Fig. 1
Longitudinal (left side) and transverse (right side) scanning of cervical esophagus (arrows). T Thyroid, C Carotid artery
Terminal esophagus is sub-diaphragmatic and can be examined by scanning sagittally the epigastrium or from the left paramedian site in ascending subcostal scans: the esophagus and the esophageal gastric junction are posterior to the left hepatic lobe, anterior to the osseous plan, and to the abdominal aorta (Fig. 2).
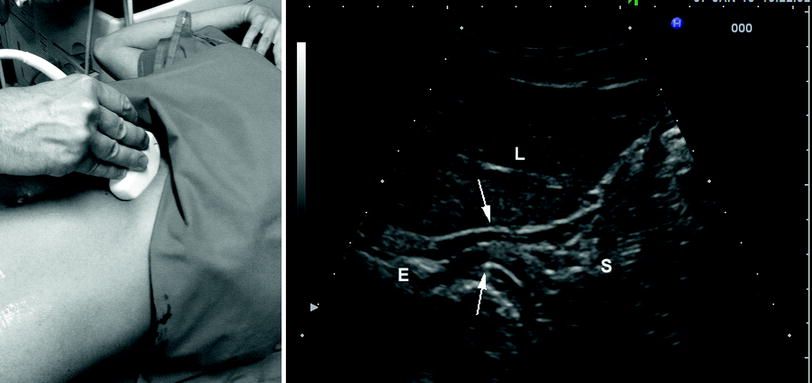
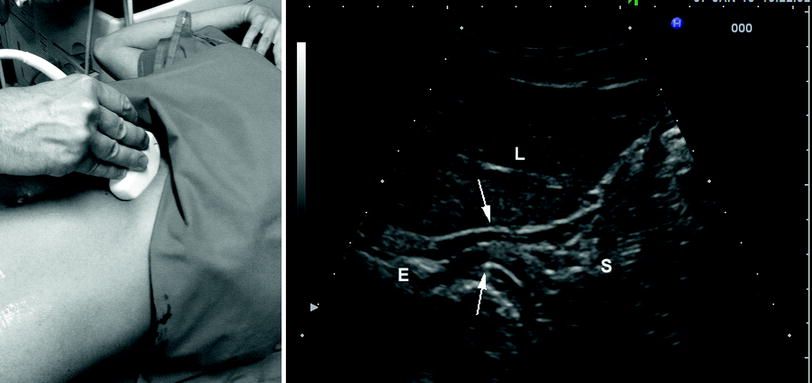
Fig. 2
Ascending subcostal scanning (left side) and corresponding ultrasonographic image (right side) of the terminal esophagus (E) and gastric cardia (arrows). L liver, S fundus of the stomach
3 Stomach
The stomach may be studied with 3.5–13 MHz convex or linear probes. The gastric wall is multilayered, and its thickness up to 7 mm, depending on its functional state (contraction or relaxation, stretching). To better visualize the gastric wall, the intake of a small quantity of water just before the examination can be convenient.
Fundus and gastric body can be difficult to look over because they are deep-seated and frequently filled with gas so that there is an obstacle to the passage of the ultrasound beam. Fundus and body can be imaged by scanning sagittally the epigastrium or using ascending subcostal scans from the left side, keeping the probe parallel to the axis of the costal arch. They are placed medially to the left hepatic lobe, before the tail of the pancreas and laterally to the spleen. Changing the patient position can be useful to better study the fundus and gastric body. Depending on the stretching of the organ and on its content, gastric folds can be seen as introflections of the gastric wall, scanning the organ transversally to its major axis (“carthweel” image), or as stratified structures parallel to the gastric wall using longitudinal scans (Fig. 3).
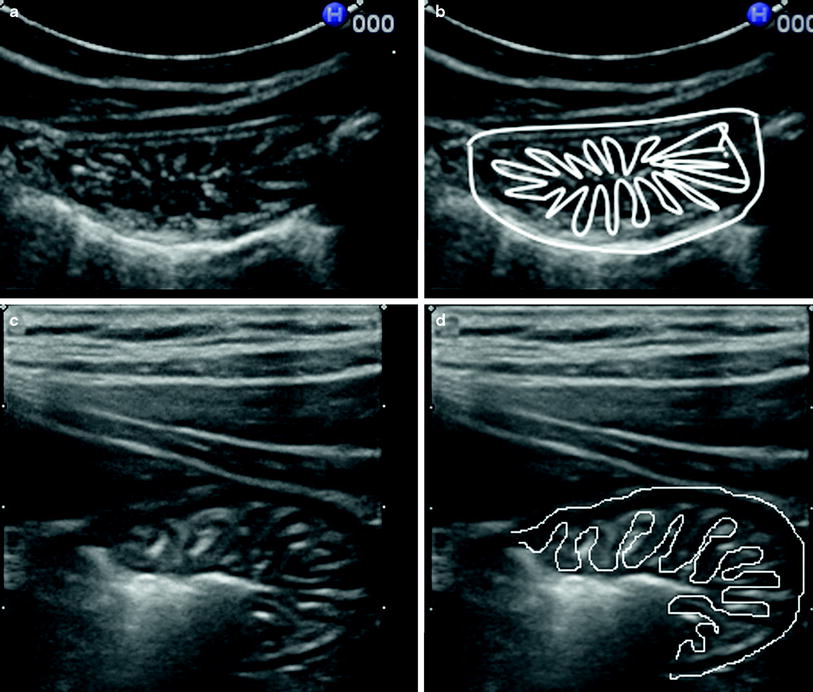
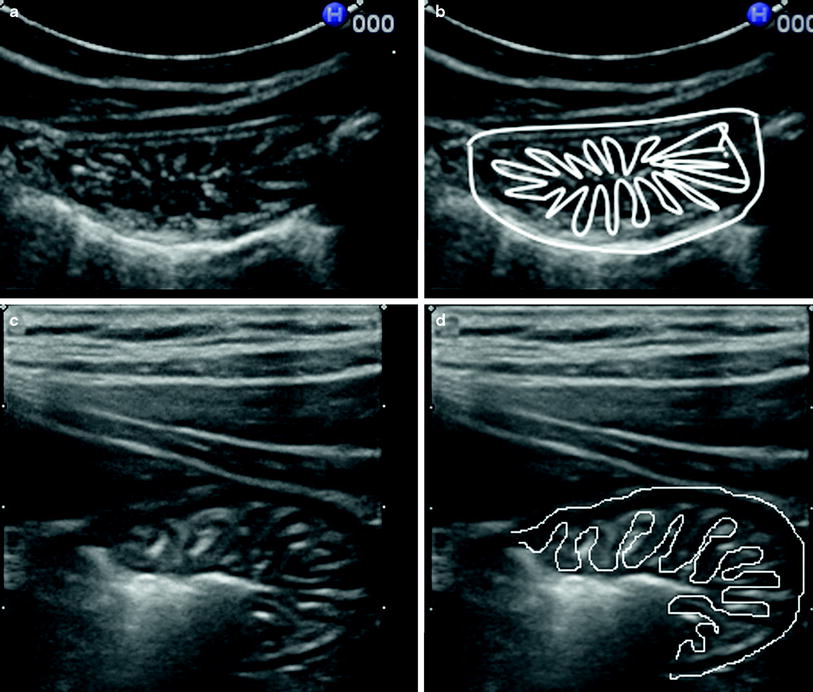
Fig. 3
Transversal scans (a, c) with schematic representations (b, d) of the gastric fundus showing gastric folds appearing as “carthweel” image
The antrum and the pyloric region can be more easily examined because they are superficial (some details can be studied with a linear probe as well). They can be detected with epigastric transversal and sagittal scans below the left hepatic lobe prior to the pancreatic body and the spleno-portal venous axis (Fig. 4). The pylorus can be distinguished from the antrum for its particular morphology and the greater thickness of its muscular layer (Fig. 5). Transabdominal ultrasonography may assess the anatomical variants of an operated stomach, which should be acknowledged because they can be mistaken for disorders of the small intestine or of the transverse colon. When a total gastrectomy has been performed a tubular structure, which is the terminal esophagus anastomosed to a jejunal loop, can be highlighted at the site of the stomach. In case of partial gastrectomy only the gastric stump anastomosed to jejunal loops is detectable.
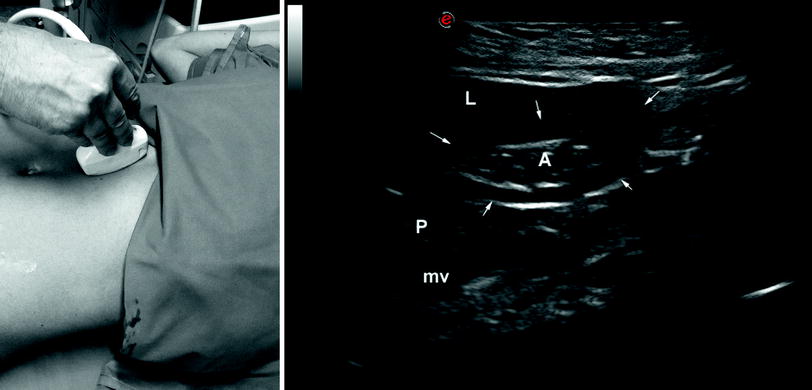
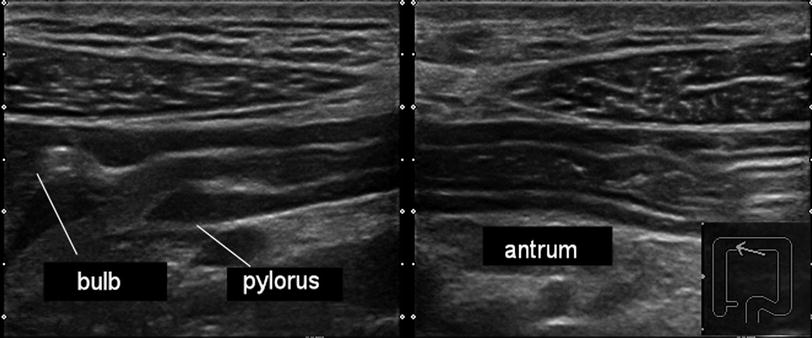
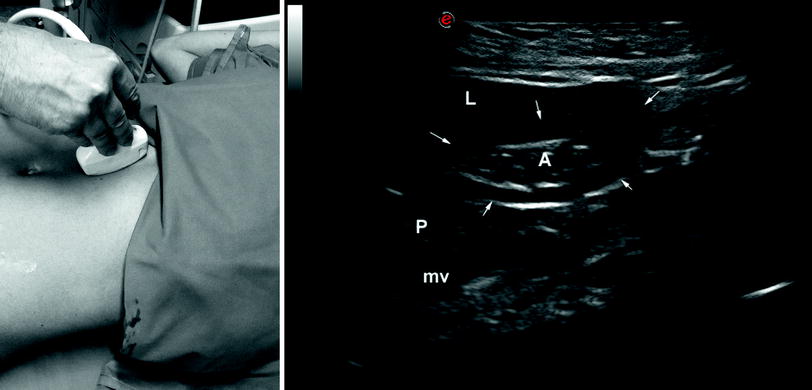
Fig. 4
Transversal scanning (left side) and corresponding ultrasonographic image (right side) of the gastric antrum (A) that is well demarcated by the thickened muscular layer (arrows). L liver, P pancreas, mv mesenteric vein
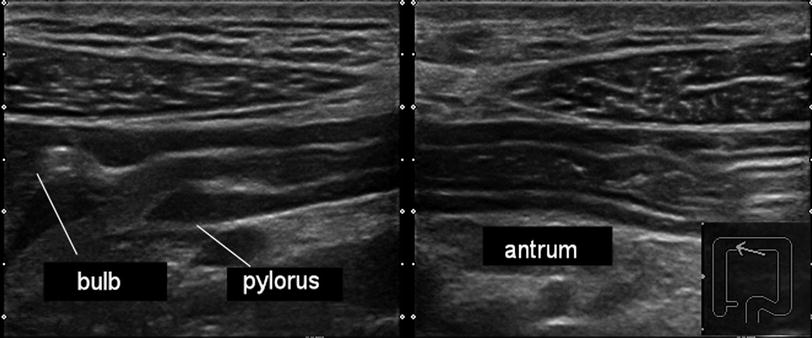
Fig. 5
Longitudinal scan on the long axis of stomach. On the left side it is well evident to the ogival shape of the thickened muscular layer of pylorus and the duodenal bulb. On the right side the antrum
4 Duodenum
The duodenum is divided into four parts each of them different for morphology, location, and relationship with the abdominal organs.
To the right of the pylorus, the duodenal bulb can be seen as a tubular structure with a thin wall and a mainly gaseous content, strongly echogenic under fasting conditions. It can be found below the left hepatic lobe, medial to the gallbladder, in front the cephalic portion of the pancreas and to the gastric antrum.
The second portion of the duodenum (descending duodenum) is antero-medial to the right kidney, lateral to the inferior vena cava and posterior to the gallbladder (Fig. 6). When the lumen is stretched by fluids, duodenal folds are recognizable as small fingerlike protrusions on the luminal site. Under the same conditions it is possible (rarely) to detect the papilla of Vater as a small (<1 cm) round structure protruding into the lumen.
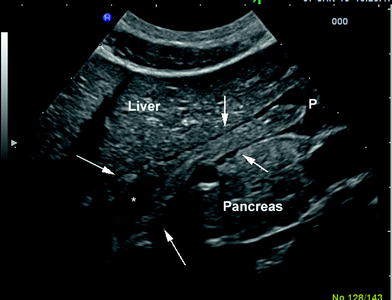
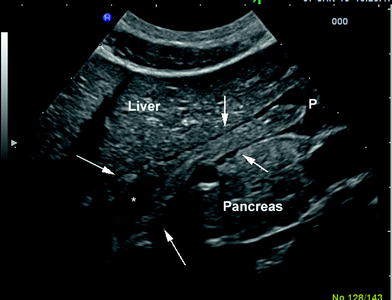
Fig. 6
Longitudinal scan of the bulb and descending duodenum (arrows) with liquid content (asterisk). P pylorus
The duodenal third portion has a very deep, horizontal course. It is difficult to visualize because of its seat and its lumen, normally collapsed. It can be searched with axial scans in the epi-mesogastrium before the aorto-caval plan, posteriorly to the superior mesenteric vessels.
The fourth duodenal portion (ascending) and the angle of Treitz are difficult to detect because they are located behind the stomach and frequently the gaseous content of the fundus and body is interposed. These structures can be detected with transverse scans of the epigastrium, behind the gastric antrum and before the pancreatic body and tail.
5 Small Intestine
Ultrasonography of the small intestine takes place in two stages. Usually it includes an overview scanning with the convex probe and a subsequent optimization of the details with linear or microconvex high frequency probes. The echogenicity of the wall is multilayered and the regular wall thickness, using high-resolution probes, with a slight degree of compression and in the absence of peristaltic contractions, is ≤4 mm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








