Fig. 23.1
(a) Operative positioning of the patient, the surgical team, and the robot. (b) Trocar positioning of the robotic and assistant ports. A 12-mm camera port (c) is placed at the halfway point between the xiphoid process and the pubis symphysis. A line is drawn connecting the C port to the right and left anterior superior iliac spines. Three robotic ports (R) are then placed, four-finger breadths apart from each other. Two additional 5-mm laparoscopic ports (L) are also inserted. L1 is located along the right mid-clavicular line, four-finger breadths lateral to C and about four-finger breadths superior to R1. L2 is just lateral to the midline, four-finger breadths from L1
Patient positioning should be completed in such a way that the operating room table can be placed in steep Trendelenburg or in extreme lateral positions without the patient sliding. Despite the numerous techniques described to prevent patient sliding, such as beanbags and different types of straps, patient injuries have been described and can be as devastating as brachial plexus injuries and lower extremity nerve injuries with and without associated compartment syndrome. Ensuring adequate positioning is key prior to starting the operation, since unintended changes in patient position may be difficult to assess once sterile drapes are in place.
Our preference is to position the patient directly on a large high-viscosity foam mat with Velcro straps that are then secured to the table. In theory, this mat provides a friction hold, decreasing in-line sliding that may occur either during Trendelenburg or reverse Trendelenburg position. A second Velcro strap is required to prevent lateral sliding. It is placed across the chest and secured as well to the operating table at this level. It prevents sliding when the bed is tilted towards the right. It is our preference to tuck both arms, parallel to the patient on the operating table. However, it is not always necessary to tuck the left arm.
When treating rectal cancer or when transanal extraction is planned, we irrigate the rectum with water. A Foley catheter is utilized in all cases and intravenous preoperative antibiotics are administered. Ureteral stents are rarely used, except when a large inflammatory process is expected or in select reoperative cases. Digital rectal and/or vaginal exam is performed as necessary during the case and prior to dividing the rectum when treating distal tumors. Intraoperative flexible endoscopy with carbon dioxide is used in our practice routinely both for tumor location and anastomosis evaluation.
Pneumoperitoneum and Port Placement
Pneumoperitoneum can be created in several ways. Entry into the abdominal cavity using either an open technique or by Veress needle has similar complication rates and both are valid starting options. It is our preference to create pneumoperitoneum by introducing a Veress needle at Palmer’s point, right below the left costal margin at the left midclavicular line (MCL). Port location is decided after pneumoperitoneum has been created. This is of particular importance during the robotic part of the procedure, as we will describe later on this chapter.
It is standard in our practice to use a six-port technique during hybrid laparoscopic-robotic LAR, including one 12-mm umbilical port for the camera, two 8-mm left lower quadrant robotic ports, a 12/15-mm right lower quadrant (RLQ) port (an 8-mm robotic port is inserted in a trocar-in-trocar configuration at this location), and two 5-mm laparoscopic ports located in the right upper quadrant (RUQ) and epigastrium (Fig. 23.1b).
The keys to port location are as follows:
A 12-mm camera port (C) is placed in the midline, at the halfway point between the xiphoid process and the pubis symphisis after pneumoperitoneum is completed. Placement could be at, below, or above the umbilicus. However, this trocar should be placed no further than 15 cm from the pubic symphisis. If this port is too high in the abdomen, the camera can hit the sacral promontory as dissection progresses into the pelvis, restricting close approach and visualization of the targets deep in the pelvis.
Once the camera port is in place, a line connecting this port to the right and left anterior superior iliac spine should be drawn. This line will then serve as guidance for the three robotic ports (R) that will be inserted under direct visualization. Maintaining a distance of 8–12 cm between ports (four-finger breadths) is necessary to decrease the risk of arm collision during the robotic stage of the procedure.
R1 is either a 12-mm laparoscopic trocar or 15-mm robotic trocar placed in the RLQ, four-finger breadths away from C. Another way to determine trocar position is by using the halfway point between C and the right anterior superior iliac spine (ASIS) or by selecting the point where the MCL intersects the line that connects C and the ASIS. An 8-mm robotic port needs to be introduced through this port (trocar-in-trocar) to allow for commonly used robotic instruments to be introduced and, therefore arm 1 to function.
R2 is an 8-mm robotic trocar placed in the mirror image of R1 in the left lower quadrant (LLQ). R3 is also an 8-mm robotic trocar placed in the LLQ. It is inserted four-finger breadths apart (8–12 cm), lateral to R2. It is on the same transverse plane, directly above the left ASIS.
Two 5-mm laparoscopic ports (L) are also routinely used in our practice. L1 is located in the RUQ, four-finger breadths lateral to C and about four-finger breadths (about 12 cm) from R1. L2 is inserted in the epigastric area, just lateral (either to the right or left) to the midline, four-finger breadths from L1.
Instruments should always be introduced into the abdominal cavity under direct visualization. They should not be moving outside the field of vision. If an instrument moves outside the field of vision, it should be kept immobile until the camera is repositioned to find the instrument. Trying to blindly bring the instrument into the field of vision can lead to severe patient harm due to the lack of tactile feedback. Minimizing collision between arms is of paramount importance in robotic surgery as it could limit the range of motion of a particular instrument and the ability to reach the targeted structured.
Initial Operative Steps
Once pneumoperitoneum has been created, both surgeon and assistant will stand on the right side of the patient, with the assistant towards the head. The abdominal cavity should be visualized entirely to rule out metastatic disease when treating rectal cancer. Subsequently, the patient is positioned in steep Trendelenburg and rotated to the right. This position facilitates retracting the small bowel and the cecum if necessary, out of the pelvis. If adhesions are present fixing either the small bowel or the cecum in the pelvis, it is of paramount importance to divide them prior to starting the robotic part of the procedure. Due to the lack of haptic feedback from the robotic platform, these structures are at risk of being inadvertently injured unless the surgeon is able to mobilize them out of the pelvis.
Laparoscopic Medial-to-Lateral Dissection of the Left Colon
The RUQ and RLQ ports (L1 and R1 ports, respectively) are the operative ports during the abdominal portion of the operation. The C and L2 ports are controlled by the assistant and an atraumatic grasper in L2 usually aids with retraction. Dissection usually starts in a medial-to-lateral fashion. However, dissection may begin by dividing the peritoneum just distal to the IMA (classic approach) or at the level of the IMV (IMV-first approach).
Starting the dissection at the level of the IMV has the advantage that the avascular plane between the retroperitoneum and the mesocolon is very easy to identify and developed with blunt maneuvers. However, this approach requires excellent exposure of the fourth portion of the duodenum and the ligament of Treitz prior to dissecting. Placing the patient in slight reverse Trendelenburg may help retract the small bowel out of this area. The IMV can usually be easily identified, traveling in a cranial to caudal direction in the mesocolon. This approach requires the small bowel to be displaced away from the LUQ, while the transverse colon should be positioned over the stomach high in the LUQ. Once the inferior mesenteric vein (IMV) is identified, we proceed to grasp the mesocolon (in many cases, the IMV itself is grasped) and gently retract it anteriorly towards the anterior abdominal wall. The peritoneum is then opened with monopolar cautery or hot-scissors just posterior to the IMV and following its course from the ligament of Treitz advancing caudally towards the IMA (Fig. 23.2). Visualization of areolar tissue usually indicates the surgeon is in the correct plane. Dissection progresses with blunt maneuvers since this is an avascular plane and allows the surgeon to mobilize the IMV and mesocolon off the retroperitoneum. Dissection advances laterally towards the lateral abdominal wall and towards the splenic flexure. Gerota’s fascia is encountered and dissected down and away from the mesocolon. Caudally, the limit of the dissection is the IMA itself. The IMV can be divided at any point; although it is preferable to complete the dissection first, as this structure helps generate counter-traction (Fig. 23.3). Our preference is to clip it proximally and then divide it using a vessel sealer, preferable a bipolar device. Conversely, the IMV can be divided in between clips or using a vascular endostapler.
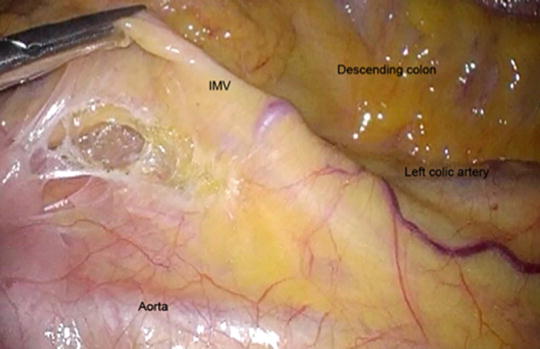
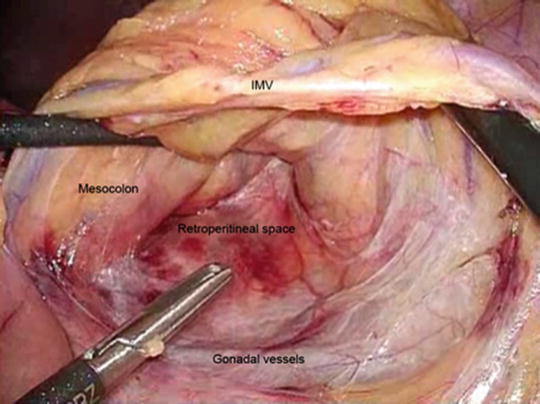
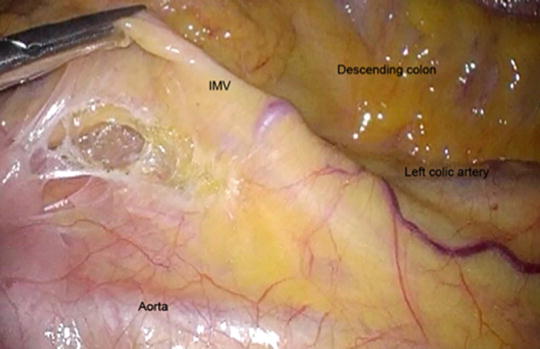
Fig. 23.2
Dissection starting at the level of the inferior mesenteric vein. As the vein is gently grasped and lifted, the peritoneum is divided and the space between the mesocolon and the retroperitoneum is entered
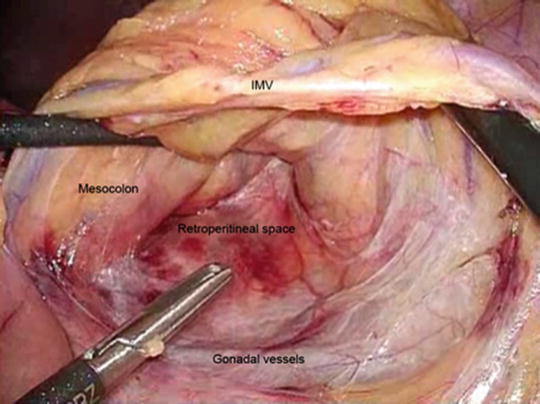
Fig. 23.3
Development of the plane between the descending mesocolon and the retroperitoneum
The lesser sac can be entered by continuing the dissection in the IMV plane. This maneuver may facilitate taking down the splenic flexure. However, this plane naturally continues under the pancreas. Therefore, carrying the dissection in this plane towards the LUQ will lead to lifting the pancreas along with the transverse mesocolon (Fig. 23.4). Unless clearly identified, our recommendation is not to continue towards the LUQ. Take-down of the splenic flexure and access to the lesser sac should be accomplished in a more traditional manner, after dividing the line of Toldt during the lateral to medial part of the procedure.
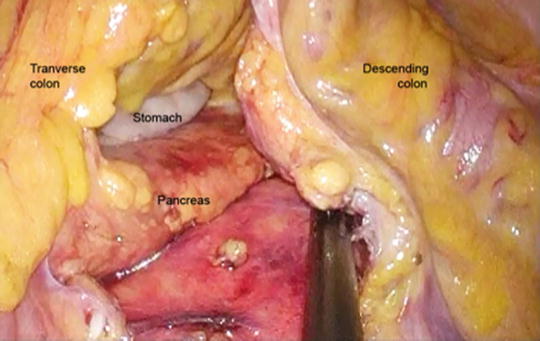
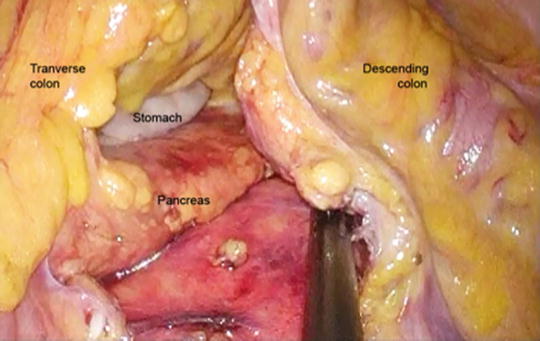
Fig. 23.4
Dissection towards the left upper quadrant after dividing the IMV allows access to the lesser sac. The pancreas and the stomach are observed in this picture
Dissection then continues, once the IMA has been identified, by gently lifting the superior hemorrhoidal pedicle towards the anterior abdominal wall. The parietal peritoneum below the superior hemorrhoidal artery is then divided advancing towards the sacral promontory. Blunt dissection allows entry into the same avascular plane that was developed before. From a practical standpoint, the surgeon should visualize the dissection area as a square where the floor is the retroperitoneum containing nerves and the iliac vessels and the roof is the superior hemorrhoidal artery. The left (cranial) “wall” demarcating this square is the IMA and the right (caudal) “wall” is the mesorectum (Fig. 23.5). Dissection is performed within this square in a medial to lateral fashion. As the gonadal vessels and the ureter are encountered, they should be dissected posteriorly towards the retroperitoneum. Visualization of the psoas muscle is usually indicative of a dissection that has proceeded in the wrong plane. The surgeon should reevaluate the plane of dissection; typically, both gonadal vessels and ureter have been inadvertently lifted with the mesocolon.
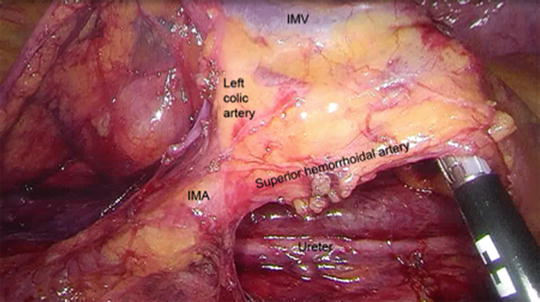
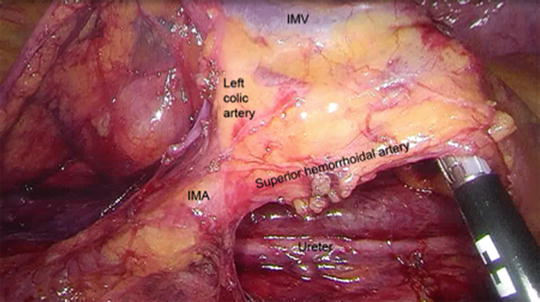
Fig. 23.5
Medial-to-lateral dissection reveals the IMV and IMA
A common mistake that makes identification of the ureter difficult is starting the dissection through a small peritoneal opening. Starting the dissection by dividing the peritoneum from the IMA all the way to the rectum facilitates this part of the procedure. While keeping in mind the boundaries of the “square”, creating a larger peritoneal opening allows for a larger area of blunt dissection and makes identification of the gonadal vessels and ureter easier. Care should be taken during this part of the procedure not to injure the hypogastric nerve plexus. Division of the IMA should not be performed prior to identification of these structures.
Once the peritoneum has been opened all the way from the IMV down to the mesorectum, a very characteristic “T” shaped configuration should be visualized as the mesocolon is retracted upwards towards the anterior abdominal wall. The IMA constitutes the vertical part of the “T”, while its two branches, the left colic artery to the left and the superior hemorrhoidal artery to the right, form the horizontal parts (Fig. 23.5).
It is important to emphasize that the left ureter travels lateral just against the IMA and can be lifted and injured when attempting to divide the IMA if the dissection is not adequate. Therefore, the IMA should not be divided prior to visualization of the ureter. The IMA can then be divided in a number of ways, such as using a vessel sealing device, clips, or endostapler with a vascular load. We routinely clip the IMA prior to using an advanced bipolar device.
Splenic Flexure Takedown
Once the medial-to-lateral dissection has been completed and both the IMA and IMV divided, the lateral attachments of the sigmoid and descending colon are taken down. The line of Toldt is divided with monopolar cautery, hot-scissors, or advanced bipolar device. Dissection usually starts at the LLQ and is facilitated by retracting the colon towards the midline. As the line of Toldt is divided, blunt maneuvers are also used as the initial medial dissection plane is easily encountered. As dissection progresses towards the LUQ, attachments from the omentum to the lateral abdominal wall and to the descending colon can be present. We usually divide the attachments to the colon, leaving those attachments between the omentum and the abdominal wall in place, unless they obstruct adequate visualization of our plane of dissection. Taking down the splenic flexure can be challenging from a technical standpoint. If progress stalls, approaching the splenic flexure from the transverse colon may make this part of the operation less cumbersome. In this case, the omentum is then divided off the distal transverse colon usually using a bipolar device. As dissection progresses, both the phrenocolic and splenocolic ligaments are encountered and divided. As the lesser sac is entered, mobilization of the colon is carried out at the base of the mesentery and allows for complete mobilization of the splenic flexure, a necessary step to be able to construct a tension-free anastomosis.
Robotic Total Mesorectal Excision
It is our practice to perform the mesorectal dissection using a four-arm Da Vinci robot (Intuitive) docked at the patient’s left hip. At the time of docking, the patient is in Trendelenburg and rotated to the right in such a way that the small bowel and right colon remain outside the pelvis. The central column of the Da Vinci cart is in-line with the patient’s left ASIS and the right shoulder. Rectal procedures can also be completed by docking the robot in between the legs. However, intraoperative digital or endoscopic rectal examinations are difficult with this approach.
A 0-degree, 12-mm robotic camera is introduced in C. Although available, we rarely use a 30-degree camera. Arm 1 is docked to R1 and will be the access site later in the procedure for stapler devices. Laparoscopic staplers require a 12-mm port, while the robotic articulating stapler requires the use of a 15-mm robotic trocar in this location. An 8-mm robotic trocar using a trocar-in-trocar technique is required to use this port during dissection. A robotic hook or monopolar scissors is usually introduced through this port. A robotic bipolar fenestrated grasper is placed in Arm 2 and docked in R2, while Arm 3 is docked in R3 with a Prograsp (Intuitive). The assistant will remain on the right side of the patient generally using an extended-length suction irrigator in L1 and a locking grasper in L2. The suction-irrigator will play an important role generating counter-traction throughout the case.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








