Groin Hernia Repair/Kugel Technique
John T. Moore
Introduction
Hernia repair constitutes a major part of the typical general surgical practice. Expansive literature has been produced demonstrating benefits associated with a large number of repairs. Most of these repairs have focused on tension-free techniques. Tension-free repairs, when performed properly, reduce the risk of recurrence to low levels. These repairs also reduce postoperative pain and accelerated return to normal activity. Surgeons have been exposed to many mesh-designed tension-free repairs. In order to achieve the published results of these repairs, proper performance of the technique selected is the key element. These techniques require a thorough understanding of the procedures used as well as a thorough understanding of groin anatomy.
The Kugel technique for groin hernia repair is a tension-free minimally invasive, yet open, preperitoneal or posterior abdominal wall groin hernia repair. It is applicable to the treatment of indirect and direct inguinal hernias as well as femoral hernias. It is particularly useful for the treatment of recurrent groin hernias after previously failed anterior repair. It can be used selectively in patient’s having undergone prior radical prostatectomy or pelvic radiation, but should be avoided in patients with recurrence after a failed laparoscopic groin hernia repair. This technique allows for rapid return to regular work and other activities without restriction. It further minimizes the risk of nerve injury and associated burdensome chronic pain syndromes because the inherent nature of this repair is to avoid direct nerve injury and avoid exposure of the groin nerves to the mesh.
Patient Selection
The key elements in successful hernia surgery are proper patient selection and proper performance of the repair. However, not all patients with hernias need to be repaired.
Elderly, debilitated, and inactive patients with asymptomatic hernias where the hernia is easily reduced may be best left alone with rare exceptions. Symptomatic patients should all be repaired promptly. Even here, postponement of the repair may be considered if the symptoms are minimal and the hernia is easily reduced. Factors to consider are cost (immediate and delayed), age, patient’s health, and type of work. There is no question delaying a repair may create a much more different repair later with more complications. Incarceration also is a rare threat.
Elderly, debilitated, and inactive patients with asymptomatic hernias where the hernia is easily reduced may be best left alone with rare exceptions. Symptomatic patients should all be repaired promptly. Even here, postponement of the repair may be considered if the symptoms are minimal and the hernia is easily reduced. Factors to consider are cost (immediate and delayed), age, patient’s health, and type of work. There is no question delaying a repair may create a much more different repair later with more complications. Incarceration also is a rare threat.
Not every patient with groin pain needs surgery. The groin area is particularly susceptible to injury. Muscle and ligamentous tears and strains can cause groin pain and even result in chronic pain, which will not improve with the hernia operation. Very small and occult hernias do exist and can be particularly difficult to diagnose, especially femoral hernias. These can cause pain in patients, but in the absence of clear physical findings for a hernia observation seems to be the best initial course. Special caution in patients is also warranted with a very short history of symptoms or a very long history of symptoms, who do not demonstrate positive physical findings of a hernia. Ultrasound in these patients is sometimes helpful, but frequently overstates the presence of a hernia. The ultrasound also does not correlate well with the symptomatology. A wait and see approach is advised in these patients. If the surgeon is to avoid the not uncommon patient complaint after surgery that “the pain is worse now than before the surgery” or even “the mesh must be causing the pain.”
While the bias of this presentation is that the Kugel technique is useful for the majority of groin hernias, there are incidences where it would be inappropriate (see “Indications”) and even instances where it might not be the best technique. Although, the repair is great for bilateral hernias and in obese patients, it might be easier to treat the morbidly obese patient with a different technique.
The Mesh Patch
The Bard Kugel patch (Davol, Cranston, Rhode Island) was developed to facilitate performance of the Kugel hernia repair. Although it is started out as a simple single-layer mesh, it became progressively more intricate in order to make the performance of the procedure easier and the repair more secure.
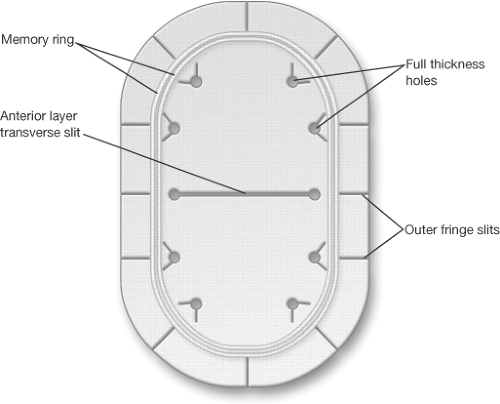
The patch is composed of two overlapping layers of knitted monofilament polypropylene mesh material that have been ultrasonically welded together (Fig. 8.1). A pocket of polypropylene is constructed on the outer edge of the patch which contains a single polyester fiber spring or stiffener that helps the patch to unfold after placement and maintain its configuration. One centimeter of mesh material extends beyond the outermost welds into which have been cut multiple radial slits. This outer fringe allows the patch to conform and fill more perfectly in the preperitoneal space, particularly when the patch folds back over the iliac vessels. A transverse slit is made in the center anterior patch, which is utilized for insertion of a finger which helps in positioning the patch in the preperitoneal space. Just beyond the anterior slit and inside of the mesh ring are multiple 3 mm holes through both layers of the patch. These serve to allow tissue to tissue contact through the patch to prevent movement of the patch after placement. This movement prevention is further augmented by several small V-shaped cuts associated with all of these holes in the anterior layer only. These cuts create a triangle of mesh which tends to pop up when the patch is placed and these act as sutureless anchors for the patch.
There are two mesh sizes used for groin hernias. The small patch is 8 × 12 cm and the medium patch is 11 × 14 cm. The small patch is adequate in most patients, although the larger patch does provide greater margin for error and is preferred in very large hernias. It is up to the surgeon to decide the appropriate size mesh patch used recognizing that the greater amount of underlay will probably result in fewer recurrences.
Operative Procedure
Anesthesia
General Anesthesia: This is my anesthetic of choice for this operation. The primary disadvantage of a general anesthesia is the limitation of the ability to test the repair at the completion of the operation.
Regional Anesthesia: This is the preferred choice for some patients with epidural anesthesia being preferred over spinal anesthesia. The epidural anesthetic has the advantage for re-dosing when the catheter is left in place during the procedure. This not only allows for minimal initial dose, but also for the administration of additional doses as needed, if the operation takes longer which may happen with bilateral hernias. Furthermore, epidural anesthesia results in less muscle paralysis enabling the patient to respond more forcefully when testing the repair following the operation.
Local Anesthesia: I have preformed this procedure using local anesthesia and monitored anesthesia care provided by an anesthesiologist, but maintenance of a relaxed patient is imperative to be able to enter and maintain appropriate visualization of the preperitoneal space through the incision. If the patient experiences pain and begins to bear down in response, it can make the procedure very difficult. Very obese patients with recurrent hernias or patients who do not tolerate monitored anesthesia care should not be done under local anesthesia because of the loss off visualization associated with muscle contraction and discomfort.
Patient Preparation
Appropriate laboratory and radiographic evaluation of patients preoperatively depends on the surgeon and the policies and procedures of the facilities in which they practice. Because of the risk of bleeding into the preperitoneal space, it is recommended that Coumadin be stopped 3 to 5 days prior to the surgery. Use of prophylactic antibiotics
is recommended due to the implantation of the foreign body into the wound. Although infection reduction is not clearly substantiated in controlled studies, antibiotics add little risk and may reduce graft infections.
is recommended due to the implantation of the foreign body into the wound. Although infection reduction is not clearly substantiated in controlled studies, antibiotics add little risk and may reduce graft infections.
Clipping of hair in the operative area is recommended over shaving at the time of the procedure, followed by an appropriate skin preparation.
The patient is positioned in a supine manner. During the performance of the operation exposure is improved by placing the patient in a Trendelenburg position with slight rotation away from the site of the procedure.
Regardless of the type of the hernia to be repaired, the mesh patch is placed in the same fashion into the preperitoneal space in every patient. The repair can be more difficult to learn because of a lack of familiarity with the anatomy in the posterior space and the angle in which the repair is approached. Understanding the unique approach is key to the successful performance of this procedure. Ideal first patients are of average size or thin where the anatomy should be clearly visible. Avoid recurrent hernias or large scrotal hernias initially. One of the advantages of this repair is the ease with which it can be converted to an anterior repair. The surgeon needs to back out of the preperitoneal space, allow the internal oblique muscle to re-approximate, and extend the skin and external oblique incision through the external ring and perform an anterior repair.
Incision
I think it is critical to utilize a headlight during the performance of this operation. Because of the angle in which the repair is approached, a headlight helps to illuminate extremely well the area of the preperitoneal space and allows for accurate placement and deployment of the mesh patch. In addition, use of a dedicated assistant is also extremely helpful. The operation can be performed with the surgical scrub functioning as the assistant. A dedicated assistant, particularly in larger patients, allows for continued visualization of the preperitoneal space through continuous retraction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree