Fig. 11.1
OR setup with the teaching surgeon using his hand and trainee operating. With permission from Carter J, Whelan RL. Hand assisted laparoscopic anterior resection. In: Milsom JW, Bohm B, Nakajima K, eds. Laparoscopic colorectal surgery. Springer, New York 2006;pp:255–273. © Springer 2006
Procedure
Port Placement and Hand Device
The ideal features of a hand-assisted device have previously been defined [2]. The device needs to be flexible to allow for a wide range of motion of the surgeon’s hand without permitting gas leakage. The device should also function as a wound protector and retractor for portions of the operation that will be performed through the hand-access device. The ergonomics of the device are also essential to ensure surgeon comfort and appropriate circulation to the surgeon’s hand during long operations.
For a low anterior resection, a Pfannenstiel incision, opening the anterior fascia transversely and dividing the posterior fascia longitudinally without dividing the rectus, is well suited (Fig. 11.2). It is important to dissect the anterior fascia off the rectus superiorly almost to the umbilicus and inferiorly as far as possible. This maneuver is the key in achieving adequate retraction and exposure. This incision has a low incidence of hernia formation [3]. Perforating vessels should be carefully controlled to prevent a rectus sheath hematoma. One disadvantage of this incision is that conversion to an open may require a midline incision that will eventually lead to an inverted “T”-shaped incision. The actual length of the incision is usually dependent on the glove size of the surgeon. A general rule of thumb is to create an incision the same length as the surgeon’s glove size in centimeters.
Fig. 11.2
Pfannenstiel incision showing muscle separation along the midline. With permission from Yuko Tonohira
For cases where the likelihood of conversion to open surgery is high, a lower midline incision for the hand-access device is better suited. This incision allows for easy conversion to a midline laparotomy, should it be necessary.
After induction of anesthesia, the abdomen is draped in the usual fashion, and a Pfannenstiel incision is made 1–2 fingerbreadths above the top of pubis. After raising flaps as described earlier, the peritoneal cavity is entered with careful attention to protecting the bowel and the urinary bladder. Placing the patient in Trendelenburg position helps move the small bowel away from the pelvis. The flexible ring of the wound protector is inserted and flattened against the parietal peritoneum.
A 10 mm port is placed at the umbilicus under manual guidance through hand port. The lid of the hand-assisted device is placed and pneumoperitoneum is established. Exploratory laparoscopy is performed to rule out metastatic disease. The feasibility of a laparoscopic approach can also be established at this time.
Under direct visualization, two 5 mm ports are placed on the right side—lateral to the rectus muscle to avoid the inferior epigastric artery. The trocars should be one palm breath from each other and away from the anterior superior iliac spine. If a stoma is planned on the right side, our preference is to place trocars lateral and well away from stoma to avoid pouching difficulties with trocar sites. One or two 5 mm trocars are also placed on the left side (Fig. 11.3).
Fig. 11.3
Suggested port placement. With permission from Yuko Tonohira
The monitors are positioned on both sides of the patient, with two monitors positioned on the left. The operating surgeon can stand on the right of the patient—using his/her right hand through the hand-assisted device and the left hand with a dissecting tool. A teaching surgeon may choose to stand between the legs and use either hand to expose for a trainee or operating surgeon.
The use of a moist laparotomy pad or a tagged towel placed intracorporeally through the hand-access device can facilitate retraction of the small intestines and cleaning of the laparoscope [4].
Positioning and Alterations During Case
The patient is placed in the steep Trendelenburg position and left side up. The omentum is positioned superior to the transverse colon. The small bowel is moved to the right of the abdomen. At this point, there should be clear visualization of the mesentery of the left colon, the ligament of Treitz and the inferior mesenteric artery and vein. Placing the patient in reverse Trendelenburg may facilitate takedown of the splenic flexure.
Technical Aspects
Mobilization
Place the greater omentum in the upper abdomen over the liver and the small bowel to the upper right quadrant of the abdomen (Fig. 11.4).
Fig. 11.4
Exposure is achieved by placing the omentum in the upper abdomen and the small bowel in the right upper quadrant. With permission from Leroy J, Henri M, Rubino F, Marescaux J. Sigmoidectomy. In: Milsom JW, Bohm B, Nakajima K, eds. Laparoscopic colorectal surgery. Springer, New York 2006;pp:145–169. © Springer 2006
Expose the left colon mesentery and inferior mesenteric artery and vein. The hand is used to identify and follow the sacral promontory and put traction on the inferior mesenteric artery (Fig. 11.5) by retracting the pedicle superiorly and anteriorly.
Fig. 11.5
Lateral traction on the sigmoid colon exposes the inferior mesenteric artery. With permission from Carter J, Whelan RL. Hand assisted laparoscopic anterior resection. In: Milsom JW, Bohm B, Nakajima K, eds. Laparoscopic colorectal surgery. Springer, New York 2006;pp:255–273. © Springer 2006
The peritoneum along the inferior aspect of the pedicle is incised sharply, starting at the sacral promontory and working toward the origin of the inferior mesenteric vessels (Fig. 11.6).
Fig. 11.6
A peritoneal window is created to start the retromesenteric dissection. With permission from Yuko Tonohira
The inferior mesenteric artery is isolated at its origin. Care is taken to protect the main trunks of the hypogastric nerves that run posterior along the aortic plexus and must be swept dorsally.
Blunt retromesenteric dissection is started carefully ensuring that the retroperitoneal fascia (purple) is not lifted with the mesentery (Fig. 11.7).
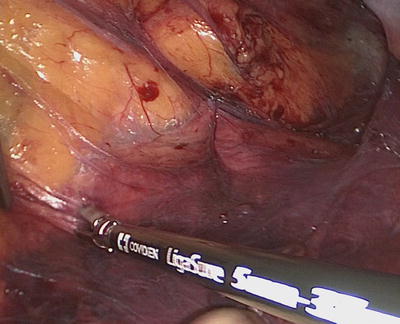
Fig. 11.7
“Purple down” The retroperitoneal fascia (purple) is dissected off the mesentery (yellow)
Using traction and countertraction, the retro-mesenteric plain is developed laterally and superiorly.
It is critical to identify the left ureter prior to dividing any mesenteric vessels in order to avoid injury (Fig. 11.8). The left ureter is located medial to the gonadal vessels at this level and more distally at the level of the common iliac bifurcation. If the left ureter cannot be identified, a different surgical exposure method such as lateral-to-medial mobilization can be utilized. Alternatively, the ureter can be identified more proximally near the origin of the IMA. If all of the laparoscopic maneuvers fail to identify the ureter, open dissection through the Pfannenstiel incision can be attempted.
Fig. 11.8
Identification of the ureter prior to dividing the vascular pedicle With permission from Yuko Tonohira
The inferior mesenteric artery (IMA) is isolated, and a window is created around the vessel ensuring the ureter is not lifted up with the mesentery. All vessels are divided with a bipolar energy device with overlapping burns. Leaving a stump helps control unexpected bleeding (Fig. 11.9). In patients with calcified mesenteric vessels, either vessel loop ligator, clips, or laparoscopic stapler should be used for vessel ligation.
Fig. 11.9
Division of the pedicle with an energy device preserving the left colic With permission from Yuko Tonohira
Depending on the location of the tumor, the IMA can be divided high on the aorta (Fig. 11.10) or can be ligated distal to the take off of the left colic. Division distal to the left colic theoretically provides an extra source of arterial blood flow to the conduit without sacrificing oncological principles.
Fig. 11.10
High ligation of the IMA (proximal to the left colic) With permission from Yuko Tonohira
Division of the IMA facilitates completion of the retromesenteric dissection (Figs. 11.11 and 11.12).
Fig. 11.11
Retromesenteric dissection using traction and counter-traction With permission from Carter J, Whelan RL. Hand assisted laparoscopic anterior resection. In: Milsom JW, Bohm B, Nakajima K, eds. Laparoscopic colorectal surgery. Springer, New York 2006;pp:255-273 . © Springer 2006
Fig. 11.12
Retromesenteric dissection ensuring that the purple retroperitoneal fascia is kept down and the ureter is protected. With permission from Carter J, Whelan RL. Hand assisted laparoscopic anterior resection. In: Milsom JW, Bohm B, Nakajima K, eds. Laparoscopic colorectal surgery. Springer, New York 2006;pp:255–273. © Springer 2006
Medially to the root of the mesentery.
Laterally to the white line.
Superiorly to the inferior border of the pancreas.
The inferior mesenteric vein (IMV) is divided. Of note, the ligament of Treitz may need to be partially released to obtain adequate exposure of the IMV, and there is an avascular plane just lateral (i.e., to the right) to its origin. The duodenum needs to be protected from inadvertent thermal injury. High division of the IMV at this location is critical to achieve good mobilization and a tension-free anastomosis in the low-lying pelvis.
An alternative approach is to perform the IMV dissection first followed by the IMA dissection. The lesser sac can be entered anterior to the pancreas with this approach. Care should be taken to ensure that the mesentery to the transverse colon is protected.
The lesser sac can also be entered by releasing the omentum from the transverse colon (Fig. 11.13). The gastrocolic attachments need to be divided to achieve adequate mobilization.
Fig. 11.13
The omentum is released from the transverse colon. With permission from Carter J, Whelan RL. Hand assisted laparoscopic anterior resection. In: Milsom JW, Bohm B, Nakajima K, eds. Laparoscopic colorectal surgery. Springer, New York 2006;pp:255–273. © Springer 2006
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








