HISTORICAL PERSPECTIVE
In the early days of hemodialysis, long (8-hour) dialysis was necessary as the dialysis technique was inefficient (5–7). Improving patient well-being with more than one or two dialysis sessions per week led to the adoption of the current standard of the thrice-weekly dialysis regimen. Improvement in the dialysis efficiency led to shorter hemodialysis sessions.
Perseverance with the original long (8-hour) thrice-weekly regimen in Tassin, France, and some other centers for more than 30 years, was associated with impressive patient outcomes and supported the notion that long dialysis was beneficial irrespective of the dialysis dose (8), an idea not clearly supported by the NCDS study (9). Long overnight hemodialysis (nocturnal hemodialysis) three times a week at home is credited to Shaldon (10). Long intermittent hemodialysis is financially attractive in comparison to daily hemodialysis, and therefore, recently, there has been an increased interest in its utilization at home or in the dialysis centers (11,12).
Home hemodialysis was necessary in the early dialysis days as it was less costly. More than 70% of dialyses in Seattle in the late 1960s was performed at home (5). Payment for dialysis with public funds, availability of hemodialysis close to the patients’ home, inception of continuous ambulatory peritoneal dialysis (CAPD), and acceptance of dialysis for sicker patients unable to be trained led to the decline of home hemodialysis. Regional or national differences in the dialysis modality distribution are often striking and can be explained by financial, geographic, and cultural factors. For example, despite some decline, home hemodialysis has been more popular in Australia and New Zealand (13). The high incidence of CAPD technique failure and reports of improved outcomes with long and/or frequent hemodialysis rekindled the interest in home hemodialysis, although there is a recent resurgence of PD in the United States (14).
The use of daily hemodialysis was reported in the 1960s first by DePalma (15,16) followed by others. Despite better patient satisfaction, blood pressure (BP) control, and anemia improvement, the initial attempts failed due to financial constraints. The published positive outcomes from the use of short daily hemodialysis by a small number of centers in Italy led by Buoncristiani and others (17–19), the advent of quotidian nocturnal hemodialysis (20), as well as interest by industry inspired renewed focus on daily hemodialysis.
Although nocturnal hemodialysis thrice weekly at home was used by Shaldon (10), the combination of long and frequent hemodialysis was reported by Uldall in 1994 (21).
Moreover, interest in alternative dialysis schedules was rekindled by the failure of both HEMO (3) and ADEMEX (22) studies to show a decrease in patient mortality rates by increasing the dose in either hemodialysis or PD, respectively.
More detailed historical aspects of home and frequent dialysis regimens are described elsewhere (5). Although most of the studies on daily and long hemodialysis were cohort studies, randomized controlled trials (RCTs) have been recently published. These include the Alberta trial on nocturnal hemodialysis (23) and the Frequent Hemodialysis Network (FHN) trials sponsored by the National Institutes of Health (NIH) (24,25).
Dialysis Prescription/Technical Aspects
Short, daily hemodialysis is characterized by dialysis performed for 1.5 to 3.0 hours, 5 to 7 days per week. There are calls for at least 3-hour short daily hemodialysis as it is characterized by better phosphate control (26). High blood and dialysate flows are used, aiming for the highest dialysis dose possible. Dialysate composition is similar to conventional hemodialysis. It is done either in the dialysis facility or at home.
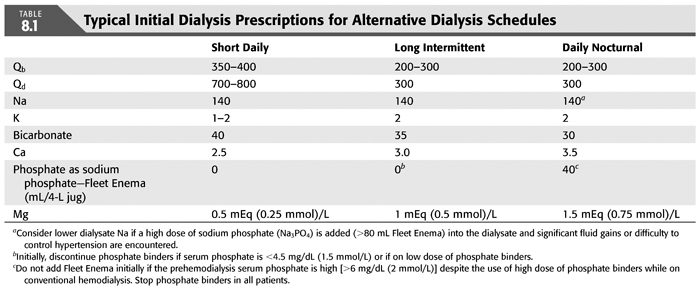
Daily (quotidian) nocturnal hemodialysis is performed 5 to 7 days per week (typically 6) during night sleep at home for an average of 8 hours. It is done by the patient or by a helper. Similarly, intermittent nocturnal hemodialysis occurs thrice weekly at the facility or at home (usually every other night). Facility-based nocturnal hemodialysis is typically performed by the dialysis staff. Blood flow is low on long hemodialysis (as a rule 200 to 300 mL/min and as low as 100 mL/min in children), whereas a typical dialysate flow is 300 mL/min. Lower dialysate volume is used by the NxStage machine. In the case of the daily nocturnal hemodialysis, the dialysate contains lower bicarbonate [typical: 30 mEq (mmol)/L] and higher calcium concentration [typical: 3.0 to 3.5 mEq (1.5 to 1.75 mmol)/L] than conventional hemodialysis (TABLE 8.1). A less significant deviation from the usual concentrate composition of the conventional hemodialysis is followed in the intermittent form. In more than 50% of patients on quotidian and less than 20% on the intermittent form, the dialysate contains a sodium phosphate additive (e.g., Fleet Enema 30 to 135 mL/4.5 L acid or bicarbonate concentrate) which corresponds to a final phosphate concentration of 1 to 3 mg/dL (0.3 to 0.9 mmol/L) (11,27,28). A higher calcium and phosphate concentration than described in the preceding text has been used during the so-called “hungry bone syndrome.”
Although all hemodialysis machines are acceptable for each of the stated regimens, several manufacturers have modified existing machines to be patient-friendly for use at home, and new machines aiming for the short daily or the long hemodialysis market have been produced. Some of the advantages include ease of use, portability, less reliance on water quality, and so on.
Anticoagulation during hemodialysis is similar irrespective of regimen. Danaparoid or argatroban have been used in cases of heparin-induced thrombocytopenia. Low molecular weight heparin has been employed for both as well as for longer dialysis. Tinzaparin has been used during nocturnal hemodialysis (29).
Water treatment at home is accomplished through the use of standard reverse osmosis systems with a carbon tank or the use of deionizer columns. The former provides for less expensive operation, and the latter is less noisy, more relevant to nightly hemodialysis. Occasionally, a water softener prior to water purification system has also been employed. The use of “ultrapure” dialysate is encouraged, although most of the published experience did not include the use of this enhancement.
Although dialyzer reuse has been practiced on home hemodialysis, it has been abandoned with the decrease in the cost of dialyzers (30). Remote monitoring of patients on nocturnal hemodialysis has been practiced by some centers (31–33), but it is considered optional. If BP monitoring without a cuff inflation and decrease in the cost of remote monitoring are achieved, remote monitoring could be attractive (33).
Dialysis Access
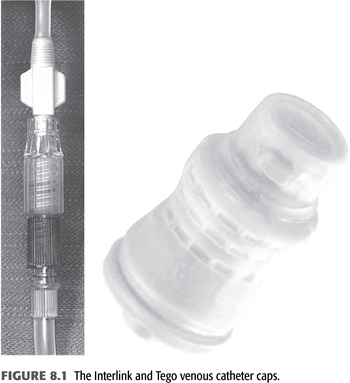
All types of accesses including permanent central venous catheters, arteriovenous (AV) fistulas, and grafts can be used with long or frequent hemodialysis either in-center or at home. Although fewer complications were reported in observational studies (34–36), the FHN trial reported increased incidence of vascular complications on daily hemodialysis (37). Lower access survival was also reported on long frequent home hemodialysis compared to long less frequent home dialysis (38). Dialysis catheter survival as well as infection rates were reported to be better on nocturnal hemodialysis when compared to conventional hemodialysis (39,40), but the infection rates were higher than when using AV accesses (41). Safety issues are very important for unattended nocturnal hemodialysis (42). The use of preperforated catheter caps during the dialysis procedure is highly recommended (InterLink, Tego) (FIGURE 8.1) (43). They prevent air emboli and bleeding from the “arterial limb” in the case of accidental disconnection.
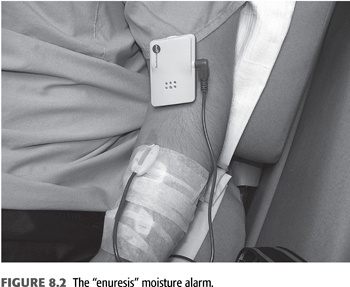
The so-called “buttonhole” technique has been used for fistula but not graft cannulation (44). Prospective studies on the outcomes when used at home are missing (44–48). Using this technique, the dialysis needle (usually “blunt,” noncutting) is inserted through the same cannulation track. A “buttonhole” is established using regular sharp needles for about 1 week. The use of the buttonhole technique has been associated with significantly higher rate of bacteremias. The putative advantages including less pain, familiarity with the site, and predictability of cannulation success have not been proved in RCTs. If used, attention should be given to proper technique and antisepsis during the “buttonhole” cannulation. Careful removal of the scab prior to the cannulation and local application of a small amount of antibiotic cream (e.g., mupirocin) after the completion of dialysis on the “buttonhole” has been advocated (47). Caution regarding the use of the buttonhole technique has been expressed by several authors (43,49). Proper secure taping of the dialysis needle is important for nocturnal hemodialysis. A single-needle system is preferable for long hemodialysis as it requires fewer cannulations and is safer in the case of accidental needle disconnection. The lower blood flow provided by the single-needle system is not a limitation for long hemodialysis. A moisture sensor taped on top of the needle insertion site is useful to awaken the patient in the event of blood extravasation during the dialysis procedure (31). An inexpensive nondisposable “enuresis alarm” is used by most centers in the interim until a dedicated product is developed (FIGURE 8.2). Commercially available sensors specifically designed for dialysis are available (50). Several inexpensive moisture sensors placed strategically on the floor in the vicinity of the dialysis machine alert the patient in case of either blood or dialysate leak (31).
 THEORY/KINETICS
THEORY/KINETICS
Small Molecule Removal
The use of Kt/V urea and urea reduction rate (URR) based on the NCDS study became popular as a measure of dialysis dose (51). These parameters are inadequate, however, in explaining the differences in outcomes between various modalities, between different schedules, or related to the presence of residual kidney function. The relatively positive clinical outcomes of patients on CAPD when compared to hemodialysis, despite the lower Kt/V offered by this method (weekly Kt/V 1.7 to 2.0 vs. 3.2, respectively), has been ascribed to the continuous nature of this treatment (52). Continuous (or frequent) dialysis can provide hemodynamic stability and therefore better cardiovascular tolerance and reduced fluctuation of physiologic parameters (53); better removal of larger molecules, which is time-dependent; and decreased exposure to the toxic peak levels of solutes which characterize intermittent dialysis. The most popular measure incorporating this effect of the dialysis frequency is the standard Kt/V (stdKt/V) proposed by Gotch (54,55). Similar weekly stdKt/V values offered by different regimens are expected to lead to similar clinical outcomes. Its calculation is based on the midweek predialysis serum blood urea nitrogen (BUN) (or the continuous BUN level in the case of native kidney function or CAPD). An stdKt/V of 2.0 corresponds to the Kidney Disease Outcomes Quality Initiative (KDOQI) dose guideline levels.
The usefulness of the stdKt/V in predicting clinical outcomes needs to be established. The use of stdKt/V increases the perceived value of high dialysis frequency, but this dose measure is not affected significantly by the increased dialysis length, as long intermittent dialysis has a smaller effect on the predialysis BUN levels. Therefore, based on this concept, the outcomes of long intermittent dialysis are expected to be inferior to the outcomes of short daily hemodialysis, which has not been established and may not be accurate. A single-pool Kt/V (spKt/V) of only about 0.53 is required daily to maintain the same weekly stdKt/V delivered by thrice-weekly hemodialysis when adhering to the KDOQI guideline dose of a spKt/V of 1.2 per dialysis session. Maintenance of the same length of weekly dialysis after the conversion to the daily regimen provides an stdKt/V of 2.5 to 3 (56). The spKt/V offered by daily nocturnal hemodialysis is much higher at about 1.8 to 2.5 per treatment, whereas the stdKt/V is 4 to 6 for the six times per week regimen (57). This concept of stdKt/V is utilized by the proponents of the NxStage machine. The prescription includes usually lower dialysate volume (about 25 L) with weekly stdKt/V similar to PD to achieve financial feasibility of daily hemodialysis.
Middle Molecule Removal
The evidence that higher larger molecule weight solute removal correlates with better clinical outcomes is supported by some studies (58–60). Patient outcomes correlated well with the length of dialysis, surrogate of middle molecule removal, in two studies from the Australian/New Zealand (61) and Dialysis Outcomes and Practice Pattern Study (DOPPS) registries (62).
As predicted, middle molecule removal is increased mainly by longer dialysis and less significantly by short daily hemodialysis. This was shown by mathematical modeling (63) as well as in clinical studies. Weekly β2-microglobulin removal increased fourfold from 127 to 585 mg after the conversion from conventional to quotidian nocturnal hemodialysis. Serum predialysis β2-microglobulin levels decreased from 27.2 to 13.7 mg/dL in 9 months (64). Advanced glycation end-product (AGE) levels decreased on daily hemodialysis (65) as did the levels of protein-bound solutes such as indole-3-acetic and acid indoxyl sulfate (66).
Phosphate Removal
Hyperphosphatemia has been considered a significant risk factor for both kidney osteodystrophy as well as cardiovascular disease and has been correlated to patient mortality (67). Despite the adequate phosphate clearance during dialysis, phosphate removal is limited by the slow intercompartmental movement of phosphate, resulting in low serum phosphate both during and in rebound posthemodialysis (68). The most significant parameter affecting phosphate removal is the length of dialysis. The effect of the dialysis regimens on phosphate control is therefore predictable. Short daily hemodialysis increases phosphate removal because phosphate removal is higher during the early part of dialysis when the blood to dialysate gradient is highest. This has been confirmed by measuring phosphate in spent dialysate (26,69). However, a 2-hour short daily hemodialysis has only a modest effect on serum phosphate as phosphate intake often increases with improving appetite. Significant improvement in phosphate control was found in studies when the dialysis time was extended to 3 hours (26,70). Daily nocturnal hemodialysis is effective in phosphate removal not only leading to elimination of the need for phosphate binders and unrestricted diet but even necessitating the addition of phosphate into the dialysate in order to avoid hypophosphatemia in 75% of the patients (TABLE 8.1) (31,71). The effect of intermittent nocturnal hemodialysis on phosphate removal is also significant, but some patients still needing binders while for others a phosphate additive into the dialysate is necessary (11). In this modality, the predialysis phosphate can be high while the posthemodialysis value can be in the hypophosphatemic range. The effectiveness of long intermittent hemodialysis in phosphate removal is higher than that of short daily hemodialysis (TABLE 8.2). The improvement in phosphate control was confirmed in the FHN in both daily and nocturnal trials (70) as well as the Alberta trial (72).

Patient Selection/Training and Utilization of the Alternative Dialysis Schedules
Patient selection and method utilization are affected by several factors. They include the local availability of the modality, finances, medical indications/contraindications, dialysis team biases, and patient/family choice. In turn, availability of the method depends on local expertise and financial factors.
The type of patients who is treated using the alternative dialysis schedules tend to follow a bimodal distribution. This includes patients who experience “technique failure” in their current modality and for whom an alternative dialysis method is used as a “rescue” treatment (73,74). Alternatively, other patients opt for these dialysis modalities motivated by a desire to improve their quality of life (QOL). The former group of patients tends to be switched either to short daily hemodialysis or intermittent nocturnal hemodialysis in the dialysis facility or daily nocturnal hemodialysis at home. Usual reasons for this “rescue” treatment include significant hemodynamic instability, cardiovascular disease, refractory hypertension, intra- and interdialytic symptoms, ascites, malnutrition, “failure to thrive,” or large body size. The second group tends to include younger patients who are more likely to dialyze at home. In the absence of comorbidities, it is often difficult to convince prevalent dialysis patients to convert to the alternative dialysis schedules especially in the form of home hemodialysis. Incident compared to prevalent dialysis patients are the more likely to elect to do home hemodialysis irrespective of the regimen. Interestingly, only 56% of the patients on conventional hemodialysis questioned would agree to come to the dialysis facility daily even if the benefits of the method were established (75). Conversely, it has been rare that patients who started on daily hemodialysis revert back to thrice-weekly hemodialysis. The age of patients opting for home hemodialysis is on average 10 years older than in center hemodialysis.
Contraindications for home hemodialysis include patient inability or lack of motivation to be trained in the absence of a suitable helper. Other contraindications include inadequate housing or difficulty with oral communication (including difficulty communicating in the prevalent language) necessary in case of an emergency in the absence of a helper at home. The presence of significant hemodynamic instability is an indication for daily nocturnal hemodialysis. Allergy to heparin is a relative contraindication to home nocturnal hemodialysis. Of course, alternative anticoagulants such as danaparoid or argatroban can be used.
Training for home hemodialysis typically lasts for 4 to 6 weeks and is usually done while on thrice-weekly hemodialysis. Self-care dialysis can be used as an interim phase as it allows for a longer training period. Beyond the basic aspects, the training usually includes blood sampling and spinning for laboratory tests, blood cultures, as well as infusion of intravenous antibiotics and iron preparations. In view of the hemodynamic stability offered by these regimens, the presence of a home helper has not been considered obligatory at least for the long form of dialysis, although it has been required in certain jurisdictions. Monthly laboratory tests and clinic visits every 2 to 3 months are the usual practice.
 OUTCOMES
OUTCOMES
Health Economics and Quality of Life
Health Economics
The cost of dialysis can be viewed from the multiple stakeholders’ perspectives. Stakeholders include the society at large, payers, dialysis facilities, members of the dialysis team affecting the patient’s decision (including health providers), patients themselves, and patients’ families. The cost/benefit ratio to the several stakeholders affects the utilization of the method. Dialysis costs are very high, challenging society’s willingness to pay. (TABLE 8.3)
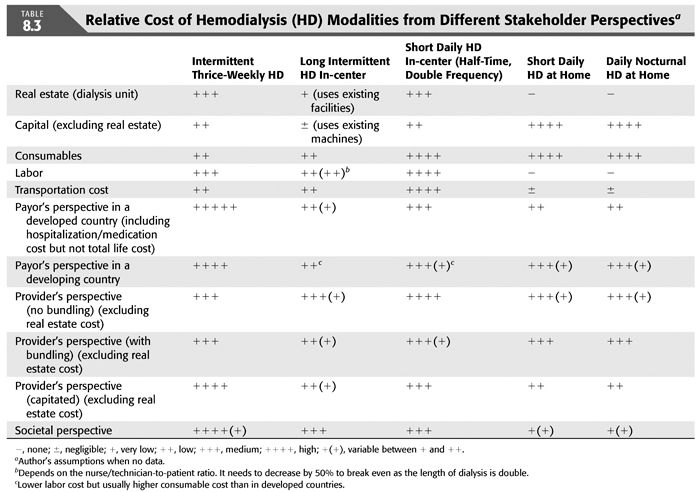
Some of the important fiscal elements of the alternative dialysis schemes, which contribute to the financial picture, are as follows:
a. Home dialysis is associated with increased capital costs (one machine per patient) but decreased labor costs.
b. Daily dialysis incurs high consumable costs (daily regimen).
c. In-center short hemodialysis may decrease the patient capacity of the dialysis unit due to frequent machine preparation with possible time lost, which consequently affects revenue (76).
d. Long dialysis potentially increases quality with negligible increase in consumable cost (“better bang for the buck”).
e. Savings from the putative improved patient outcomes can be derived from both decreased hospitalization rate and length, as well as lower medication utilization.
f. Higher cost to the payer is incurred from possible increased patient survival.
g. Societal, patient, and patient’s family benefit can be derived from the improvement of the vocational rehabilitation of the patient with lower utilization of societal services.
h. Possible decreased use of injectables on the alternative dialysis schedule regimens can harm (no bundling) or benefit the dialysis provider’s finances (with bundling).
i. Increased cost of dialysis burdens the dialysis provider, whereas decreased hospitalization rates benefit the payer. In a capitated system, it benefits the provider.
j. Increased cost of home utilities (water and electricity) from home hemodialysis is usually incurred by the patient.
k. Transportation cost reduction, by using home hemodialysis, benefit the patient or the publically supported transit system.
The differential cost and benefit allocation among the stakeholders as it is dictated by the structure of the system is critically important for the adoption of these regimens. At the international level, the consumable/labor cost ratio in different countries also has a major impact on the potential adoption of these methods irrespective of the clinical benefits. In a country with high consumable to labor cost ratio daily hemodialysis is not financially attractive.
Several published studies have addressed the costs of quotidian home hemodialysis (77–79). These studies are either retrospective (80,81) or prospective (78,82–84), and although they are controlled, they are not randomized with the exception of the Alberta study (78). All these studies showed that although the cost of capital and consumables increases on daily (short and nocturnal), the decrease in labor cost offsets the increased expense as long as the treatment is delivered at home. In-center daily hemodialysis is clearly more expensive. Although in a retrospective analysis the decrease in hospitalization offsets the increased cost of the in-center short daily hemodialysis (80), this may apply only to patients with increased morbidity who require frequent hospital admissions (73).
It is reasonable to speculate that home intermittent nocturnal hemodialysis is the least expensive of the alternative schedule modalities. There are no studies published on the cost of in-center intermittent hemodialysis. In this modality, although the cost of consumables is probably similar to conventional hemodialysis, the labor cost has not been quantitated in a published study. Higher labor cost related to the longer dialysis could be offset by the lower staff to patient ratio related to the hemodynamic stability of the patients.
Several studies suggested that daily hemodialysis is associated with fewer hospital admissions and reduced costs for hospitalization, as well as lower cost of medications including erythropoiesis-stimulating agent (ESA), cardiovascular medications, and phosphate binders (on nocturnal hemodialysis) (77,83,85). In all of the studies, the total cost of health care for in-center conventional hemodialysis was higher than for quotidian hemodialysis, with cost savings estimated to be between $5,000 and $10,000 per patient-year (80,82–85). Importantly, home programs were less expensive even when patient-specific savings (such as reductions in hospitalization) were excluded. These results need to be confirmed in more properly designed studies.
Quality of Life
Several approaches to the measurement of the QOL on the alternative dialysis schedules have been adopted. They include dialysis-independent measures, dialysis-dependent measures, and utility scores. Although most studies were not randomized, two RCTs have been published.
Improvements in QOL have been reported on several elements of Kidney Disease Quality of Life (KDQOL) (73,80,86–89). Patient testimonials has been very positive (90). Minutes to recovery after a hemodialysis session were shorter after daily hemodialysis (91).
Utility scores calculating quality-adjusted life years (QALYs) were published in both short daily and nocturnal hemodialysis (89,92). The utility instruments used included the willingness to pay, time trade-off, standard gamble technique (92), and Health Utility Index tool (83). Daily nocturnal hemodialysis was an economically “dominant” modality as it improved QOL while it decreased cost (92,93). There were no negative effects on QOL measures after the conversion from conventional to in-center intermittent nocturnal hemodialysis (94). The daily hemodialysis arm of the FHN trial demonstrated a significant improvement of the composite end point of death and physical component of the KDQOL (24). The nocturnal arm of the study failed to show improvement in the similar index (25). The Alberta study did not find improvement in the QOL in the patients randomized to nocturnal hemodialysis using the EuroQol five dimensions questionnaire (EQ-5D) index scores (p = 0.06) but showed improvement using the visual analog of the same index as well as several kidney disease-specific subscores (95).
Cognitive Function
There is some evidence, in one observational study, of improvement in the cognitive function of patients after their conversion to quotidian nocturnal hemodialysis (96). Improvement in cognitive function, as well as electroencephalogram (EEG) tracing, was also seen on short daily hemodialysis (97). Self-reported general mental health improved on daily hemodialysis in the FHN trial, but the depressive symptoms did not change significantly (98). The FHN trial did not show any improvement in cognition on frequent dialysis (99).
Cardiovascular Effects
Blood pressure, left ventricular geometry, and left ventricular function. Improved BP control has been reported consistently in all forms of alternative dialysis schedules (15,100). This includes short daily hemodialysis (19,73
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


