Chapter 34 FREE VAGINAL WALL SLING
Pubovaginal sling procedures are the main surgical operations used to correct stress urinary incontinence (SUI). These procedures provide for a tape insertion underneath the urethra or bladder neck. The American Urological Association guidelines panel studied the long-term efficacy of all anti-incontinence procedures and found that pubovaginal slings were among the most versatile and successful.1–14
Until the end of the 1990s in most cases autologous tissues were used to create a tape. However, by the late 1990s specialists began to make use of synthetic materials, mainly in the form of Prolene tapes.9,13
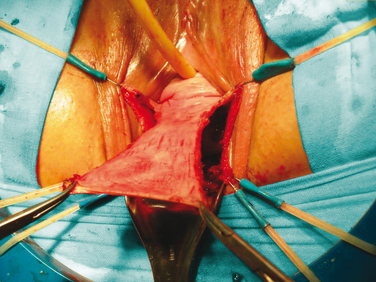
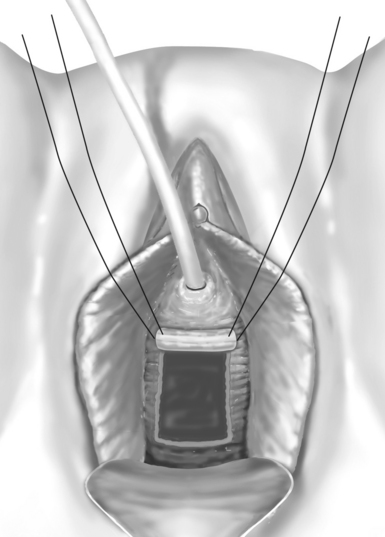
This chapter covers several aspects of the free vaginal wall sling procedure. At the same time, it touches on the technical particularities of the full-thickness, nonisolated vaginal wall flap, based on the bladder neck area. This procedure was first described in 1996 by the French group from Nice.11 The patient is placed in the lithotomy position with access to the suprapubic area, and an 18-Fr Foley catheter is inserted. After the vaginal cavity is exposed a ∪-shaped incision is made to create a rectangular flap based superiorly in the bladder neck (Fig. 34-1). During vaginal dissection, it is preferable to create a thin flap to preserve perivesical tissue for cystocele repair. After flap mobilization, the cystocele is repaired with a running double-layer 3-0 monofilament polyglyconate suture (Fig. 34-2). The rectangular vaginal flap is then rolled to form a tube and secured at each end with two 2-0 polypropylene sutures. Before being rolled, the vaginal flap must be de-epithelialized with a scalpel to prevent postoperative cyst formation. Then, the vaginal tube is positioned in the bladder neck and sutured to periurethral tissues or suspended subcutaneously with two 2-0 polypropylene sutures (Fig. 34-3). Cystoscopy is performed to rule out urethral or bladder perforation and confirm bladder neck suspension. Posterior colporrhaphy is performed, and a povidone-iodine–impregnated vaginal gauze is inserted; it is removed the following day. Normally, the Foley catheter is withdrawn after 48 hours.
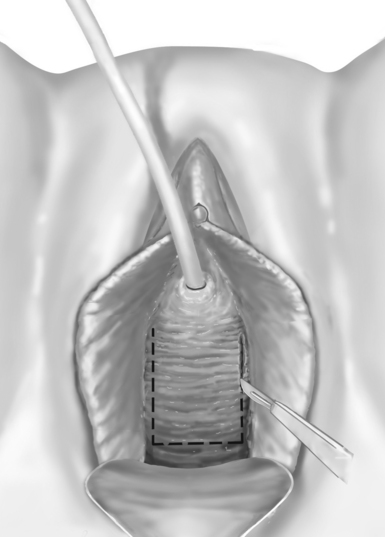
Figure 34-1 A U-shaped incision is performed to create a rectangular vaginal flap based on the bladder neck area.
Why do patients choose free vaginal wall sling procedures? What are the long-term functional results of these procedures? What is the purpose of the patient-doctor conversation, and should we convince our patients to proceed with this type of surgery? Should the free vaginal wall procedure remain in the surgical armamentarium? Finally, should we make any comparison with synthetic tapes or other tension-free vaginal tape (TVT)-like procedures?
RATIONALE
The free vaginal wall procedure may have the following applications:
PREOPERATIVE CONSIDERATIONS
Preoperative considerations currently include the following requirements: