Fig. 1
Inguinal hernia. a Oblique scan of inguinoscrotal region showing the inguinal hernia containing omentum (OM) and bowel (BO). The testis (T) is undescended and located in the inguinal canal. b Transverse scan of left inguinal region showing the hernial sac (HER) located medial to the inferior epigastric vessels (arrow) in direct inguinal hernia. c Indirect inguinal hernia on left side with the neck of sac located lateral to inferior epigastric vessels (arrow). d Oblique scan in a premature infant showing the inguinal hernia containing the fallopian tube (FT) and ovary (OV). e Oblique scan of an infant showing inguinal hernia containing part of the urinary bladder (arrows). BL urinary bladder, UT uterus
The inguinal hernia can be associated with conditions like hydrocele, varicocele, or mass of the cord, like an encysted hydrocele or lipoma, which are readily diagnosed by sonography. In male children, an indirect inguinal hernia may be associated with undescended testis. The testis may be lying by the side of the sac in the inguinal canal (Fig. 1a), or it may be intraabdominal. This information helps to avoid causing injury to the testis during surgery and to combine orchidopexy during repair. In females the inguinal hernia may contain ovary, fallopian tube, or rarely, the uterus, which are easily identified on sonography (Fig. 1d, Huang et al. 2003). The hernia containing these organs is common in premature infants (George et al. 2000). Very rarely, the urinary bladder may form the content of a sliding type of inguinal hernia (Fig. 1e, Catalano 1997).
1.2 Femoral Hernia
Femoral hernia occurs through a space bounded superiorly by the iliopubic tract, inferiorly by the Cooper’s ligament, laterally by the femoral vein and medially by the insertion of the iliopubic tract into Cooper’s ligament. It is more common in females than in males. On examination it reveals a mass below the inguinal ligament. On sonography, the femoral hernia is seen posterior to the inguinal ligament and medial to the femoral vein, in contrast to the inguinal hernia, which is anterior to the inguinal ligament. (Fig. 2, Deitch and Soncrant 1981; Dattola et al. 2002).
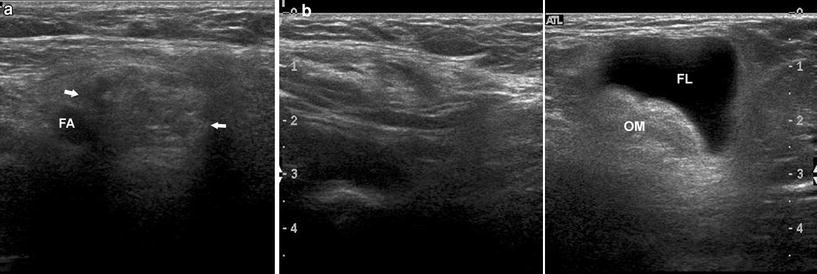
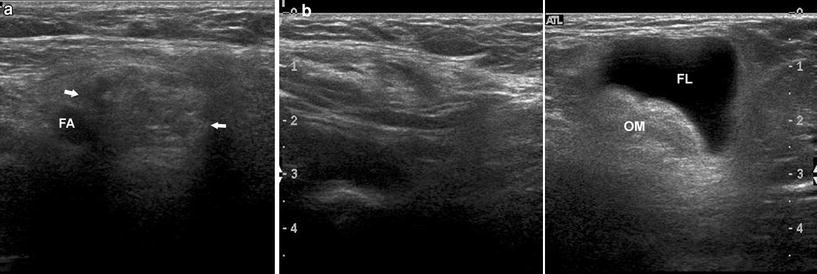
Fig. 2
Incarcerated femoral hernia. a Transverse scan at the level of the femoral vessels of right side showing the neck of the sac containing omentum (arrows) medial to the femoral artery (FA). The femoral vein is not visualized as it is compressed. b Longitudinal scan showing the echogenic omentum (OM) in the sac with fluid (FL) due to incarceration
1.3 Ventral Hernia
Ventral hernia covers all protrusions through anterior and anterolateral abdominal wall, excluding groin hernias. It is suggested by the patient’s clinical history and is well seen on physical examination; however, the patient’s history may be atypical and physical examination may be limited in obese patients, in patients with severe abdominal pain or distension, in small hernias or with hernias located in uncommon sites (Spangen 1975; Mufid et al. 1997). In certain clinical situations, it may be necessary to relate the symptoms to the ventral hernia or, it may be necessary to know whether the ventral hernia is complicated or not. In these situations an imaging investigation becomes necessary. Sonography is a dynamic, noninvasive, easily available, and low cost modality useful in studying the ventral hernia. It is performed at rest and during a maneuver such as Valsalva, cough, or erect position. Sonographic diagnosis of ventral hernia is made when bowel or other abdominal organs or fatty tissue of the abdominal wall is seen protruding out of the abdomen with continuity within the abdomen. (Rettenbacher et al. 2001). The hernial orifice is seen as a defect in the fascia, which is seen as an echogenic line deep to the muscle layer and its location and width can be noted. Sonography reveals the contents, which can be omentum, bowel (Fig. 3a), or properitoneal fat (Fig. 3b). Some ventral hernias are not seen at rest and are brought into view with only one of the maneuvers. When the hernia is seen at rest, an attempt is made to slide the contents into the abdomen to know if the hernia is reducible (Video 2). Sonography readily differentiates other conditions that mimic ventral hernia such as lipoma, metastasis, suture granuloma, abscess, or endometriosis. Umbilical hernia is a type of ventral hernia that occurs through the weak umbilicus. Fatty epigastric hernia is protrusion of the properitoneal fat through a defect in the linea alba.
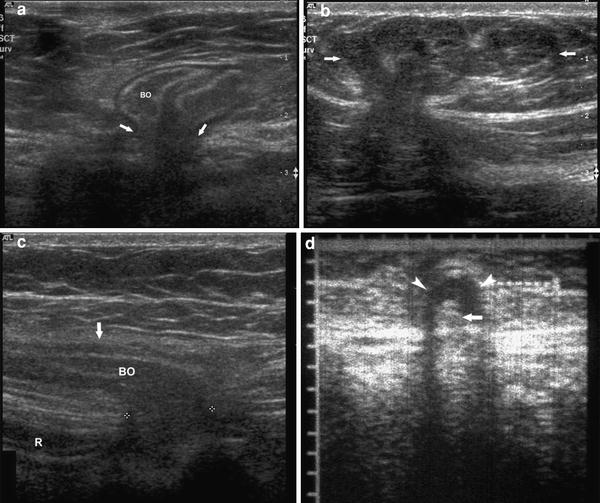
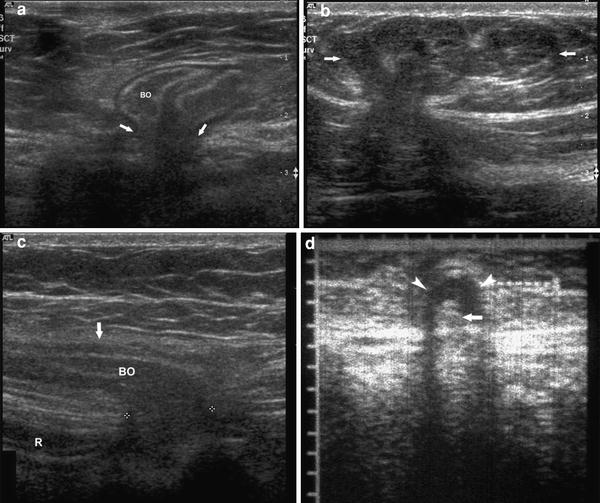
Fig. 3
a Scan of the anterior abdominal wall with Valsalva maneuver showing the ventral hernia containing the bowel loops (BO) and the defect in the fascia (arrows). b Fatty epigastric hernia with herniation of the properitoneal fat (arrows). c Spigelian hernia showing the defect marked by calipers lateral to the rectus muscle (R) and the contents (BO) limited anteriorly by the Spigelian fascia (arrow). d Richter’s type umbilical hernia showing fluid filled hernial sac (arrowheads) and irreducible herniation of only a part of the circumference of the bowel (arrow) which showed wriggling peristaltic movement on real time
1.4 Spigelian Hernia
Spigelian hernia is a rare type of ventral hernia in which the abdominal contents protrude through an area of weakness at the junction of linea semilunaris and linea semicircularis (Sutphen et al. 1980). The linea semilunaris is a vertical band-like groove that is formed by the union of the medial edges of the aponeuroses of the external oblique, internal oblique, and transverse abdominal muscles. In its upper 75 %, the fused aponeurosis of these three muscles splits medially to form the anterior and posterior rectus sheaths. Midway between the umbilicus and symphysis pubis, the aponeurosis of the three lateral abdominal muscles passes medially to cover only the anterior surface of the rectus muscle, leaving the posterior surface of the lower fourth covered only by the transversalis fascia and peritoneum. The line forming the inferior margin of the rectus sheath is called the linea semicircularis. Also, at this level, the fiber bundles of the transverse abdominal and internal oblique muscles are much thinner and more widely spaced, causing further weakening through which omentum and small intestine could potentially protrude. Spigelian hernias occur with equal frequency in men and women and in every age group (Mufid et al. 1997). Spigelian hernias may not appear as distinct masses, making them difficult to diagnose clinically. This is because these hernias always dissect between the layers of the anterior abdominal wall, rather than in the subcutaneous tissues, as other ventral hernias do. Spigelian hernias have been mistaken for abdominal abscesses, seromas, hematomas, ovarian masses, pseudocysts, and malignant omental or peritoneal implants (Wechsler et al. 1989).
On sonographic examination during the Valsalva maneuver or erect position, intraabdominal contents, including bowel, mesentery, and omentum, is seen to herniate through a defect in the left lower quadrant abdominal wall in the space between the rectus muscle medially and the external and internal oblique muscles laterally. The hernia extends medially anterior to the rectus muscle (Fig. 3c). The Spigelian fascia, which prevents its extension into the subcutaneous tissue, limits it anteriorly (Mufid et al. 1997). These hernias are also associated with a higher risk of bowel incarceration and strangulation than other abdominal wall hernias.
1.5 Richter’s Hernia
In Richter’s hernia, only part of the circumference of the bowel on the ante mesenteric border protrudes into a hernia. It can occur with any type of abdominal wall hernia but is more common in femoral hernia. The symptoms and clinical course vary widely, depending on the degree of obstruction, or if strangulation is present. In strangulation, the patient presents with a painful mass, nausea, and vomiting. In contrast to other types, there is no abdominal distention as there is no bowel obstruction. On sonography, complicated Richter’s hernia is seen as a small segment of bowel showing wriggling movement in the neck of the hernial sac, which contains fluid (Fig. 3d). There are no dilated bowel loops in the abdomen (Middlebrook and Eftekhari 1992; Hiller et al. 1994).
If strangulated Richter’s hernia is not relieved there may be perforation of the small part of the circumference of the small bowel which may present as abscess in the abdominal wall (Fig. 4).
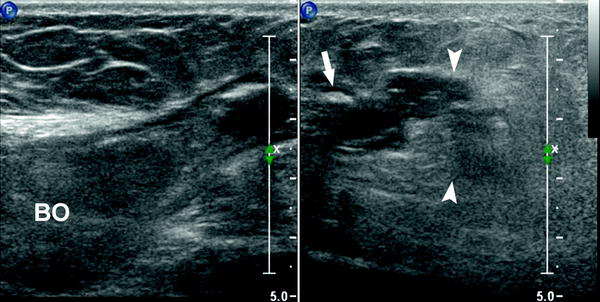
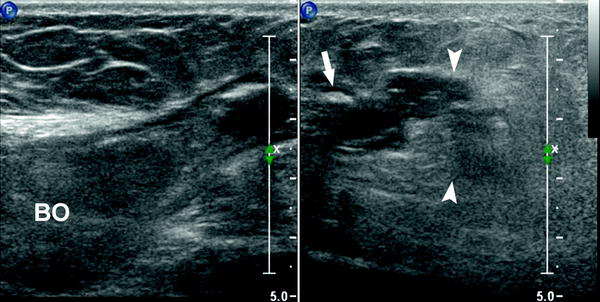
Fig. 4
Complicated Richter Hernia. Oblique scan of the periumbilical region of the abdominal wall showing herniation of a part of the circumference (arrow) of the intraabdominal bowel loop (BO) into the umbilical hernia. There is an abscess (arrow heads) close to the breach in the wall of the bowel
1.6 Obturator Hernia
Obturator hernia occurs through the obturator foramen in pelvis which contains the obturator nerve and vessels. It is bounded superiorly and laterally by the pubic bone and inferiorly by the obturator membrane. Obturator hernia is nine times more common in females. It occurs most frequently in emaciated patients aged >70 years. It is rarely diagnosed clinically as there is no external hernia.
It is usually diagnosed at laparotomy done for small bowel obstruction. It can be diagnosed on sonography, when there is small bowel obstruction.
On axial scan of the inguinal region, it is seen as an echo poor mass deep to the pectineus muscle. It is much deeper in relation to the common femoral vessels.
On longitudinal scan the upper limit will not be seen (Fig. 5).
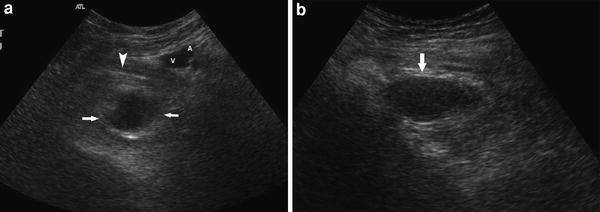
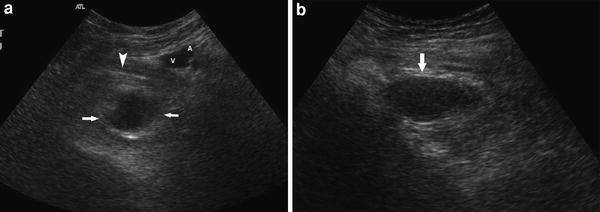
Fig. 5
Obturator Hernia. a Transverse scan of the left inguinal region showing the loop of bowel (arrows) deep to the pectineus muscle (arrow head) and far deep to the common femoral artery (A) and Vein (V). b Longitudinal scan showing the herniated loop (arrow), the upper limit of which is not well defined
1.7 Complications of Hernia
The pattern of complications is common for all types of hernia. The complications are irreducibility, obstruction, and strangulation. Irreducible (incarcerated) hernia may be due to a narrow neck or adhesion of contents to the sac wall. In obstruction, the intestine in the hernia gets obstructed due to a narrow neck, adhesion or volvulus, but it is viable. Strangulation results when there is compromise to venous drainage and later arterial supply of the contents. In obstructed hernia there is colicky pain, abdominal distension, and vomiting. Incarcerated hernia is present at rest; it is irreducible and usually contains some fluid in the sac that can be seen on sonography (Fig. 2b, Rettenbacher et al. 2001). In obstructed inguinal hernia the patient has symptoms of intestinal obstruction. There are dilated bowel loops in the abdomen which show active peristalsis. The appearance of the bowel in the hernial sac depends on whether the obstruction is to afferent or efferent loop in the sac. In the more common afferent loop obstruction, the bowel loops in hernial sac remain collapsed and there is transition between the dilated intraabdominal bowel loop and collapsed bowel loop in the hernia (Fig. 6a). In efferent loop obstruction, the bowel loop in the hernial sac is dilated. The transition is between dilated loop in hernial sac and collapsed loop in abdomen (Fig. 6b). The obstruction may be of closed loop type due to block of both the afferent and efferent loops at the neck of the hernia, or due to volvulus of the loop in the hernial sac. Here, the loop of bowel in hernial sac is disproportionately more dilated than proximal intraabdominal loops, it is tensely distended and may lack air in its lumen (Fig. 6c). The peristalsis is usually absent in this loop as it is tensely distended. In strangulation there is ischemia of the contents of the hernia. The hernia is tender, with free fluid in the sac. The wall of the aperistaltic bowel is thickened (Fig. 6d). On color Doppler study, no flow is seen in the omentum or bowel, which is strangulated (Liang et al. 2001). In the case of the bowel, dilated loops of bowel are seen in the abdomen.
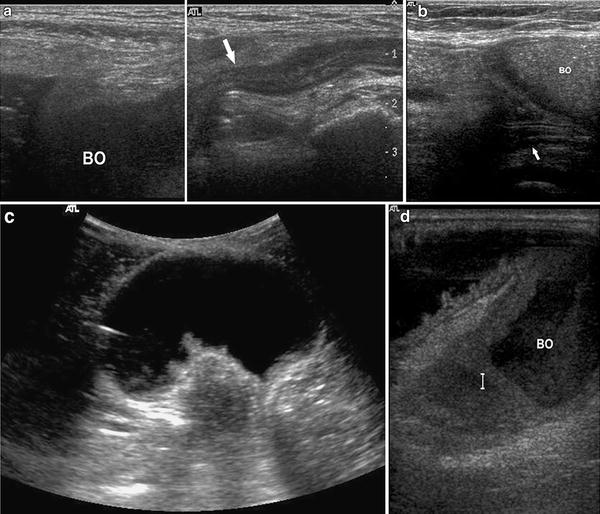
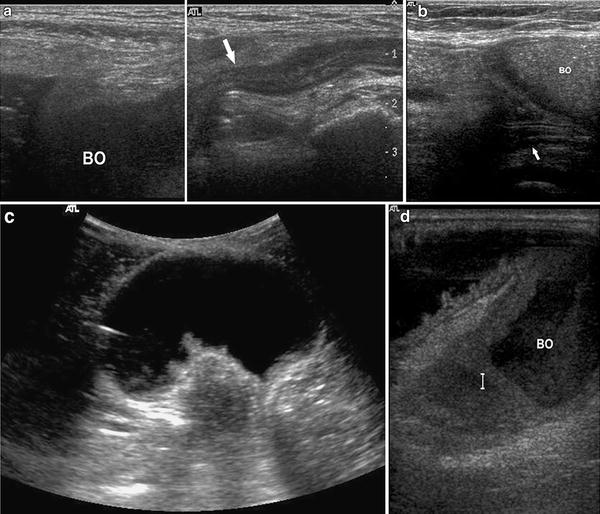
Fig. 6
Complicated hernia. a Afferent loop obstruction showing the transition between the dilated intraabdominal loop (BO) and collapsed loop in inguinal hernia (arrow). b Efferent loop obstruction showing dilated bowels in ventral hernia (BO) with transition between the dilated loop in hernia and collapsed intraabdominal loop at the neck of the sac (arrow). c Tensely distended loop devoid of air in a ventral hernia due to closed loop obstruction. d Strangulated loop of bowel (BO) in a ventral hernia showing thick walls
1.8 Postoperative Sonography
Sonography is useful in postoperative follow-up of the patients with hernia. The prosthetic mesh can be seen as a brightly echogenic reticular line and curled prosthesis (Fig. 7a) or a displaced prosthesis can be recognized (Parra et al. 2004; Dattola et al. 2002). Fluid collection (seroma or abscess) is well seen and its relation to prosthesis can be assessed (Fig. 7a). If necessary, the fluid can be aspirated under sonographic guidance (Parra et al. 2004). Adhesion of bowel to the prosthesitic mesh is one of the complications that can lead to bowel obstruction. Sonography can reveal dilated loops and the bowel loop adherent to the mesh (Fig 7b, Furtschegger et al. 1995). Recurrence of hernia can be confirmed and the location of defect in relation to the mesh can be known. In the case of inguinal hernia, the vascular supply to the testis can be assessed by color Doppler study, and testicular ischemia or infarction may be recognized (Holloway et al. 1998).
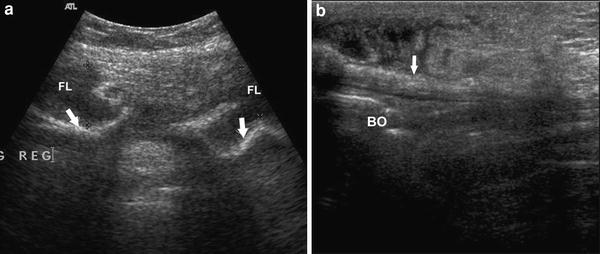
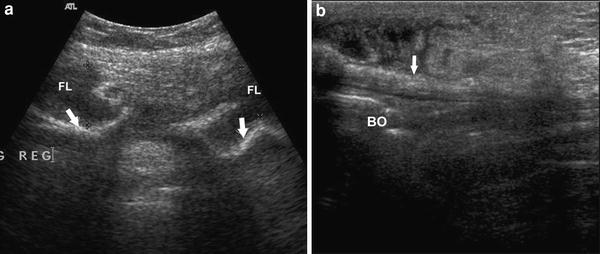
Fig. 7
Scan of the abdominal wall after hernial repair showing the curled echogenic mesh (arrows) with collection of fluid (FL) anterior to it in a and bowel (BO) adherent to the straight mesh (arrow) in b
1.9 Internal Hernia
Internal hernia involves protrusion of a viscus, usually the small bowel, through a normal or abnormal aperture within the peritoneal cavity. Internal hernias are rare, with reported incidence of 0.2–0.9 % of autopsies (Ghahremani 1984). A substantial proportion of these remains asymptomatic. It is an uncommon cause of small bowel obstruction. About 4 % of bowel obstruction is due to internal hernia (Feldman et al. 2002). Owing to the risk of strangulation of the contents of the hernia, even small internal hernias are dangerous and may be lethal. This hernia may be either congenital or acquired. Congenital internal hernias include paraduodenal, foramen of Winslow, mesenteric, and supravesical hernias. During fetal development, the mesentery of the duodenum, ascending colon, and descending colon becomes fixed to the posterior peritoneum. These segments of the bowel became retroperitoneal. Anomalies of mesenteric fixation may lead to abnormal openings through which internal hernias may occur. This is the likely mechanism of paraduodenal and supravesical hernias. Abnormal mesenteric fixation may lead to abnormal mobility of the small bowel and right colon, which facilitates herniation. During fetal development, abnormal openings may occur in the pericecal, small bowel, transverse colon, or sigmoid mesentery, as well as in the omentum, leading to mesenteric hernias. In the case of left paraduodenal hernia, an abnormal foramen (fossa of Landzert) occurs through the mesentery close to the ligament of Treitz, leading under the distal transverse and descending colon and posterior to the superior mesenteric artery. The small bowel may protrude through this fossa. The mesentery of the colon thus forms the anterior wall of a sac enclosing a portion of the small intestine. Mesenteric hernias occur when a loop of intestine protrudes through an abnormal opening in the mesentery of the small bowel or the colon. The most common area for such an opening is in the mesentery of the small intestine, most often, near the ileocolic junction. Various lengths of intestine may herniate, posterior to the right colon, into the right paracolic gutter. Acquired internal hernias may occur as a complication of surgery, or trauma, if abnormal spaces or mesenteric defects are created. Compression of the loops in the internal hernia may lead to obstruction of the herniated intestine. Obstruction may be acute, chronic, or intermittent. Strangulation may occur by compression of vessels at the neck of the sac, or by torsion of the herniated segment. The herniated bowel may also compress arteries in the margins of the mesenteric defect, causing ischemia of non herniated intestine.
Any of the various forms of internal hernias may present with symptoms of acute or chronic intermittent intestinal obstruction. The diagnosis is difficult among patients with chronic symptoms and is rarely made preoperatively among patients who present with acute obstruction (Ghahremani 1984). About 50 % of patients with paraduodenal hernias develop intestinal obstruction, which may be of low grade, chronic, and recurrent, or may be of high grade and acute (Zimmerman and Laufman 1953; Nyhus and Condon 1989; Pershad et al. 1998). In acute bowel obstruction, the patients present with colicky abdominal pain with vomiting. The features seen on sonography are: (a) small bowel obstruction, as evidenced by dilated hyperperistaltic loops (b) zone of transition between dilated and nondilated bowel and, (c) cluster of collapsed, crowded, and compressed small bowel loops, as if enclosed in a bag (Fig. 8). This cluster of loops is seen away from the zone of transition: to the left in paraduodenal hernia and to the right in paracecal hernia. These are the features seen when the afferent loop entering the sac is obstructed because of crowding and compression of bowel loops in the sac. When there is obstruction to the efferent loop at the neck, the sac contains dilated loops of small bowel with the zone of transition at the neck of the sac (Vijayaraghavan 2005). The differential diagnosis for sonographic appearance of internal hernia is abdominal cocoon. In abdominal cocoon there is no evidence of small bowel obstruction or zone of transition. The loops do not appear to be compressed and show normal peristalsis (Vijayaraghavan et al. 2003).
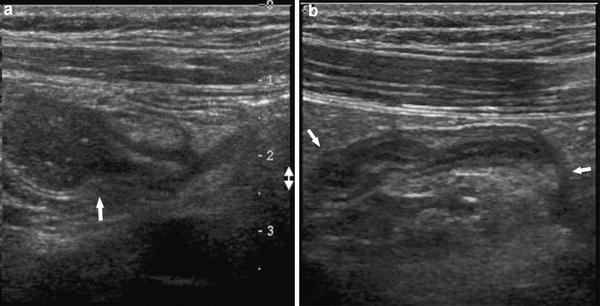
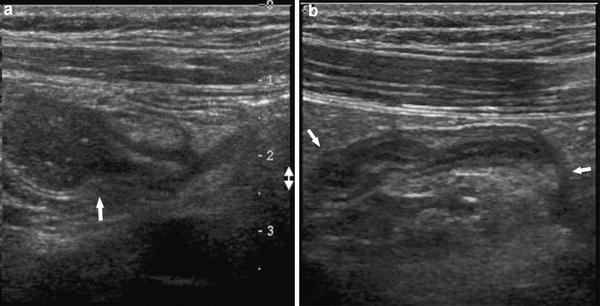
Fig. 8
Paraduodenal internal hernia. a Oblique scan above the umbilicus showing the zone of transition (arrow) between dilated and non dilated bowel. b Transverse scan to the left of zone of transition shows the cluster of crowded and compressed loops of bowel as if they are tightly packed within a sac (arrows)
1.10 Diaphragmatic Hernia
The diaphragmatic hernia is an abnormal protrusion of abdominal organs into the chest through an abnormal opening in the diaphragm or through the esophageal hiatus. The abnormal opening may be congenital, caused by improper fusion of the various parts of diaphragm during fetal development, or acquired, due to traumatic rupture of the diaphragm. The four basic types of congenital diaphragmatic hernia are the posterolateral Bochdalek hernia, the anterior Morgagni hernia, the hiatus hernia, and the rare form of herniation through the central tendon or septum transversum, otherwise called the peritoneopericardial hernia. The left-sided Bochdalek hernia is the commonest of these occurring in approximately 90 % of the cases. The congenital diaphragmatic hernia occurs in one of every 2,000–4,000 live births. While congenital diaphragmatic hernia is most commonly a disorder of the newborn period, as many as 10 % of patients may present with the condition after the newborn period and even during adulthood. The outcome in patients with late presentation of congenital diaphragmatic hernia is extremely good. During newborn period, the infants exhibit respiratory distress and cyanosis. In later age groups the condition is asymptomatic, or presents with nonspecific symptoms.
The diagnosis of left-sided congenital diaphragmatic hernia in the newborn is revealed on a chest X-ray, as it contains air-filled bowels. The right-sided hernia containing solid liver or right kidney may be difficult to diagnose on a chest X-ray. Sonography reveals the defect in the right dome of the diaphragm and the herniated liver or right kidney. In the rare type of peritoneopericardial hernia, there is herniation of the left lobe of the liver with, or without colon, into the pericardial sac through a defect of the central tendon of the diaphragm. This hernia also presents in the newborn period as respiratory distress or cyanosis. In such a case, an X-ray of the chest will reveal an enlarged cardiac silhouette. Sonography reveals the herniation of left lobe of liver into the pericardial sac containing some pericardial fluid (Fig. 9a, Vijayaraghavan 1988). The herniated liver pushes the heart above and laterally. The diaphragmatic hernia of Bochdalek type, presenting in later ages, may be seen on sonography as a defect in the diaphragm with intrathoracic visualization of viscera such as stomach, spleen, and bowels, on the left side (Fig. 9b), and liver or right kidney on the right side.
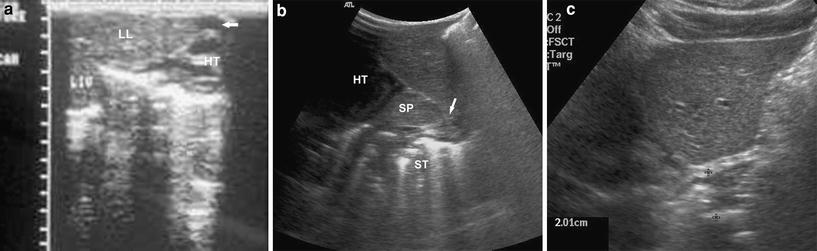
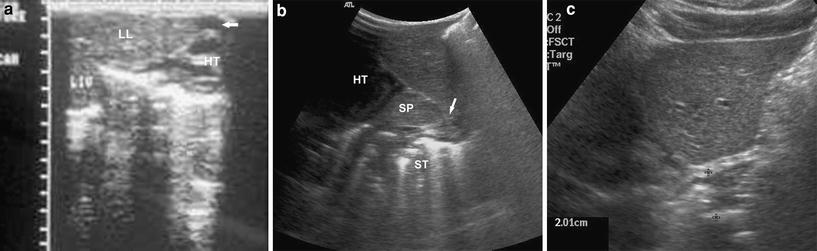
Fig. 9
a Oblique scan of epigastrium and precordium showing the left lobe of the liver (LL) herniated into the pericardium pushing the heart (HT) better outlined by the minimal pericardial fluid (arrow). LIV intraabdominal liver. b Longitudinal scan of left hypochondrium revealing the defect (arrow) in the posterior part of left dome of diaphragm with spleen (SP) and air filled stomach (ST) lying in the chest posterior to the heart (HT) suggestive of left diaphragmatic hernia of Bochdalek type. c Longitudinal scan of left hypochondrium showing the shortened and thickened intraabdominal esophagus in gastro esophageal reflux of hiatus hernia
In the hiatus hernia, the stomach herniates up through the esophageal hiatus of the diaphragm. There are two types of hiatus hernia. In the sliding type, the gastroesophageal junction and fundus of stomach slide through the hiatus and are situated above the diaphragm. It is associated with gastroesophageal reflux. In the rolling or para esophageal type, the gastroesophageal junction is in the abdomen, and the fundus of stomach herniates by the side of the esophagus. Many authors have described the sonographic findings associated with the gastroesophageal reflux caused by the hiatus hernia in children (Naik and Moore 1984; Westra et al. 1990; Le Dosseur et al. 1992). Sonography is performed after the usual feed of formula, milk, water, or juce. The transducer is placed in the midline under the xiphisternum and the distal esophagus is visualized, as it comes out of the diaphragm. The transducer is slightly rotated to obtain the longitudinal section of the intraabdominal portion of the esophagus and observed for 10 min. The length of the esophagus is measured from the diaphragm to the cardia and the thickness is measured between the serous layers. The number of episodes of gastroesophageal reflux is also noted. Normal values for these observations have been described for the different age groups of children (Westra et al. 1990; Le Dosseur et al. 1992). Aliotta et al. (1994) have described the thickness of the hiatal portion of the esophagus in adults indicative of hiatus hernia as 16 mm or more (Fig. 9c).
2 Small Bowel Volvulus
Small bowel volvulus refers to rotation of the bowel around the mesenteric axis, which often results in a closed loop obstruction, lymphatic, venous, or arterial occlusion (Fig. 10a). It is one of the conditions causing small bowel obstruction, which requires prompt diagnosis and treatment to avoid poor outcome, as it can progress rapidly to gangrene of bowel. It is a rare but a life-threatening emergency. It is more common in Africa (24–60/100,000) and Asia, compared with Western countries (1.7–5.7/100,000; Gulati et al. 1973; Cathcart et al. 1981; Schwartz and Ellis 1989; Parkes 1997). The small bowel volvulus can be primary or secondary depending on whether a predisposing factor is present or not. Predisposing condition may be congenital or acquired. Malrotation of midgut, a persistent omphalalomesenteric duct and mesenteric cyst are some of the congenital conditions. Some of the acquired conditions are adhesion, ascariasis and a mesenteric cyst, or tumor. In malrotation of midgut, there is arrest of the rotation and fixation phase of embryonic development, which results in developmental failure of peritoneal fixation and a narrow mesenteric pedicle. The narrow mesenteric pedicle predisposes to volvulus because of increased mobility. Increase in the weight of the distal aspect of mesentery due to a mesenteric cyst or tumor, a mass of ascaris worms and dilated loop of bowel in a closed loop obstruction can predispose to volvulus,. The third factor, which predisposes volvulus, is restriction of the bowel at a fixed point, which acts as a fulcrum for rotation. The point of fixation may be at the apex of the volvulus, as seen in persistent omphalalomesenteric duct and adhesion of bowel to abdominal wall or it may be at the base, as seen in adhesions between two loops of bowel with volvulus occurring at this site. Volvulus in malrotation of midgut typically presents in the neonatal period, but can also occur at a later age and even in adults. The volvulus due to other causes may occur at any age. The clinical presentation of volvulus of small bowel can be nonspecific and includes bilious vomiting, abdominal pain, and distension. Some patients may have chronic or intermittent symptoms.
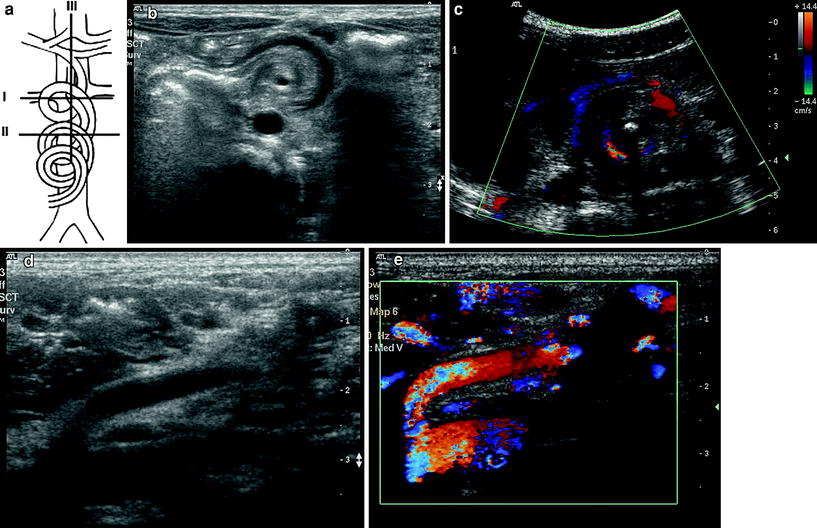
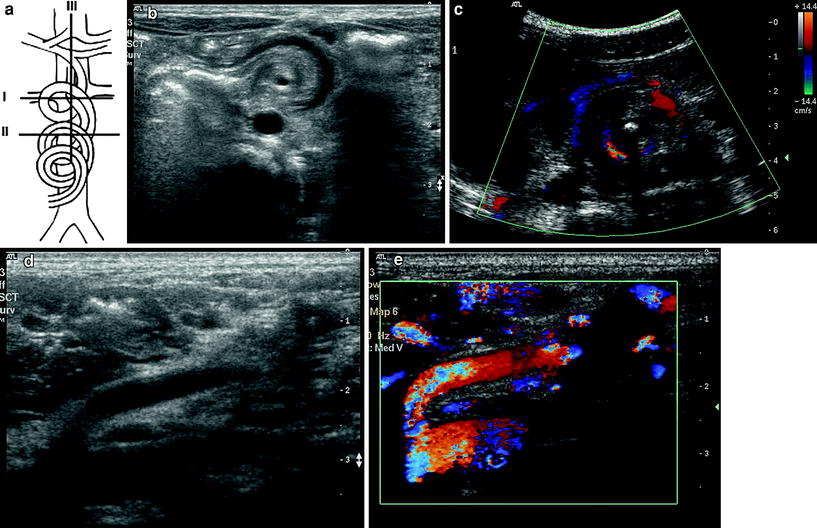
Fig. 10




Small bowel volvulus in malrotation of midgut. a Line diagram showing the rotation of vessels and planes of section. b Transverse section through plane I showing the mass of whirlpool with its axis formed by superior mesenteric artery seen as a hypoechoic dot. c Similar section through II with color Doppler showing the mass of whirlpool with the superior mesenteric vessels going around the central echogenic axis formed by wrapped up omentum. d Longitudinal section through superior mesenteric artery (plane III) shows the truncated superior mesenteric artery sign. e The same appearance on color Doppler study
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








