Chapter 1 Four Decades
The History of ERCP
Endoscopic retrograde cholangiopancreatography (ERCP) has been a remarkable technological advance over the past 40 years in the field of gastrointestinal endoscopy and has redefined the medical and surgical approach to patients with pancreatic and biliary tract diseases. Since its inception in 1968, the medical community has witnessed significant achievements by the pioneers in endoscopy who incrementally advanced ERCP techniques from their infancy to maturity. The “infancy” of ERCP focused on diagnosis, the “adolescence” on therapy of common biliary tract diseases such as bile duct stones and malignant strictures, the “early adulthood” on pancreatic endotherapy and prevention of post-ERCP pancreatitis (PEP), and the current “mature adulthood” on continued refinement of techniques to make ERCP safer and more effective. Numerous pioneers in the field of ERCP have played significant roles in developing new techniques and novel instrumentation, spearheaded innovative techniques to reduce adverse events, and trained generations of endoscopists to perform safe ERCP. We have now reached a 40-year milestone in ERCP and can look back and recall an exciting and enjoyable journey, replete with enthusiastic innovation that has benefited so many patients (Boxes 1.1 and 1.2). It would require an entire textbook to incorporate all of the important contributions made by the many ERCP clinicians over the past 40 years. We extend an apology in advance to any individuals omitted from this brief summary of the history of ERCP.
Box 1.1 History of ERCP
Four Decades, Decade by Decade
1980s: Refinement and Reporting
 Refinement of accessories, improvements in radiographic imaging
Refinement of accessories, improvements in radiographic imaging
 Reporting adverse events of sphincterotomy
Reporting adverse events of sphincterotomy
 Biliary stent placement for obstructive jaundice and shift from palliative surgery
Biliary stent placement for obstructive jaundice and shift from palliative surgery
 Introduction of the teaching head: “seeing is believing”
Introduction of the teaching head: “seeing is believing”
 Acceptance of ERCP by the medical community
Acceptance of ERCP by the medical community
 ERCP training gets its start for physicians and ERCP nurses
ERCP training gets its start for physicians and ERCP nurses
1990s: Training and Expanding Therapy
 More emphasis on advanced training
More emphasis on advanced training
 Endoscopic photography and videography: sharing images with others
Endoscopic photography and videography: sharing images with others
 “Theater presentations” of ERCP
“Theater presentations” of ERCP
 Therapy of pancreatic disorders: chronic pancreatitis, pseudocysts, and necrosis
Therapy of pancreatic disorders: chronic pancreatitis, pseudocysts, and necrosis
 Era of laparoscopic cholecystectomy and bile duct injuries
Era of laparoscopic cholecystectomy and bile duct injuries
 Safer sphincterotomy: monofilament wires and computer-regulated blended current
Safer sphincterotomy: monofilament wires and computer-regulated blended current
 Complementary pancreaticobiliary techniques developed
Complementary pancreaticobiliary techniques developed
Box 1.2
Key Points
 In the early years of ERCP in the 1970s, pioneers such as McCune, Oi, Classen, Kawai, Cotton, Vennes, Silvis, Geenen, and others established a new technology.
In the early years of ERCP in the 1970s, pioneers such as McCune, Oi, Classen, Kawai, Cotton, Vennes, Silvis, Geenen, and others established a new technology.
 Close collaboration was vital between the endoscopist and industry to design new instrumentation leading to higher cannulation rates, improved sphincterotomy, more effective drainage techniques, and improved outcomes.
Close collaboration was vital between the endoscopist and industry to design new instrumentation leading to higher cannulation rates, improved sphincterotomy, more effective drainage techniques, and improved outcomes.
 The early adopters of ERCP were self-taught, and subsequent trainees were schooled by the apprentice model. Training accelerated with introduction of videoendoscopy. Minimum qualifications for ERCP competency were poorly defined.
The early adopters of ERCP were self-taught, and subsequent trainees were schooled by the apprentice model. Training accelerated with introduction of videoendoscopy. Minimum qualifications for ERCP competency were poorly defined.
 The fourth decade of ERCP has emphasized scientific rigor with several prospective, outcome-based studies. Newer techniques such as prophylactic pancreatic stent placement were adopted to make ERCP safer in high-risk patients for post-ERCP pancreatitis.
The fourth decade of ERCP has emphasized scientific rigor with several prospective, outcome-based studies. Newer techniques such as prophylactic pancreatic stent placement were adopted to make ERCP safer in high-risk patients for post-ERCP pancreatitis.
ERCP in Its Infancy
In the 1920s bile duct imaging was performed by surgeons Evarts Graham and Warren Cole with the use of intravenously administered iodinated phenolphthalein that was selectively excreted into the bile and recorded radiographically. Oral cholecystography and percutaneous skinny “Chiba” needle cholangiography were subsequently developed to improve the visualization of the bile duct.1,2 What defied the clinician was a nonoperative technique to image the pancreatic duct. In 1965 two innovative radiologists, Rabinov and Simon,3 fashioned a bendable catheter that was inserted through a peroral basket catheter. The medial duodenal wall was “blindly scratched” with the tip of the catheter and resulted in the first nonoperative pancreatogram (Fig. 1.1). In eight attempts, Ravinov and Simon obtained an interpretable pancreatogram in two patients. The gastrointestinal endoscopist now entered the arena. William McCune and his surgical colleagues at George Washington University (Washington, D.C.) are credited with the first report of endoscopic cannulation of the ampulla of Vater in living patients.4 McCune used an Eder fiberoptic duodenoscope (Eder Instrument Company, Chicago), which had both a forward and side lens and an endotracheal-type cuff placed on the scope just beyond the lens. The balloon was inflated and deflated to enable adequate focal length for mucosal visualization. McCune taped a small-diameter plastic tube that served as a tract to the endoscope and could house a bendable cannula. The cannula was advanced to the major duodenal papilla under endoscopic guidance. McCune’s cannulation success rate was only 25% (50% duodenal intubation and 50% pancreatic duct opacification) in his report of 50 patients. In his discussion of the first reported series, McCune stated: “Anyone who looks through one of these instruments has to have 2 personality characteristics. First, he has to be honest, and secondly, you have to have an undying, blind, day and night, uncompromising persistence.” ERCP was born, and slowly grew to an established technique due to the honesty and persistence of endoscopic pioneers.
In March 1969 in Japan, Oi (Fig. 1.2) and colleagues—in close collaboration with Machida (Machida Endoscope, Ltd., Tokyo) and Olympus corporations (Olympus Optical Co., Ltd., Tokyo)—developed a side-viewing fiberoptic duodenoscope with a channel and an elevator lever to enable manipulation of the cannula. Initially, Oi was able to visualize the ampulla in about half of 105 cases.5 In a subsequent report, Oi was able to cannulate the papilla in 41 of 53 patients (71%) without significant morbidity.6 By 1972 Jack Vennes and Steven Silvis of the University of Minnesota had published the experience in their first 80 attempts at cannulation of the bile and pancreatic ducts, paving the way for acceptability in the American endoscopic wilderness (Table 1.1).7,8 Over the next 5 years, pioneers with the names Safrany, Cotton, Geenen, Siegel, Classen, and Demling and the Japanese groups (Fig. 1.3) embraced this new technique and reported on the successes (cannulation rates >90%) (Fig. 1.4), the shortcomings (PEP), the nuances (variety of cannula types, cannulation angles), and the practical application of ERCP in our understanding of biliary and pancreatic disorders.9–15 But what could we as endoscopists do with this newfound knowledge?
Fig. 1.2 One year after Dr. William McCune successfully performed the first ERCP at George Washington University, in Japan Dr. Itaru Oi, with his chief Dr. Takemoto, performed endoscopic cholangiopancreatogram (ECPG), as it was called, with a Machida scope in 1969.5 The method used was almost the same as Dr. McCune using a prolonged gastrofiberscope. In close collaboration with the Machida and Olympus corporations, Oi developed a side-viewing fiberoptic duodenoscope with a channel and an elevator lever to enable manipulation of the cannula.
Table 1.1 ERCP in Its Infancy: Cannulation Rates around 1972
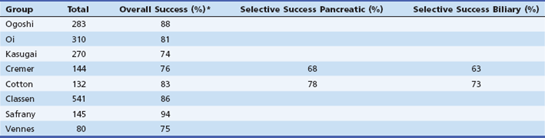
*Generally defined as entry into either duct.
From Cotton PB. Progress report: cannulation of the papilla of Vater by endoscopy and retrograde pancreatography (ERCP). Gut 1972;13:1014-1025.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree