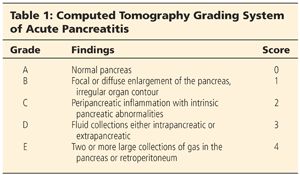
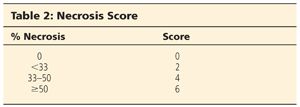
■ The grading of severity of pancreatitis can be classified into five categories (Table 1) and a CT severity index can be calculated based on the grading of unenhanced CT findings and the percentage of necrosis demonstrated on contrast-enhanced CT (Table 2). The CT severity index is the sum of the unenhanced CT score and the necrosis score where the maximum is 10 and greater than or equal to 6 indicates severe disease.4
■ If infected pancreatic necrosis is suspected, the diagnosis is confirmed with culture results from CT-guided fine needle aspiration (FNA) or from specimens collected during necrosectomy.
■ FNA and culture should be obtained in patients who show clinical features of sepsis or those with a deteriorating clinical course 1 to 2 weeks after the onset of disease.
■ Commonly, the Atlanta classification is used to divide acute pancreatitis into mild and severe categories. The criteria for severe acute pancreatitis include the following: a Ranson’s score of 3 or greater, an APACHE II score of 8 or greater within the first 48 hours, organ failure, or local complications (necrosis, abscess, or pseudocyst involving the pancreas). Other predictors of disease severity within the first 24 hours of hospitalization include a C-reactive protein of greater than 120 mg/dL, procalcitonin greater than 1.8 ng/mL, and a hematocrit greater than 44.5
SURGICAL MANAGEMENT
Preoperative Planning
■ Cross-sectional imaging as described earlier is necessary to determine the extent of necrosis, for signs of infection as well as planning of approach.
■ The use of prophylactic antibiotics remains controversial. Antibiotics should be restricted to clear cases of CT-proven pancreatic necrosis and tailored to culture results when available. Current recommendations include imipenem or meropenem for 2 weeks for patients with proven necrosis.6,7 Preoperative antibiotics are recommended prior to incision.
■ Access: large-bore IV or central access for fluid resuscitation, rapid blood transfusion, vasopressor infusion; Foley catheter and nasogastric tube placement. Consider central line and arterial line monitoring in the case of hemodynamic instability.
■ Timing of the procedure: Better outcomes are achieved if necrosectomy is delayed for at least 21 days.8−10 This delay allows for clinical stabilization of the patient, resolution of any signs of organ failure, and decreased inflammatory reaction.
Positioning
■ Positioning for laparoscopic pancreatic necrosectomy should be supine for a transperitoneal approach and lateral for a retroperitoneal approach. If the patient is supine, prep the entire abdomen from nipple to midthigh.
TECHNIQUES
RETROGASTRIC-RETROCOLIC DEBRIDEMENT (TRANSPERITONEAL)
First Step
■ A transperitoneal approach is begun by placing the initial trocar in the periumbilical position (FIG 2).
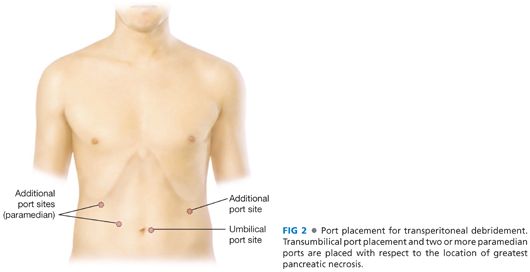
■ A 30-degree angled laparoscope is used to guide the insertion of two right paramedian trocars and an additional assistant’s trocar in the left lateral abdomen. Start with exploratory laparoscopy after establishing pneumoperitoneum.
Second Step
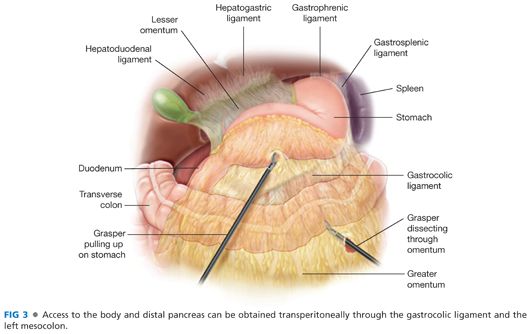
■ The area of necrosis can be approached through the gastrocolic ligament or the transverse mesocolon (FIG 3). If a percutaneous drainage catheter is in place, this can be left in position and used as a guide to identify the necrosis. Dissection is accomplished with a harmonic scalpel or bipolar electrocautery device. The left side of the pancreas may be drained by mobilization of the splenic flexure. In addition, if necrosis extends above the pancreas, the lesser sac may also be entered through the gastrohepatic ligament, taking care to safeguard the right and left gastric arteries.
Third Step
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








