Fig. 15.1
a Operation setup and port placement for laparoscopic distal gastrectomy. b Actual operation setup
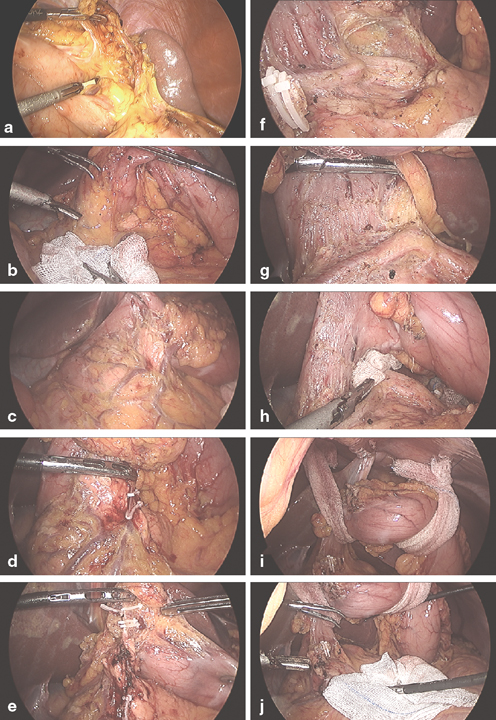
Fig. 15.2
Dissection of greater curvature side of the stomach. Dissection of left gastroepiploic vessels at their origin. Setup for dissection of infrapyloric area; notice the assistant’s right hand a is lifting antrum and the left hand b is push down mesocolon with a gauze, which facilitate separation of omentum from fused mesocolon. c Anterior surface of pancreas head and 2nd portion of duodenum are exposed. d Dissection of right gastroepiploic vein. e Dissection of right gastroepiploic artery. f and g Dissection of duodenum along the gastroduodenal artery. h Put gauze behind right gastric artery pedicle. i and j Hanging stomach using gauze strips around antrum and lower body to facilitate exposure of supra-pancreatic node dissection
Dissection of the Infrapyloric Lymph Nodes (Station 6)
The division of the greater omentum is continued toward the hepatic flexure. The assistant retracts the stomach antrum with right hand instrument and counter traction of mesocolon with left hand instrument (Fig. 15.2b). This maneuver improves the operation field so that the operator can identify the infrapyloric anatomy. The infrapyloric dissection is performed using ultrasonic coagulating shears and should be performed carefully to avoid the tearing of small vessels that leads to troublesome bleeding. The right gastroepiploic vein is identified, ligated, and divided at its origin from the gastrocolic trunk (Fig. 15.2c–e). The right gastroepiploic artery is also divided at its origin from the gastroduodenal artery (GDA) and the infrapyloric branches are then divided to expose the bulb of the duodenum. After then, dissection continues along the GDA until GDA meet common hepatic artery (Fig. 15.2f, g).
After dissection of the posterior side of first portion of duodenum, gauze is inserted in the posterior surface of duodenum (Fig. 15.2h). This maneuver protects underlying vessels during supraduodenal dissection.
Dissection of the Suprapyloric Lymph Nodes and the Hepatoduodenal Ligament Along the Proper Hepatic Artery (Stations 5 and 12a)
For the suprapyloric dissection, the assistant’s right hand is grasping right gastric artery pedicle and left hand presses downward on the pylorus with a grasper over a gauze (Fig. 15.3a, b). The space between right gastric artery and first part of duodenum is divided carefully over the gauze which was put under the duodenum (see Fig. 15.2h). Once this space is opened, the GDA is exposed. Continue dissection along the right side of the hepatic artery and lymph node tissue are pulled off along the vessel to the left side of the patient to enable complete dissection of the station 12a lymph nodes (Fig. 15.3c, d, e, f, g). After ligation and division of the right gastric artery, the duodenal bulb is mobilized and transected distal to the pylorus for Billroth II.
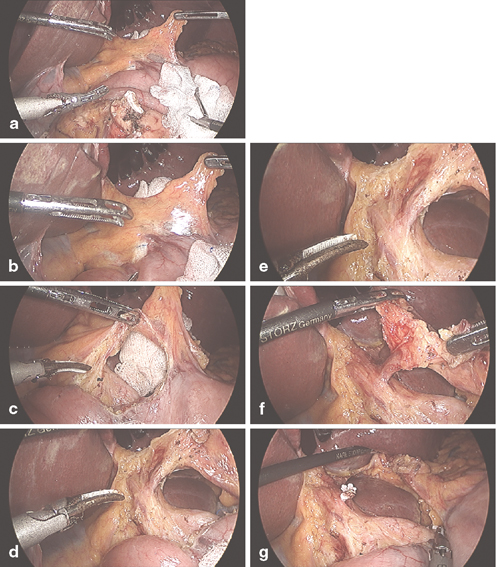
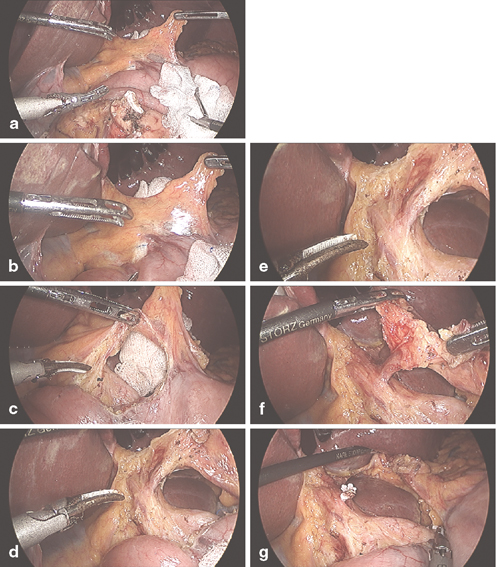
Fig. 15.3
Supra-pyloric dissection a–c the gauze put behind right gastric artery (see Fig. 15.2h) is visible and serves as a safe guard to guide dissection along the 1st portion of duodenum also protect underlying arteries such as gastroduodenal artery. d–f Dissection continues the right side of hepatic artery proper (#12a LN) and along the right gastric artery (#5 LN). g Right gastric artery is ligated and transected
Dissection of the Common Hepatic Artery and Celiac Axis (Stations 7, 8a, and 9)
The pedicle of the left gastric vessels is carefully lifted by the assistant’s right hand and the pancreas is carefully pressed downward by the assistant’s left hand (Fig. 15.4a, b). The dissection of common hepatic artery begins by opening up the peritoneum that overlies the superior border of the pancreas and proceeds from the common hepatic artery to the root of the posterior gastric artery using ultrasonic coagulating shears. After dissection and division of the left gastric artery and vein, all the nodal tissue around the celiac axis should be swept off the retroperitoneum (Figs. 15.4c, d, f).
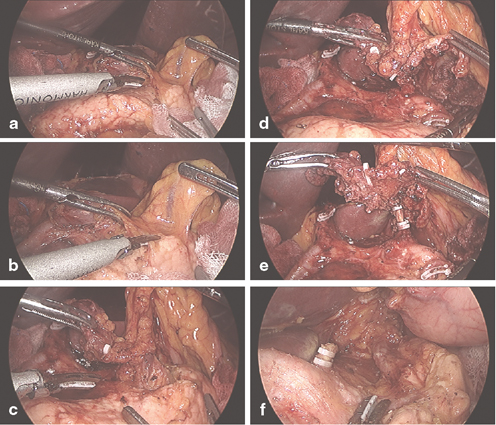
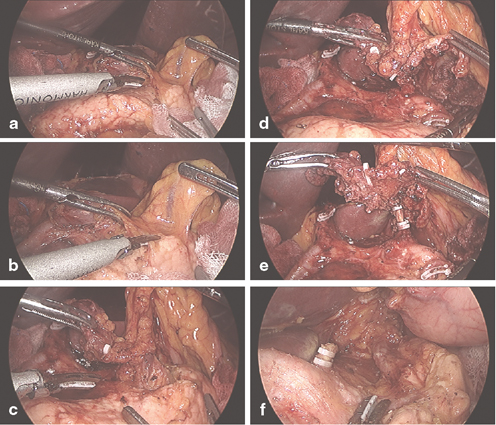
Fig. 15.4
Supra-pancreatic area dissection. a–e Setup for the supra-pancreatic node dissection; (a) the assistant’s right hand ( R) is lifting left gastric vessels pedicle and the left hand ( L) is push down pancreas with a gauze, (f) #11p LN dissected along the splenic artery and vein
Dissection of the Splenic Artery (Station 11p)
After division of the left gastric artery, the soft tissue around the proximal portion of the splenic artery and vein is dissected and removed en bloc until the proximal half of the splenic artery (Fig. 15.4f). During this procedure, the assistant provides downward counter retraction of the pancreas (to evert the upper border of pancreas). Dissection is performed using ultrasonic coagulating shears and should be performed carefully to avoid bleedings from rich small vessels around the splenic vessels that frequently lead to minor bleeding.
Dissection of the Right Paracardial Nodes and Lesser Curvature (Stations 1 and 3)
The upper border of the right paracardia is the junction of the cutting line of the lesser omentum and the right crus of the diaphragm. All the soft tissue around this region should be taken off, and removal of the soft tissue proceeds from the oral side to the anal side along the lesser curvature. It is helpful if the assistant lifts and retracts the soft tissues against the gastric wall during this procedure (Fig. 15.5a, b, c).
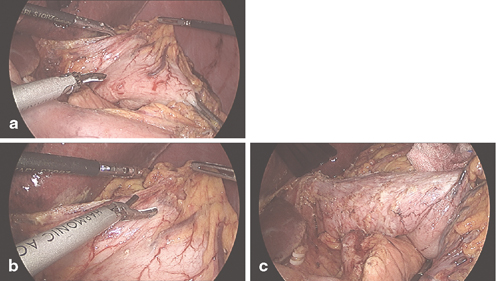
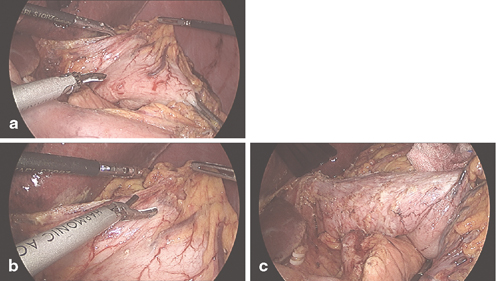
Fig. 15.5
LN dissection along the lesser curvature of cardia and upper stomach. a–c dissection from posterior side of lesser curvature to anterior side
D2 Lymphadenectomy Technique for Laparoscopic Total Gastrectomy
Dissection of the Left Paracardial Area and Short Gastric Artery (Stations 2 and 4sa)
The esophagus is adequately mobilized and transected for laparoscopic total gastrectomy. After transection of the esophagus, the assistant rolls the distal esophageal stump and upper stomach caudally toward the dorsal side of the upper stomach . The esophagocardiac branch of the left inferior phrenic artery is divided at its origin to enable complete dissection of the station 2 lymph nodes. Dissection continues toward the phrenoesophageal membrane and the splenophrenic ligament and finally the posterior surface of the upper stomach is separated from the retroperitoneum.
Dissection of the Splenic Hilum and the Distal Splenic Artery (Stations 10 and 11d)
Dissection of the distal splenic artery continues from the proximal splenic artery to the splenic hilum (Fig. 15.6a). The splenic artery and vein should be exposed and the soft tissue around the vessels and splenic hilum is carefully dissected with ultrasonic coagulating shears to avoid thermal injury that leads to troublesome postoperative pseudoaneurysm (Fig. 15.6b) .
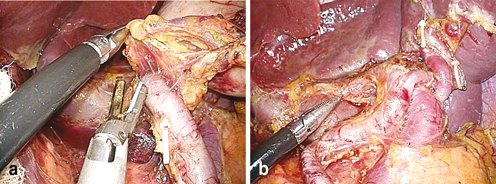
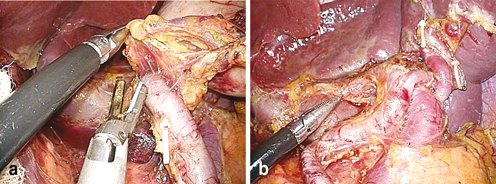
Fig. 15.6
Laparoscopic total gastrectomy with D2 lymphadenectomy. a Dissection around distal splenic artery. b Dissection of splenic hilum
Reconstruction by Billroth I Method after Laparoscopic Distal Gastrectomy
Gastroduodenostomy performed using a Billroth I method is one of the most common types of reconstruction after laparoscopic distal gastrectomy. Billroth I anastomosis preseves the physiologic duodenal passage of food and avoids gastrojejunostomy-related complications such as afferent loop syndrome or Petersen’s hernia. Gastroduodenostomy performed using a Billroth I method is relatively simple and faster than reconstruction performed using Billroth II or Roux-en-Y methods.
Extracorporeal End-to-End Modified Double Stapling Method
For extracorporeal end-to-end modified double stapling, a 4–5 cm length of transverse mini-laparotomy is made on the right upper epigastrium of the abdomen. The duodenum is retrieved and clamped using a purse-string clamp. After completion of a purse-string suture, a Kelly clamp is applied just proximal to the purse-string clamp and the duodenum is transected between the two clamps. An anvil is inserted into the duodenal stump, and a purse-string suture is tied to fix the anvil.
The appropriate proximal resection margin is determined by directly observing the clip through the gastrostomy, and the greater curvature side is partially transected with a linear stapler. The shaft of a circular stapler is introduced into the stomach through the gastrotomy, then the shaft is rotated toward the duodenum and the trocar is advanced to penetrate the corner of the stapling line at the greater curvature.
The trocar is connected to the anvil that has been placed in the duodenum, and the circular stapler is closed and fired, completing the end-to-end gastroduodenostomy by double stapling. After hemostasis of the intraluminal bleeding, the lesser curvature side of the proximal stomach is transected completely using another linear stapler.
This method has several advantages over other methods of Billroth I anastomosis: ((1) it permits the proximal resection margin to be longer than with other methods; ((2) it results in the equal tension on the anterior and posterior walls of the remnant stomach; and ((3) it does not need an additional gastrotomy on the remnant stomach [21].
Extracorporeal End-to-Side Posterior Wall Method
The distal resection and anvil insertion performed in the extracorporeal end-to-side posterior wall method are the same as in the extracorporeal end-to-end modified double stapling method. For proximal resection, the stomach is transected from the greater curvature to the lesser curvature in two steps: (1) The greater curvature side of the planned proximal margin is grasped with two clamps and transected between the two clamps, and (2) the remaining lesser curvature side is transected using a linear stapler. After the specimen is removed, the shaft of a circular stapler is introduced into the stomach through the gastrostomy, which was previously clamped. The trocar is advanced to penetrate the posterior wall of the remnant stomach. The circular stapler is closed and fired, completing the end-to-side gastroduodenostomy. Finally, the gastrotomy is closed using another linear stapler [22].
Intracorporeal Delta-Shaped Method
The intracorporeal Billroth I method has gained popularity since Kanaya et al. reported the first delta-shaped anastomosis [23]. Delta-shaped anastomosis is a functional end-to-end gastroduodenostomy technique performed using linear staplers, and it offers technical simplicity, wider lumen anastomosis, and a better cosmesis in comparison to the extracorporeal Billroth I methods, and a good surgical field even in obese patients. However, it requires sufficient length of duodenal stump and remnant stomach, so is not recommended when the tumor is located above the angle of the stomach or very close to the pylorus.
After mobilization of the gastroduodenum, a 60-mm linear stapler is introduced through the left lower 12-mm trocar and the duodenal bulb is transected just below the pylorus. The direction of the stapling is more vertical (posteroanterior direction) than the conventional mesentero-antimesenteric direction, resulting in a favorable blood supply and the appropriate angle for the anastomosis (Fig. 15.7a).
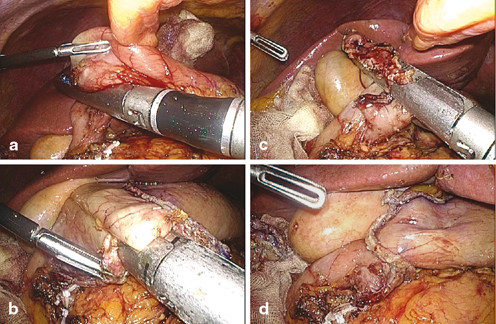
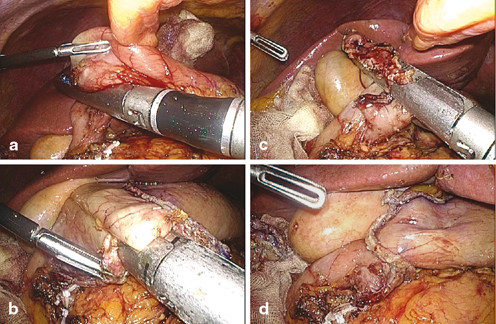
Fig. 15.7
Intracorporeal delta-shaped Billroth I anastomosis. a Posteroanterior transection of the duodenum just below the pylorus. b Side-to-side gastroduodenostomy. c Closure of the entry hole using a 60-mm linear stapler. d View after the anastomosis
After proximal transection of the stomach with several linear staplers, the specimen is removed from the abdominal cavity through the extended umbilical wound. Entry holes are made on the tip of the greater curvature side of the remnant stomach and on the posterior tip of the duodenal stump using laparoscopic electrocautery or a harmonic scalpel. The cartilage jaw of a 45-mm linear stapler is inserted into the stomach and the remnant stomach is rotated to the posterior wall side. The jaw of the stapler is inserted into the duodenal stump and the duodenum is also rotated toward the posterosuperior wall to form a side-to-side (posteroposterior) gastroduodenostomy (Fig. 15.7b). After firing the stapler and hemostasis, the common entry hole is closed by one or two 60-mm linear staplers (Fig. 15.7c, d). Transient approximation of the entry hole using stay sutures can be helpful for making an aligned closure of the common entry hole.
Other Intracorporeal Billroth I Methods
Several intracorporeal Billroth I methods have been introduced that use circular staplers [24–26]. However, these techniques are not preferred over delta-shaped anastomosis because of the technical difficulty in the intracorporeal purse-string suture and long-operation time caused by the extracorporeal processes.
Reconstruction by Gastrojejunostomy After Laparoscopic Distal Gastrectomy
Intracorporeal Billroth II/Uncut Roux-en-Y Method
After radical lymphadenectomy and confirmation of a negative resection margin on the frozen section biopsy, a 15–20 cm jejunal loop from the ligamentum of Treitz is brought up to the remnant stomach with atraumatic forceps and the jejunal loop is laid besides the remnant stomach in the antiperistaltic direction to examine any tension in the mesentery.
Entry holes are made on the tip of the greater curvature side of the remnant stomach and on the antimesenteric surface of the jejunum using laparoscopic electrocautery or a harmonic scalpel. A 60-mm linear stapler is introduced through the right lower port. The cartilage jaw of the staplers is inserted into the jejunum and the anvil jaw is then inserted into the stomach. The stapler is fired to complete the gastrojejunostomy (Fig. 15.8a). After hemostasis, the common entry hole is closed with another linear stapler or a running suture with an absorbable thread.
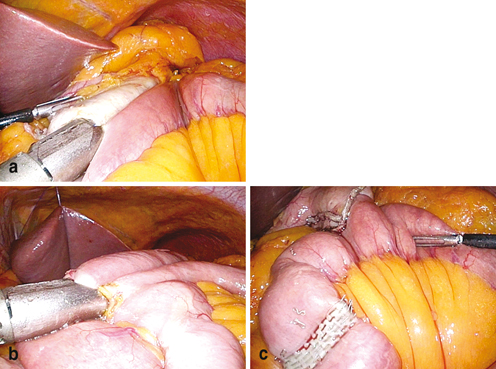




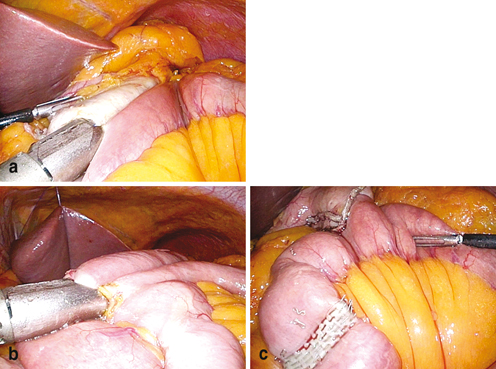
Fig. 15.8
Intracorporeal uncut Roux-en-Y gastrojejunostomy. a antiperistaltic side-to-side gastrojejunostomy using a 60-mm linear stapler. b Side-to-side jejunojejunostomy using a 60-mm linear stapler. c View after uncut procedure on the afferent loop using a 45-mm knifeless linear stapler
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







