■ Enhanced hepatic MRI is an equivalent alternative.
■ Tissue sampling with core biopsy by ultrasound or CT guidance can be useful to make or confirm a diagnosis.
■ Additional diagnostic studies that are necessary prior to operation are basic labs, including a hepatic function panel and coagulation studies. A complete blood count including a platelet count is important to help detect advanced portal hypertension if the patient has cirrhosis. If disease-specific tumor markers are elevated, they are helpful to confirm a diagnosis as well as to follow patients during treatment.
SURGICAL MANAGEMENT AND OPERATIVE TECHNIQUE
■ There are several advantages of laparoscopic liver resection when compared to an open technique. These include decreased blood loss, less postoperative pain, quicker return to diet, and a shorter length of stay.1 These advantages have been demonstrated in case-controlled studies. Additionally, oncologic outcomes (margins, survival) are not compromised when laparoscopic technique is used for patients with hepatocellular carcinoma and metastatic colorectal cancer.2–4
■ During the World Consensus Conference on Laparoscopic Surgery in 2008, the international position on laparoscopic liver surgery was created—this should be used as a guide to determine which patients are eligible for minimally invasive hepatic resection.5 This statement recommends surgery with minimally invasive technique for patients with a single lesion of 5 cm or less located in segments 2 to 6. It suggests that major liver resection can be performed with minimally invasive technique but only by those experienced both with liver surgery as well as minimally invasive liver resection. Some surgeons in high-volume centers may choose to operate beyond these criteria in certain settings. Importantly, the consensus conference suggests that the surgeon should be facile with minimally invasive technique, including the skill of intracorporeal suturing should bleeding become an issue.
■ The decision to use hand-assisted versus pure laparoscopic technique is surgeon specific and mostly depends on comfort with either technique. As our own experience in laparoscopic hepatectomy has grown, so has our comfort with performing anatomic hepatic resection in a pure laparoscopic manner. When comparing pure laparoscopic technique to hand-assisted or hybrid technique in 113 patients undergoing anatomic liver resection, we found similar results for estimated blood loss and complications; however, interestingly, shorter operative times were noted in the pure laparoscopic group (188 minutes vs. 264 minutes for the pure vs. hand-assisted technique, P < .05).6
■ Consideration of the background liver is important to help decide which patients are appropriate for resection—up to 80% of a healthy liver in a relatively healthy patient can be resected without major consequence. This percentage decreases if the liver is cirrhotic.
■ The technique of minimally invasive right hepatectomy is, as intended, the same as for open surgery except minimally invasive equipment is used.
■ Two surgeons who are experienced in hepatobiliary and minimally invasive surgery are appropriate for these cases. An assistant to hold the camera is optimal, thus allowing both hands of both surgeons to be free.
TECHNIQUES
HAND-ASSISTED LAPAROSCOPIC RIGHT HEPATECTOMY
■ The patient is positioned supine with the arms tucked. Padded barriers are secured at the patient’s feet to prevent sliding with the anticipated use of steep reverse Trendelenburg during the case.
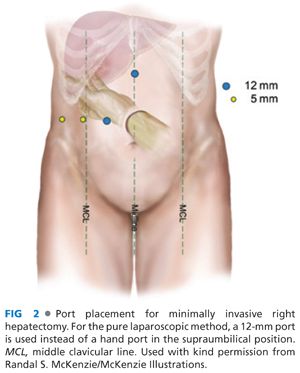
■ Access is gained to the abdominal cavity via a 5-mm port ideally in the left upper quadrant (LUQ), and pneumoperitoneum of 12 mmHg is created. Additional ports are placed using a 5-mm 30-degree scope for visualization (FIG 2). These ports include an 8-cm hand access site in the supraumbilical position. Two 12-mm ports are placed in the subxiphoid and right paramedian position, and two 5-mm ports are placed in right subcostal positions. The camera is switched to a 10-mm 30-degree scope in the right paramedian port.
■ The lesion is identified.
■ Standing at the patient’s left, the surgeon places his or her nondominant hand through the hand access device.
■ The round and falciform ligaments are divided using a sealing device, exposing the anterior surface of the hepatic veins.
■ The ligamentous attachments of the right liver are dissected. With the patient in reverse Trendelenburg position and with the right side up, the gallbladder fundus is retracted superiorly via a grasper in the LUQ port. The right lobe of the liver is retracted anteriorly using a closed grasper in the subxiphoid port. With a hand retracting the colon inferiorly, the hepatic flexure is dissected using a cautery device. The colon is reflected inferiorly. Attachments to the duodenum are dissected from the liver as necessary. Using hand assistance for ligament exposure, the right triangular and coronary ligaments are dissected up to the right hepatic vein (RHV)/inferior vena cava (IVC), also using a sealing device (FIG 3).

■ Laparoscopic ultrasound of the liver is performed via the 12-mm subxiphoid port to confirm anatomy and ensure that the procedure will include the pathology that is anticipated.
■ The IVC is dissected (FIG 4A,B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








