Fig. 21.1
Theater organization for laparoscopic low anterior resection
The surgeon works from the patient’s right with an assistant to the left of the surgeon and on the left side of the patient. We prefer to use two monitors on the left side of the patient; one is placed at hip level for optimal surgeon’s view and a second one opposite to the first assistant. A third monitor in the right side of the patient may be useful to the second assistant. The operating nurse and instrument table should be on the right side, close to the foot of the patient.
The pneumoperitoneum is made by a Veress needle inserted in a periumbilical location or in the left upper quadrant (Palmer’s point). The abdomen is insufflated with CO2 gas. When a 12 mmHg pressure is obtained, a 10/12-mm port is inserted at the level of the umbilicus and a 30° camera is introduced. Two 5-mm trocars are introduced in the right side of the abdomen and in the left lower quadrant. Finally, a 5/12-mm trocar is introduced in right lower abdominal region (Fig. 21.2). Additional trocars can be introduced as needed. Care is needed during trocar placement to avoid injury to the inferior epigastric vessels.
Fig. 21.2
Trocar positions for the abdominal approach. The blue 5-mm trocar is used if a splenic flexure approach is necessary
First, the surgeon should explore the abdominal cavity laparoscopically looking for tumor implants or liver metastasis. A steep Trendelenburg and right side down position of the table is adopted and the small bowel is moved to the right upper quadrant. We favor a medial-to-lateral approach to the superior rectal vessels, however there are some situations in which early mobilization of the lateral attachments of the sigmoid colon and a lateral to medial approach may be advantageous.
We use the 5-mm LigaSure device (Covidien) as a hemostatic device and a monopolar energy device (e.g., hook) to perform the surgery. A gentle skyward traction of the sigmoid colon is made by the assistant with a grasping forceps so the inferior mesenteric vessels are retracted. In general, grasping the colon should be avoided to prevent bowel injury. The surgeon incises the peritoneum at the base of the sigmoid mesentery over the right iliac vessels and the space between the superior rectal vessels and the retroperitoneum is bluntly dissected. The inferior mesenteric artery and vein are dissected separately and the left ureter is localized over the left common iliac artery (Fig. 21.3). The gonadal vessels should also be identified lateral to the ureter before ligating the mesenteric vessels. The inferior mesenteric artery is divided 1 cm from its origin using clips, a laparoscopic linear stapler, or simply with the LigaSure device (Fig. 21.4). The inferior mesenteric vein is found next to the pancreas and similarly divided. The mesentery of the descending and sigmoid colon is released from medial to lateral all the way to the line of Toldt (Fig. 21.5). Care should be taken to avoid injuries to the mesenteric arcades to guarantee a correct blood supply to the descending colon. Gauze is used for hemostasis and to protect the ureter and gonadal vessels and is left as a marking reference to assist in the takedown of the lateral attachments from the left side. The assistant surgeon gently pulls the sigmoid colon medially to expose the peritoneal attachment in the left gutter. The peritoneum is incised from the pelvic brim to the splenic flexure.
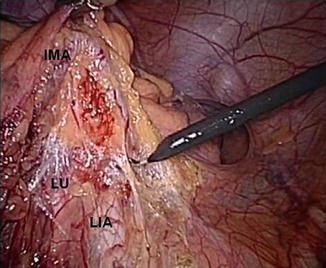
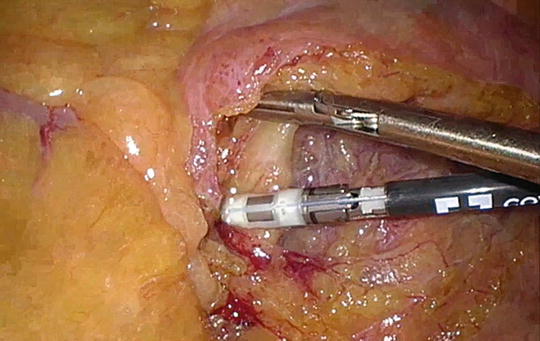
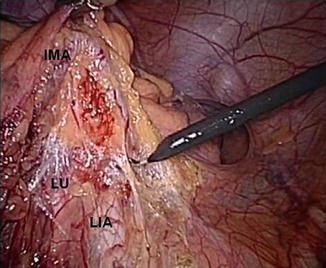
Fig. 21.3
Laparoscopic view of the pelvis. Traction of the inferior mesenteric artery (IMA) allows the correct visualization of the left ureter (LU) and left iliac artery (LIA)
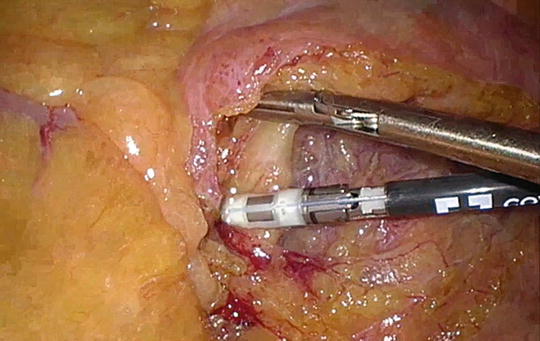
Fig. 21.4
Division of the inferior mesenteric artery with the LigaSure device
Fig. 21.5
Schematic of the resection
Now, the attention is turned to the pelvis to begin the rectal surgery. By pulling the rectum upward toward the anterior abdominal wall, the surgeon separates the mesorectum from the promontory opening the areolar avascular space. At this point the surgeon can bluntly separate the mesorectal fascia from the presacral fascia propia by pushing the mesorectum anteriorly (Fig. 21.6). As such, the hypogastric nerves and, more distally, the pelvic nerve plexus are exposed and protected from potential injury. The dissection should be meticulous to avoid injuring the sacral venous plexus.


Fig. 21.6
Dissection of the mesorectum in an avascular presacral plane. The instrument is holding the rectum up against the anterior abdominal wall
The dissection is then continued laterally, opening the peritoneum all the way to the anterior peritoneal reflection in the cul-de-sac and dividing the lateral ligaments. The position of both ureters and hypogastric nerves should be checked at this point and preserved. Finally, the surgeon incises the peritoneum of the rectovesical pouch in men or the rectovaginal pouch in women, exposing Denonvilliers’ fascia. The dissection is continued, alternating right and left side, until the distal rectum is completely freed taking care to preserve the neurovascular bundles. Once the rectosacral ligament is incised at the level of the fourth sacral vertebra, the dissection meets the levator ani muscle and the pelvic floor. When a TME is performed, the rectum is divided at the level of the pelvic floor, ideally leaving a margin of at least 2 cm distal to the tumor. An articulating linear stapler is commonly used to divide the rectum (Fig. 21.7). In very low rectal tumors, an intersphincteric resection is necessary using a perineal transanal approach.
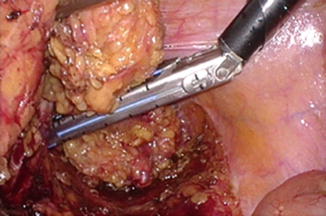
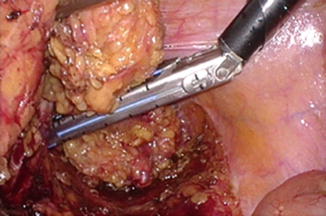
Fig. 21.7
Distal resection of the low rectum with an articulating laparoscopic linear stapler
Anastomotic Technique
Depending on the patient and the location of the tumor, the anastomosis can be performed mechanically or hand-sewn.
Mechanical Anastomosis
For middle or high rectal tumors we exteriorize the rectum and sigmoid colon with a Pfannenstiel incision. The specimen is drawn out of the peritoneal cavity after protecting the wound (e.g., using a plastic ring drape) and divided proximally with scissors to verify the blood supply. A 2-0 polypropylene purse-string suture is then applied to the open end of the proximal colon (Fig. 21.8). The anvil of a circular stapler is inserted and secured with the purse-string suture (Fig. 21.9). The mesenteric fat is cleared from the end of the bowel close to the anvil and the bowel is returned to the abdomen closing the fascia behind. The pneumoperitoneum is established again to finish the anastomosis.
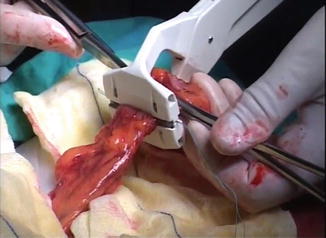




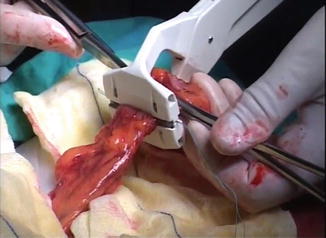
Fig. 21.8
Proximal resection of the rectum with a purse-string device. B Introduction of the circular stapler anvil
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








