Fig. 1
Parks’ classification of perianal fistulae
The treatment of perianal fistulae may be medical or surgical. It depends mainly on the nature and course of fistulae and the presence of abscesses. Cryptoglandular fistulae usually are primarily treated by surgery, whilst patients with Crohn’s disease are treated with antibiotics, immunosuppressive agents or anti-tumour necrosis factor alpha, but after have ruled out the presence of abscesses.
Therefore, accurate diagnosis of these lesions is mandatory for the proper management, since incorrect or inappropriate treatment may lead to irreversible functional consequences and recurrence of the fistula.
To date, the main imaging modalities in the management of patients with perianal fistulae are transanal ultrasound and magnetic resonance imaging (MRI). Transperineal ultrasound has been proposed when these diagnostic tools are contraindicated, not appropriate or not available, and as a non-invasive and cheap technique to monitor perianal lesions during treatment.
2 Transperineal Ultrasound
Transperineal ultrasound is a simple, non invasive and cheap technique, to study the pelvis and perianal inflammatory diseases. It is an alternative to MRI or transanal ultrasound when, for various reasons, these are contraindicated or not appropriate, in particular in children and patients with anal strictures, painful perianal abscesses or lesions extending far from the anus and not accessible to transrectal ultrasound (e.g. in gluteus or in the scrotum). For these reasons, being perianal ultrasound performed with conventional probes, may be also used as readily available adjunct imaging procedure in patients with incomplete or dubious findings in previous examinations.
2.1 Sonographic Features
Perineal fistulae can be detected by transperineal ultrasound as hypoechoic tracts, sometimes with air within, between the anus or rectum and the perianal skin or vagina (Stewart et al. 2001; Mallouhi et al. 2004; Wedemeyer et al. 2004; Zbar et al. 2006; Domkundwar and Shinagare 2007). Transperineal ultrasound also can indentify the site internal opening of the fistulae and enable a description of their anatomical course, providing a correct classification according to the Parks criteria. Internal opening may be revealed as a hypoechoic focus in the intersphincteric space that abuts the internal sphincter, often with a small corresponding defect in the internal sphincter. The site of internal opening may be assessed with a sensitivity ranging from 90 to 95 %. (Fig. 2; Wedemeyer et al. 2004; Zbar et al. 2006; Domkundwar and Shinagare 2007).


Fig. 2
Transperineal internal opening assessment. Internal opening (arrows) clearly appears at 6 o’clock as hypoechoic focus in the intersphincteric space that abuts the internal sphincter and crosses the submucosal layer of anal canal. V: vagina
Regarding the classification of perianal fistulae, intersphincteric fistulae are visualised as hypoechoic tract within or closer to internal sphincter (Fig. 3).
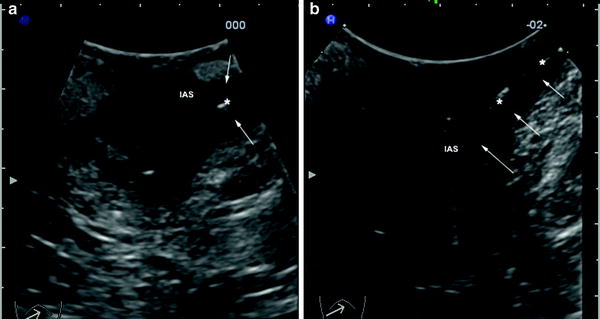
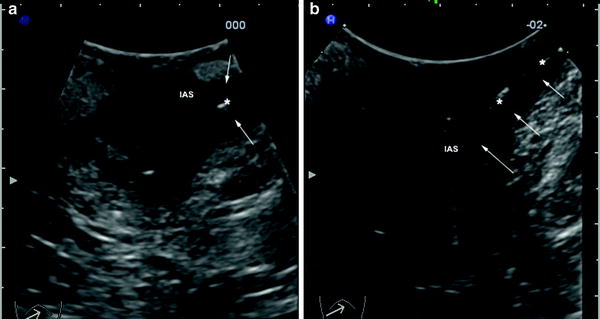
Fig. 3
Intersphincteric fistula (arrows) in a young woman detected by a cross sectional (a) and by longitudinal (b) transperineal scans. The fistula is visualised as hypoechoic area (a) or tract (b) containing gaseous hyperhecoic spots (asterisks), within or closer to internal anal sphincter (IAS)
Transsphincteric fistulae appear as hypoechoic tracts that cross the external sphincter (Fig. 4). Extensions of these fistulae may be revealed as hypoechoic fluid collections and intersphincteric horseshoe extension that may be imaged by transverse scan (anterior translabial scans in women) or as ovoid lesions just posterior to the anorectal junction (Fig. 5). Ischioanal or supralevator extensions and abscesses may be imaged as collection or hypoechoic extensions or masses beyond the external sphincter and elevator anii (Fig. 6). Rectovaginal or anovulvar fistulae can be imaged as hypoechoic areas or tracks between rectum or anus and vagina or vulva (Fig. 7).
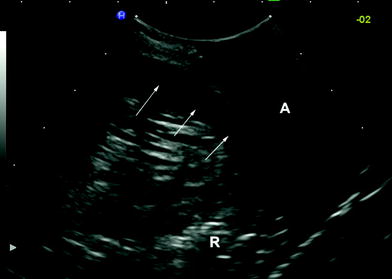
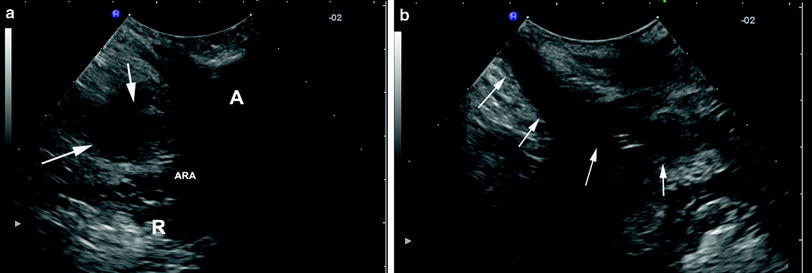

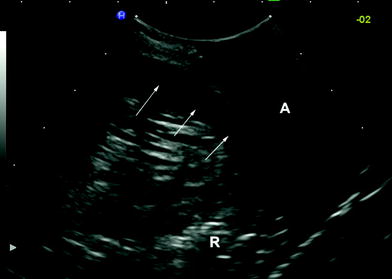
Fig. 4
Trans-sphincteric fistula detected by a longitudinal transperineal scan. The fistula, visualised as hypoechoic tract (arrows), arises for the posterior side of the anorectal junction and crosses the external anal sphincter. R, rectum; A, anus
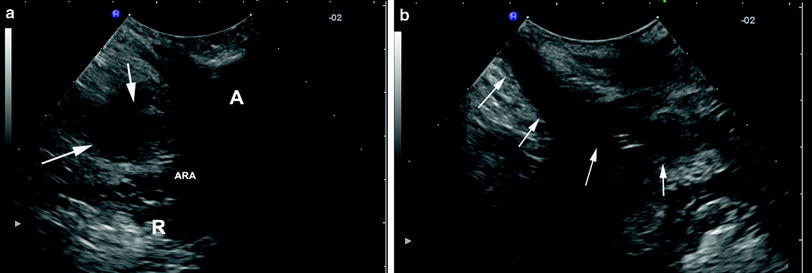
Fig. 5
Longitudinal (a) and transversal (b) perianal sonographic cross-sections of a transsphincteric fistula with left horseshoe extension (arrows). A, anus; R, rectum, ARA, anorectal angle

Fig. 6




Ischioanal abscesses (a, b) detected by transperineal scans as hypoechoic or anechoic areas sometimes with inhomogeneous or gaseous content (A) extending beyond the external sphincter. c, Complex perianal Crohn’s disease with a large perianal abscess (asterisks) extending beyond the elevator anii (arrows)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








