If resolution does not occur, there are two surgical options, including excision of the pouch or an attempt at salvage, usually by means of an abdominal approach.
Management
There is a considerable variation in the reported success of abdominal salvage surgery. Satisfactory success rates were reported in a series of 35 patients who had chronic sepsis, either abscess or fistulation, including 22 who had ulcerative colitis, 10 who had Crohn’s disease, one who had indeterminate colitis, and two who had familial adenomatous polyposis. Twenty-nine patients had leakage from the ileoanal anastomosis and four from the upper pouch. Overall a pelvic abscess was present in 25 patients, and 10 had a vaginal and 12 a perineal fistula. All underwent abdominal revision with detachment of the ileoanal anastomosis, curettage of any chronic abscess cavity with drainage or repair of fistula, and reanastomosis. The median interval between the first operation and revision was 24 months. At a median follow-up of 18 (range 6 to 105) months, 30 patients had preserved anal function. Twenty-one of the 22 patients who had ulcerative colitis retained anal function, but the functional outcome was not satisfactory in all cases. The median frequency of defecation per 24 hours was 9.6 times, but the range was considerable, from 4 to 35. Urgency was common and was constantly present in four patients and intermittent in 14. The quality of life was reported as good or excellent by 17 patients and fair or poor by 13. Despite disappointing function in some patients, it is clear that major surgical revision can result in worthwhile salvage in many.
Others, however, have reported poorer results. In a series of 114 patients who underwent abdominal salvage surgery for various reasons after RPC, 29 had procedures for intra-abdominal sepsis. These included drainage of abscess (three patients), diverting ileostomy (18), revision of the pouch (six) and primary closure of fistula (four). Of the 29 patients, 17 still had an ileostomy at the time of assessment, and in 10, the pouch had been removed. Only 10 had satisfactory anal function. The authors showed, importantly, that failure continues with the passage of time; at 2 years, 34 procedures had failed, and at 5 years, the probability of remaining free of pouch excision was 75%.
A similar experience was reported in 131 patients who developed early sepsis out of a total of 706 who had RPC for ulcerative colitis (494) and polyposis (212). The occurrence of early sepsis conferred a higher chance of cumulative failure compared with that in patients who did not develop early sepsis. Furthermore, failure after attempted salvage rose from 20% at 3 years to 40% at 10 years. Of the 131 patients followed for 51 (interquartile range 31 to 96) months, sepsis was caused by fistulation in 76% of cases, anastomotic separation in 15% of cases, and abscess formation alongside the pouch in 10% of cases. The authors classified the site of fistulation into three levels: level 1 (upper pouch) in 19% of cases, level 2 (lower pouch, rectal cuff) in 31% of cases, and level 3 (ileoanal anastomosis) in 50% of cases. Sepsis was treated conservatively in 24 cases (18%), by minor surgery in 33 cases (25%), and by major surgery in 74 cases (56%). As might be expected, the failure rate was higher after major (47%) than after minor (6%) surgery. Overall, failure was related to sepsis at level 3, the presence of a pouch–vaginal fistula (43%), an original diagnosis of ulcerative colitis, and the number of salvage procedures. It was also cumulative with time, even after salvage intervention.
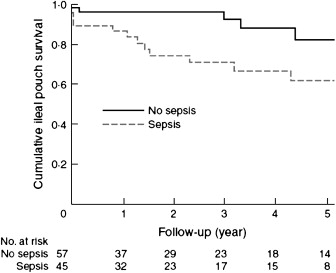
The largest series of abdominal salvage surgery published to date included 112 patients, with the following original pathology: ulcerative colitis (n = 86), indeterminate colitis (n = 11), familial adenomatous polyposis (n = 10), and other conditions (n = 5). At a median follow-up of 46 (range 1 to 147) months, 24 (21%) patients experienced pouch failure, the incidence of which increased with time. The pouch failed in all patients who had Crohn’s disease. Successful salvage at 5 years was associated with a nonseptic (85%) rather than a septic (61%) indication ( P = .016) as shown in Fig. 1 . Frequency of nighttime defecation and fecal urgency improved after salvage surgery.