■ Use of self-retaining retractors facilitates exposure of the terminal bile duct and the first and second portions of the duodenum (FIG 2).

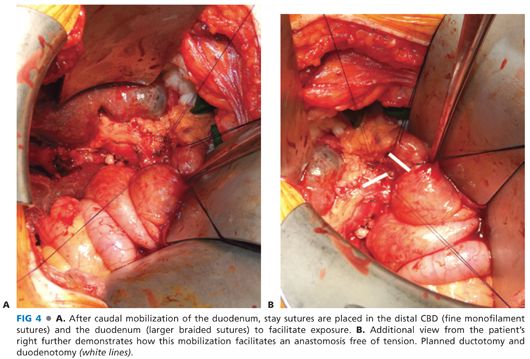
■ An extensive Kocher maneuver is performed to optimally mobilize the duodenum. This mobilization is a critical step for the success of a tension-free anastomosis. The pancreatic head and terminal bile duct are palpated and examined to assess for extent of disease and unexpected findings.
■ If the gallbladder remains in place, a cholecystectomy is performed (FIG 3).
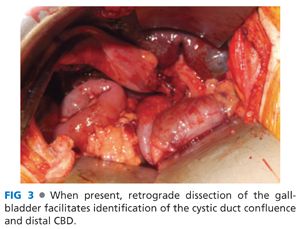
■ The porta hepatis is examined and the CBD clearly identified for the course of greater than 3 cm along its anterior wall. In cases with significant inflammation and fibrosis, the anatomy can be distorted. Palpation of the hepatic artery can be helpful in orientation, as can palpation of an intraductal biliary stent or aspiration of bile with a fine needle and syringe.
■ Incision of the peritoneum at the cephalad aspect of the first portion of the duodenum can facilitate the establishment of a plane between the posterior wall of the duodenum and the anterior wall of the CBD, providing additional length and improving the proximity of the planned ductotomy and duodenotomy sites, thus reducing potential tension on the anastomosis (FIG 4).
Choledochoduodenal Anastomosis
■ Identification of the CBD is confirmed by aspiration with a 21-gauge needle.
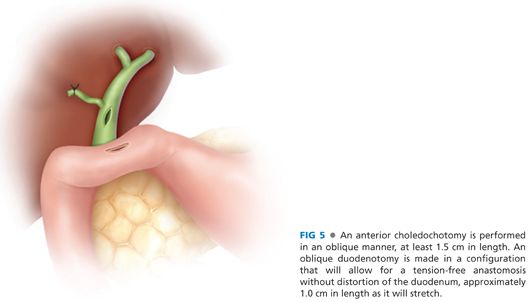
■ An anterior ductotomy is made sharply, typically with a no. 11 blade at the site of the needle aspiration, large enough to permit entrance into the duct with the tip of a fine hemostat. An anterior longitudinal choledochotomy is then extended with scissors or electrocautery for 1.5 cm in length. The ductotomy is made on the distal CBD as close as safely possible to the duodenum. Arterial bleeding on the distal ductotomy means “far enough.”
■ The distal CBD and common hepatic duct should be irrigated with an 8-Fr catheter to clear the duct of stones and sludge. If ductal lithiasis is present, choledochoscopy should be undertaken to confirm clearance of the duct of stones. Residual stones may require balloon catheter or basket extraction.
■ When cavernous transformation of the portal vein is present, the venous network surrounding the common duct will require a combination of suture ligation, coaptive electrocautery, and argon beam coagulation to achieve hemostasis.
■ The mobility of duodenum is assessed to determine where an anastomosis will most suitably lie without tension. A duodenotomy is then made with electrocautery, with cutting current in the postbulbar duodenum. The angle of the duodenotomy will vary from patient to patient, depending on the underlying disorder and variation from normal anatomy. In pancreatitis, the mobility of the duodenum varies with the underlying peripancreatic fibrosis so the location of the duodenotomy will vary accordingly. The duodenotomy is usually an oblique incision, with the goal of a comfortable anastomosis without distortion of the duodenal flow. The duodenotomy should be cut at a length of about 1.0 cm as it will always stretch more than expected (FIG 5).
■ If a preoperative prograde or retrograde stent has been placed, it may be prudent to leave it in place to serve as a postoperative stent, particularly in the difficult anastomosis in the presence of severe peripancreatic fibrosis, recognizing the risk of stent-induced postoperative biliary sepsis related to the sialomucin stent biofilm harboring gram-negative bacteria.
■ A single layer of interrupted sutures with fine 4-0 or 5-0 monofilament absorbable suture is used for this anastomosis. Full-thickness corner sutures are placed through the duodenum and then the bile duct at either end of the anastomosis such that the tails are outside the lumen. They are marked with a hemostat and act for exposure and for conceptual planning (FIG 6).

■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








