■ Detection of early-stage disease may be enhanced by magnetic resonance (MR) with cholangiopancreatography (MRCP) with or without secretin administration. Morphologic changes in the pancreatic duct and hydrodynamic-significant strictures may be evident on these images.12
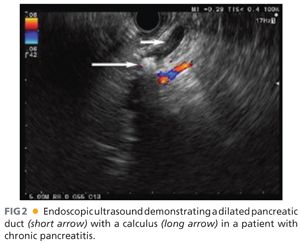
■ Endoscopic ultrasound (EUS) with or without functional testing by administration of secretin may aid in the diagnosis of early fibrosis in chronic pancreatitis (FIG 2). EUS has a sensitivity of 84% and a specificity of 100%, correlating with histology for chronic pancreatitis.13 Furthermore, EUS is advantageous when mass lesions are present in chronic pancreatitis because EUS-guided biopsy is the most reliable method of confirming malignancy.
■ Imaging of the pancreatic duct prior to surgical intervention is essential because all strictures and intraductal calculi must be addressed by the operative approach. Ductal anatomy can be delineated by MRCP or endoscopic retrograde cholangiopancreatography (ERCP). ERCP is often performed in the context of pancreatic duct stenting as endotherapy often precedes operative management.
SURGICAL MANAGEMENT
■ Operative management of chronic pancreatitis by lateral pancreaticojejunostomy with or without pancreatic head resection is indicated in patients with disabling abdominal pain, weight loss, and evidence of pancreatic duct obstruction.14 Morphologic characteristics are associated with outcomes. An excellent response to pancreatic head resection with pancreaticojejunostomy is most likely in the setting of an enlarged head of the pancreas and a distally dilated pancreatic duct.15
Preoperative Planning
■ These patients are often afflicted with a chronic disease and have lacked regular medical care, thus a thorough evaluation of the patient prior to pancreatic head resection and duct drainage is essential.
■ Patients should be alcohol-free for at least 6 months and enrolled in an alcohol cessation program with aftercare. Ideally, cigarette smoking would also be stopped prior to an operation, although this is difficult for most patients.
■ Specific attention should be paid to the nutritional status of patients with chronic pancreatitis because they often meet criteria for severe protein and caloric malnutrition. Fat-soluble vitamin deficiency should also be considered. If malnutrition is evident, a nasojejunal feeding tube should be placed with the delivery of enteral feeds with pancreatic enzyme supplementation prior to operative intervention. Additional protein supplementation may also be necessary. Generally, 2 to 4 weeks of enteral nutrition prior to an operation will place the patient in an anabolic state.
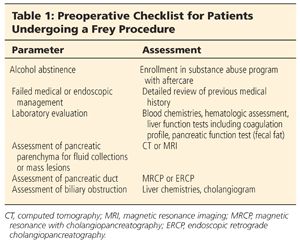
■ Table 1 highlights the preoperative checklist of patients who are candidates for a Frey procedure with longitudinal drainage of the pancreatic duct.
Positioning
■ The patient is placed on the operating room table in a supine position. Because the risk for blood loss is moderately high, at least two large-bore intravenous cannulas should be established or a central line should be placed. Arterial monitoring is recommended for patients with comorbidities.
TECHNIQUES
EXPOSURE OF THE PANCREAS
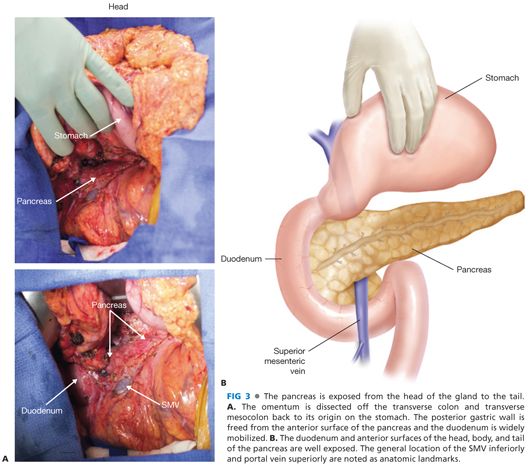
■ A midline celiotomy is created to allow adequate exposure of the upper abdomen. After a thorough exploration of the abdomen, the pancreas is exposed by elevating the omentum off the transverse colon and pancreatic head back to the origin on the stomach. The hepatic flexure is mobilized as necessary and the duodenum is widely Kocherized. Frequently, the posterior wall of the stomach is adherent to the pancreas and must be dissected free. At the inferior border of the pancreatic neck, the right gastroepiploic vein is circumferentially dissected and divided at the insertion into the superior mesenteric vein (SMV). The distal stomach and proximal duodenum are mobilized from the head of the pancreas to allow adequate exposure for resection of the pancreatic head. The SMV should not be dissected free from the posterior surface of the pancreas for fear of venous injury. These maneuvers should provide wide exposure of the pancreas from the duodenum to the tail of the pancreas (FIG 3).
PANCREATIC HEAD RESECTION
■ The gastroduodenal artery is identified at the superior border of the pancreas and ligated with a figure-of-eight 4-0 Prolene suture. The resection of the pancreatic head should be mapped with care to avoid injury to the SMV. The pancreatic head is generously resected, leaving only a thin rim (3 to 5 mm) of tissue along the duodenal wall and posteriorly (FIG 4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








