Lichtenstein-based Groin Hernia Repair
Steven D. Schwaitzberg
Introduction
There are a variety of open hernia repair techniques that the surgeon can choose from today. For the last 20 years the majority of surgeons have employed some form of mesh augmented repair for the reconstruction of the groin. One of the key early adopters of mesh augmented hernia repair was Irving Lichtenstein who along with Alex Shulman and Parviz Amid developed this method of hernia repair. This technique followed in the footsteps of the earliest mesh augmented repairs performed by Francis Usher who used a piece of polypropylene mesh to create a cuff around the conjoined tendon before suturing it to the inguinal ligament. The Lichtenstein repair came into existence with the recognition that classic Bassini or McVay (Cooper’s ligament) type procedures were associated with higher than acceptable long-term recurrence rates even when relaxing incisions in the anterior rectus fascia were employed. This repair requires the surgeon to define precise anatomic landmarks. A tension-free repair is then created utilizing a modest size polypropylene mesh to reconstruct the floor of the inguinal canal which continues laterally with a keyhole in the mesh to accommodate this spermatic cord thus reconstructing the internal ring. This repair can be mastered with a relatively shallow learning curve and is associated with low recurrence rates and complications.
The Lichtenstein hernia repair is indicated for initial mild to moderate, direct or indirect inguinal as well as femoral hernias in both men and women. It can also be deployed in patients with recurrent groin hernias particularly when an alternate technique was used at the initial repair. Surgeons who choose this technique should be prepared to make the appropriate technique modifications that are based on the specific type of hernia encountered.
Patient Preparation
This technique can be performed under local, regional, or general anesthesia. One cited advantage of performing this technique in awake patients is the opportunity to ask the patient to cough and assess the repair for weakness. The arms may remain outstretched or can be tucked on the basis of the patient’s body habitus and the surgeon’s preference. In routine cases, a urinary catheter is not necessary. Sufficient bladder decompression is achieved if the patient is able to urinate immediately prior to the procedure and a consensus is reached with anesthesia that minimal amounts of intravenous fluids will be administered intraoperatively. The lower abdomen and groin are prepped consistent with the surgeon’s preference. Many surgeons prefer the use of a plastic barrier draped over the skin to prevent contact of the mesh with the skin. Unless the patient has a large intrascrotal hernia, the scrotum does not need to be draped into the operative field. The use of the plastic barrier drape makes it possible to easily include the umbilicus, the anterior superior iliac spine (ASIS), and the pubic tubercles into the operative field. A single dose of first generation cephalosporin is commonly administered for prophylaxis.
Incision
For most patients, a properly placed incision need not be much larger than 5 cm. There are two basic incision types for this procedure, transverse or oblique (Fig. 2.1). Transverse incisions have the advantage of being made in the lines of Langer which imparts a theoretical cosmetic advantage. The oblique incision is essentially made over the distance from the internal to the external ring which in theory allows for the smallest length of incision needed. The oblique incision is prepared by marking a line from the ASIS to the pubic tubercle. A 5 to 7 cm incision is then made parallel 1 cm cephalad to the previously marked line which begins medially 2 cm lateral to the pubic tubercle and continued for the selected distance. Given the general laxity of the skin in this region it can easily be shifted in order to visualize all of the required structures to be dissected. Once the skin is incised, the incision is carried down to the external oblique fascia sharply or by cautery. It is common to encounter a subcutaneous vein requiring ligation in the lateral aspect of the wound. The external oblique should be exposed from the external ring 10 cm laterally and at least 5 cm in width. This will facilitate closure at the end of the case.
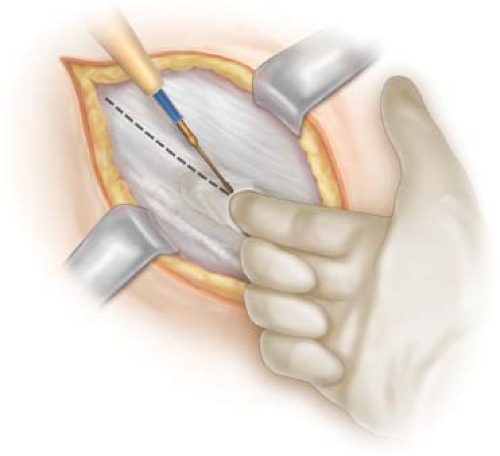
Dissection
The true dissection commences at opening the external oblique fascia in line with its fibers (Fig. 2.2). After identifying the pubic tubercle the surgeon or assistant can place their finger into the external ring just under the external oblique fascia. The fascia is then opened medially to laterally with electrocautery using the surgeon’s finger to protect the underlying structures. Alternatively, one blade of the Metzenbaum scissors is placed under the external oblique aponeurosis and the scissors are “pushed” in the direction of the fibers opening the layer. This guarantees that the external ring will be completely opened which is a requirement for adequate exposure. The external oblique should be open for at least 10 cm which will allow for complete exposure of the internal ring as well as a few centimeters laterally. Cephalad and caudad flaps of the external oblique aponeurosis are developed from the pubic tubercle for the entire length of the incision. The cephalad extent of the dissection should expose the conjoined tendon and rectus sheath. The caudad flap dissection should be continued until the inguinal ligament (Poupart) is clearly demonstrated. Self-retaining retractors are used to maintain the exposure. At this point the course of the ilioinguinal nerve should be discerned. At this point either the nerve is carefully mobilized and retracted behind the cephalad flap of the external oblique aponeurosis or some surgeons prefer to resect the nerve and allow the proximal end to retract into the internal oblique muscle fiber. The second option is more commonly employed in older patients. Not all patients experienced numbness when this resection maneuver is performed because of overlapping innervation. If the nerve is resected, neuroma is possible, inguinodynia is avoided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree