Hysteroscopy and Hysterosalpingography
Jacques Barbot
Hubert Guedj
Has hysterography become an obsolete method of diagnosis, and will hysteroscopy replace it? Since the renewal of interest in hysteroscopy, this question has been commonly asked. For a long time, hysterography was the only feasible method to visualize the uterine cavity, and a high degree of refinement was attained in the interpretation of the hysterogram. On the other hand, hysteroscopy was considered a curiosity without practical value. As the efficiency of hysteroscopy was increasing, its confrontation with hysterography gradually showed the weak points of the radiologic method. Today the current has reversed in the same excessive way, and the tendency is to consider hysterography as an outmoded technique that has lost its utility.
Long experience with the two techniques and a constant comparison of the results provided by each of them have shown that each technique has inherent defects and strengths; often the two are complementary. Certainly hysteroscopy is the most direct method of investigation that integrates all the richness and nuances of the visual sense in enabling one to reach the right diagnosis. Shape, contours, relief, colors, vasculature, consistency, and mobility are sight-oriented parameters. Hysterography is an indirect method, using a contrast medium in an attempt to disclose the contour of the uterine cavity and providing only black-and-white shadows. Nevertheless, this technique of investigation is very delicate, and the contrast medium is often able to find its way into structures that remain out of reach of visual examination.
Technique of Hysterosalpingography
The technique of hysteroscopy is fully described in this book and will not be described again here. The methodology of hysterosalpingography (HSG) is simple, but it is worthwhile to specify certain points of importance. HSG provides valuable information only when the procedure is performed with technical perfection. We will not describe the technique in detail, but will emphasize the main points that are essential for a correct interpretation of the x-ray images.
A water-soluble contrast medium should be used to obtain the most discriminating images of the uterine cavity and the fallopian tubes. The spreading of the medium must be observed under fluoroscopic control to time the x-ray images at definite stages of the filling, with each stage providing specific information. With this technique, five judiciously taken films are amply sufficient for a complete investigation. The first image is taken during initial filling; very little dye is instilled to obtain a halftone image that reveals the details of the mucosa and small filling defects. The second is taken after complete filling of the uterine cavity. This image is used to determine uterine contour, size, and general configuration. It may demonstrate an abnormality of the uterus such as congenital malformation, endometrial polyp, myoma, or endometrial carcinoma. It also reveals the anatomy and patency of the tubes. Normally the dye should reach the distal end of the tubes and spill freely into the pelvis. The third is an anteroposterior image. It provides information about the position of the uterus and can enable detection of displacements such as retroversion. It is also needed to determine the exact location of a filling defect with respect to the anterior or posterior wall of the uterus. The course of the tubes is also visualized. The fourth image is taken after removal of the cannula during evacuation of the dye. It gives an overall view of the genital tract and allows optimal study of the internal os and endocervix. The fifth image is very important for infertility evaluation. It is taken 15 to 20 minutes after removal of the cannula. It will enable one to confirm whether the tubes are normally patent, with dye dispersing freely into the abdominal cavity, or whether the dye is trapped within diseased tubes (e.g., in the case of hydrosalpinx) or has become loculated in the peritoneal cavity (e.g., in the case of adhesions).
Some technical mistakes are not uncommon when performing HSG and may be responsible for erroneous interpretation. The investigation should be performed during the proliferative phase of the menstrual cycle. The atony of the uterus resulting from the action of progesterone may be misleading. Uterine bleeding is a contraindication, since blood clots cause artificial filling defects on the imaging study. The introduction of air bubbles during filling by way of the cannula may cause artifacts suggestive of intrauterine disease. In the same way, a cannula that is not tightly sealed at the cervix may cause leakage of the contrast medium and artifacts. Failure to
apply enough traction on the cervix to correct for anteversion or retroversion will not allow adequate exposure of the uterus perpendicularly to the x-rays and results in distortion and foreshortening of the image. Nonremoval of a radiopaque speculum after fixing the cannula to the cervix will obtund meaningful evaluation of the endocervical canal. All of these mistakes can be easily avoided. In brief, the technical quality of the hysterogram required for proper reading of the film can be easily obtained by respecting the following points:
apply enough traction on the cervix to correct for anteversion or retroversion will not allow adequate exposure of the uterus perpendicularly to the x-rays and results in distortion and foreshortening of the image. Nonremoval of a radiopaque speculum after fixing the cannula to the cervix will obtund meaningful evaluation of the endocervical canal. All of these mistakes can be easily avoided. In brief, the technical quality of the hysterogram required for proper reading of the film can be easily obtained by respecting the following points:
In women of reproductive age, performance of procedure during the proliferative phase
In all cases, performance of procedure not too close to a period of bleeding
Use of a water-soluble contrast medium
Removal of all air bubbles from the cannula
Tight seal of the speculum before taking the films
Proper traction on the cervix
Use of fluoroscopic control to select the proper images
Appearance of the Normal Uterine Cavity as Visualized by Hysterography and by Hysteroscopy
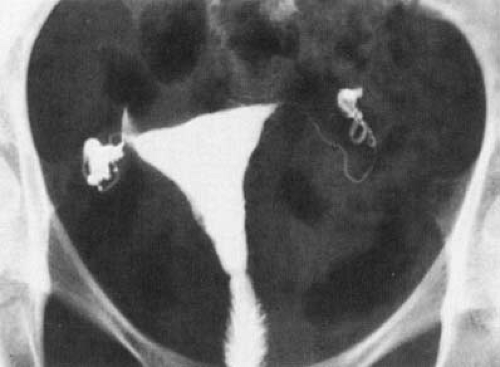
What is seen of the uterine cavity on the radiograph is in fact the geometric projection of the cavity on a flat surface (the radiographic plate). The uterus should be parallel to the plate to achieve an orthographic projection that preserves true angles and proportions of the image. This geometric approach has the great advantage of enabling one to perceive the general configuration of the uterine cavity and the relations between its different parts. An accurate mapping of the cavity is thus obtained with a small enlargement that depends on the thickness of the tissues that keep the uterus away from the radiographic plate (Fig. 18.1). Exact measurement can be obtained by taking into account the coefficient of enlargement (10% to 20%).
On the normal hysterogram, the endocervical canal appears as a fusiform cavity tapering toward the internal os. The pattern of the arbor vitae stands out as a network of denser lines. The contours are made irregular by the injection of crypts and mucous glands forming oblique diverticula. These irregularities are variable and inconstant, and often make the evaluation of the endocervix difficult. The isthmus is a narrow channel with a stricture at each end. The endometrial cavity appears as a triangle, roughly isosceles, with the short base up. In fact, the lateral sides of the hysterogram are not straight lines but are made up of two segments forming an angle about halfway between the internal os and the tubal ostium, with the upper segment diverging out. Thus the endometrial cavity is divided into two parts. The lower part above the internal os is rather narrow and funnel shaped. The upper part widens out and includes the fundus in the middle and the two cornua laterally. The tubal ostia are often marked by a stricture followed by a dilated triangle corresponding to the initial portion of the tube. We will not describe the tube further because it cannot be investigated hysteroscopically and no comparison is possible.
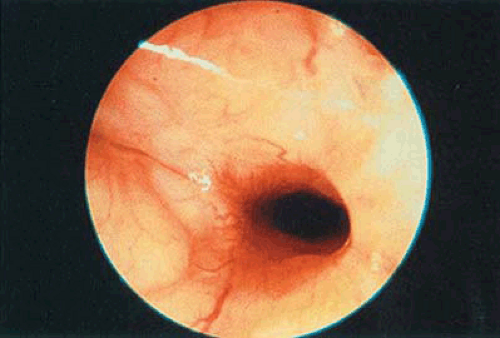 FIGURE 18.2 Normal hysteroscopic appearance of the endocervical canal. The internal os is opened by the pressure of the gas. |
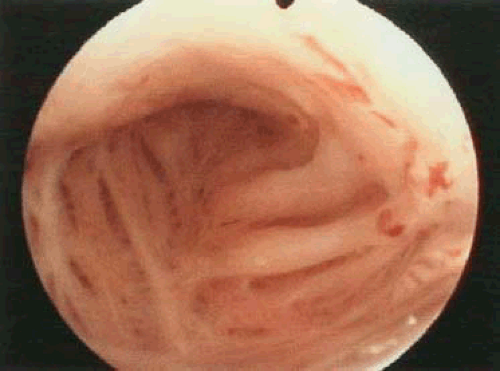
The hysteroscopic panoramic view of the uterine cavity is radically different. The cavity is seen in perspective in a lengthwise direction and the proportions are no longer maintained, the foreground being enlarged compared with the background. The distortion is dramatically increased by the optical instrument through which the inside of the uterus is scrutinized. If this situation is advantageous for the study of small details, a mental correction is always necessary to restore the true size and extent of each structure relative to the others. With panoramic hysteroscopy, the endocervical canal appears as a barrel-shaped cavity. Its cross section is circular (Fig. 18.2). It is best examined during the removal of the endoscope, after
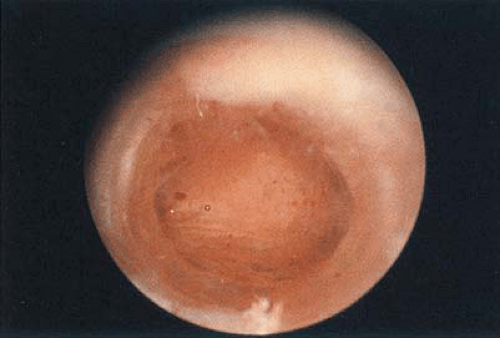
the endometrial cavity has been evaluated. The leakage of the distending medium is less important than passage through the isthmus where distention must be optimal. The relief of the arbor vitae, made up of longitudinal and oblique folds separated by furrows, is nicely displayed. The internal os appears as a dark, round hole; its size depends on the pressure of the distending medium (Fig. 18.3). After the isthmus is passed, the endometrial cavity is viewed as a suite of two chambers connected by a large opening (Fig. 18.4). The lower chamber, which is cone shaped with the vertex down, often appears cylindrical because of the distortion of the optical system. The upper chamber is composed of a central portion, the fundus, and two lateral conical alcoves, which are the cornua joined by the tube at the vertex (Fig. 18.5). The communication of the two main chambers corresponds to the angulation we described on the hysterogram lateral outlines. Hysteroscopically it is an oval or circular opening with blunt or sharp edges, depending on the degree of divergence of the two horns. The thickness, color, vasculature, and consistency of the mucous membrane covering the uterine cavity vary with the time of the menstrual cycle. Hysteroscopy has demonstrated that the stricture followed by a dilated triangle— often visible at the origin of the tube on the hysterogram and considered at one time as a sphincter—was in fact a mucosal fold (Fig. 18.6). Hysteroscopically the tubal ostium may show various appearances. It may be circumscribed by a circular mucosal fold followed by a dilated portion. In that case, the first millimeters of the intramural portion of the tube can be evaluated and small tubal polyps may be disclosed. The mucosal fold can be incomplete (i.e., semicircular). Sometimes the ostium is reduced to a plain, narrow hole
without any fold or dilatation (Fig. 18.7). In reality the tubal ostium is often punctiform, as can be established by contact hysteroscopy. Only the pressure of the distending medium makes it appear wide open.
the endometrial cavity has been evaluated. The leakage of the distending medium is less important than passage through the isthmus where distention must be optimal. The relief of the arbor vitae, made up of longitudinal and oblique folds separated by furrows, is nicely displayed. The internal os appears as a dark, round hole; its size depends on the pressure of the distending medium (Fig. 18.3). After the isthmus is passed, the endometrial cavity is viewed as a suite of two chambers connected by a large opening (Fig. 18.4). The lower chamber, which is cone shaped with the vertex down, often appears cylindrical because of the distortion of the optical system. The upper chamber is composed of a central portion, the fundus, and two lateral conical alcoves, which are the cornua joined by the tube at the vertex (Fig. 18.5). The communication of the two main chambers corresponds to the angulation we described on the hysterogram lateral outlines. Hysteroscopically it is an oval or circular opening with blunt or sharp edges, depending on the degree of divergence of the two horns. The thickness, color, vasculature, and consistency of the mucous membrane covering the uterine cavity vary with the time of the menstrual cycle. Hysteroscopy has demonstrated that the stricture followed by a dilated triangle— often visible at the origin of the tube on the hysterogram and considered at one time as a sphincter—was in fact a mucosal fold (Fig. 18.6). Hysteroscopically the tubal ostium may show various appearances. It may be circumscribed by a circular mucosal fold followed by a dilated portion. In that case, the first millimeters of the intramural portion of the tube can be evaluated and small tubal polyps may be disclosed. The mucosal fold can be incomplete (i.e., semicircular). Sometimes the ostium is reduced to a plain, narrow hole
without any fold or dilatation (Fig. 18.7). In reality the tubal ostium is often punctiform, as can be established by contact hysteroscopy. Only the pressure of the distending medium makes it appear wide open.
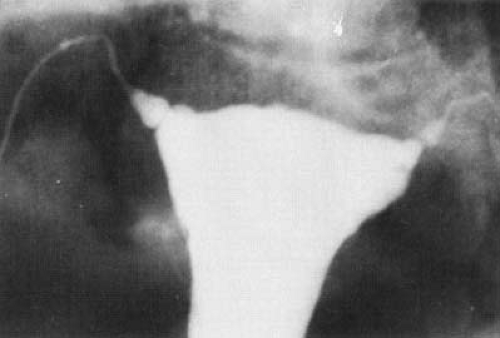 FIGURE 18.6 Hysterogram demonstrates the initial portion of the tubes marked by a stricture followed by a dilated triangle. This aspect was thought at one time to be due to a sphincter. |
We have now described two different representations of the same uterine cavity. The hysterographic perspective has cartographic qualities and we can refer to it each time we want to know the exact configuration of the premises. The hysteroscopic perspective is the eye within the cavity, which provides the details accurately.
Typical Appearance of the Most Common Abnormalities as Visualized by Hysterography and by Hysteroscopy
The correct diagnosis using the hysterographic approach is based on the analysis of the alterations of the normal radiographic shadows caused by the presence of intrauterine disorders. Two types of alterations are analyzed. First, there are the direct signs, which represent the shadow of the lesion itself. When the lesion lies or protrudes into the uterine cavity, its presence causes a filling defect, which provides a lacunar image on the normal triangular uterus shadow. Polyps, myomas, synechiae, and carcinoma are responsible for this type of alteration. When the lesion extends outward from the uterine cavity through the myometrium, it adds its own shadow to the outline of the normal uterus, which becomes modified by diverticula or pouches. Adenomyosis, cesarean scars, myomectomy, or uterus perforation can produce this type of alteration. Second, there are the indirect signs, which represent the repercussion of the lesion and the general shape of the uterine cavity. They appear as distortion, enlargement or shrinkage, rigidity, or swelling and contribute to the final appearance of the uterine shadow from which one should be able to infer the correct diagnosis. All the art of hysterography lies in the ability to match a given uterine shadow with a specific uterine disease.
The hysteroscopic approach is different since the lesion is seen directly, and the collection of information is much
greater and varied. Emphasis will be placed on the hysterographic signs, since the hysteroscopic appearance of most lesions is thoroughly described in Chapter 19.
greater and varied. Emphasis will be placed on the hysterographic signs, since the hysteroscopic appearance of most lesions is thoroughly described in Chapter 19.
Endometrial Polyps
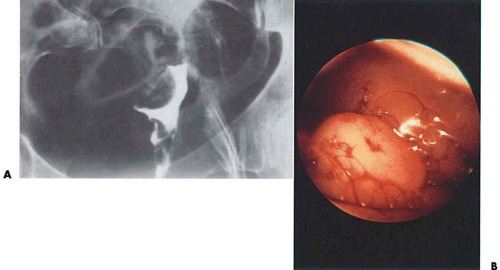
On the hysterogram, the direct sign of endometrial polyps is a filling defect having a contour that is regular but not too sharp and that tends to fade as the instillation of the contrast medium increases (Fig. 18.8). This defect is also mobile during the filling of the uterine cavity (Fig. 18.9). The pedicle is sometimes visible, and its implantation is determined on the anteroposterior film. The outline of the uterine cavity is not distorted but quite normal, this being in favor of a soft formation. However, in the case of a very large polyp, a distorted hysterogram may be suggestive of a myoma (Fig. 18.10).
 FIGURE 18.11 CO2 panoramic hysteroscopy showing the polyp seen in Figure 18.9. |
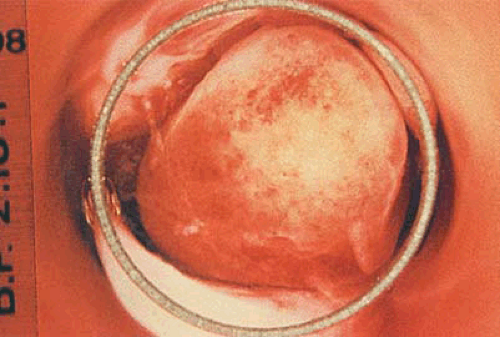 FIGURE 18.12 Contact hysteroscopy of the polyp seen in Figure 18.11. |
The diagnosis of a polyp is practically never missed by the hysteroscopic examination (Fig. 18.11). The appearance of the overlying mucosa allows one to determine whether it is functional or nonfunctional (Figs. 18.12 and 18.13).
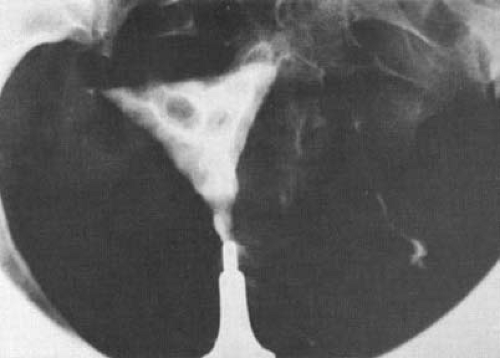
Submucous Myomas
In the case of submucous myomas, the typical hysterogram demonstrates a round, regular filling defect (Fig. 18.14). The base of implantation, which appears on the anteroposterior film, is broad. The location of the defect does not change during the filling of the cavity. The main feature is the distortion of the hysterogram, which results from the firmness of the lesion, the contours becoming convex. Sometimes the whole cavity seems blown up. In the case of a purely intramural myoma, no filling defect is visible and only the distortion of the hysterogram is suggestive of the lesion.
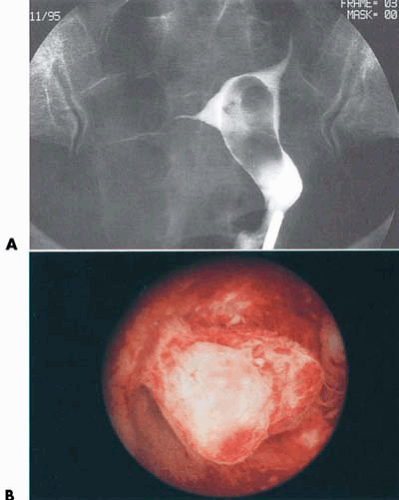 FIGURE 18.13 A: The hysterogram shows a large filling defect. B: Twin polyps are seen floating in glycine. They were detected following an episode of uterine bleeding. |
 FIGURE 18.14 Circular filling defect suggestive of a submucous myoma as the endometrial cavity is distorted. |
The hysteroscopic diagnosis of a myoma is easy (Fig. 18.15). The hemispheric protrusion bulging into the uterine cavity is regular, smooth, firm, and covered with atrophic endometrium and dilated vessels. The pedunculated fibroid is less typical and may resemble an endometrial polyp. The purely intramural myoma is difficult to detect, since the distortion of the endometrial cavity is its only sign and is not hysteroscopically obvious.
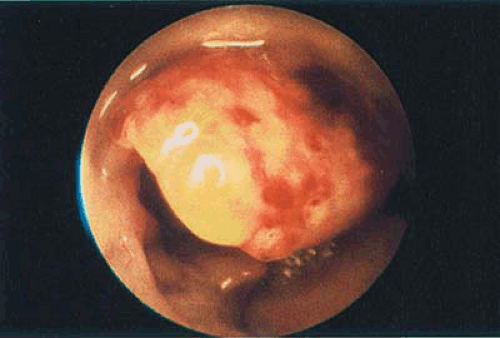 FIGURE 18.15 The corresponding (see Fig. 18.14) hysteroscopic study confirms the presence of a submucous myoma. |
Endometrial Hyperplasia
Diffuse endometrial hyperplasia is typically characterized by numerous regular filling defects of different sizes and separated by denser outlines (Figs. 18.16 and 18.17). The whole
hysterogram looks dappled, and the contours are often hazy or indented but the cavity is not distorted. The diagnosis of focal hyperplasia is much more difficult and is often missed. The only sign may be an inconstant defect appearing on the initial filling and then disappearing.
hysterogram looks dappled, and the contours are often hazy or indented but the cavity is not distorted. The diagnosis of focal hyperplasia is much more difficult and is often missed. The only sign may be an inconstant defect appearing on the initial filling and then disappearing.
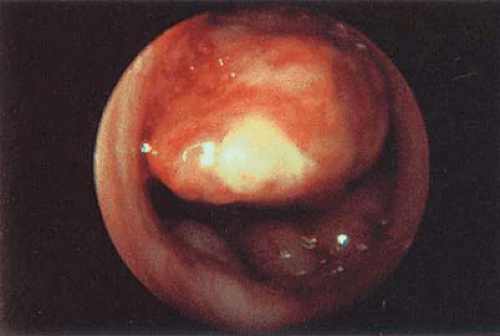 FIGURE 18.17 This polyp is in fact a polypoid form of carcinoma. The surface is irregular and displays atypical vessels. |
Although the diagnosis of hyperplasia may be difficult hysteroscopically, the visual examination usually provides extra information concerning the type of hyperplasia—which can be plain, polypoid, or cystic (Fig. 18.18). It is most important to find any areas of atypical hyperplasia that might be undetectable on the hysterogram (Fig. 18.19).
 FIGURE 18.18 Hysteroscopy finding (see Fig. 18.16) is suggestive of hyperplasia mucosa. The protrusions are responsible for the filling defects on the hysterogram. |
Endometrial Carcinoma
The extended carcinoma usually exhibits characteristic features on the hysterogram (Fig. 18.20). The filling defect is not uniform and has a jagged contour. Many terms have been commonly used in Europe to depict it, such as “boggy” or “moth-eaten.” A portion of the hysterogram may appear to be “amputated.” The intravasation of the contrast medium is not uncommon, and its consequences concerning dissemination of cancer cells may alarm some physicians. Additionally, the early carcinoma does not always present a typical appearance, and the diagnosis may be missed. Staging of the tumor can also be established on the hysterogram, but it has already been demonstrated that hysteroscopy yields more accurate results.
 FIGURE 18.19 Diffuse hyperplasia as seen by hysteroscopy. The thickened walls of the uterus are closely opposed. |
 FIGURE 18.20 Hysterogram is suggestive of an endometrial carcinoma displaying a very irregular ragged filling defect, especially along the right lateral outline. |
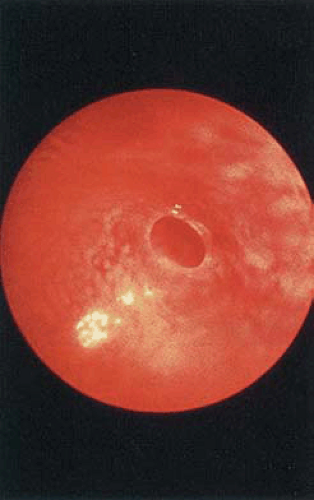
Several hysteroscopic patterns of invasive endometrial carcinoma have been described, among which the vegetating type is the most common (Fig. 18.21). The main advantage of visual control is to provide directed sampling
of small, uncertain lesions and thus allow earlier diagnosis (Fig. 18.22).
of small, uncertain lesions and thus allow earlier diagnosis (Fig. 18.22).
 FIGURE 18.21 Hysteroscopy confirmed the invasive carcinoma having the gross appearance of the vegetating type.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|