Pantelis A. Sarafidis, George L. Bakris
Evaluation and Treatment of Hypertensive Urgencies and Emergencies
The term malignant hypertension first appeared in 1928 and described patients with extremely high blood pressure (BP) values, to emphasize that because of rapid target organ damage, their average prognosis was similar to that of most cancer patients.1 Subsequently, malignant (or accelerated) hypertension was used to describe patients with greatly elevated BP and vascular damage that could manifest as retinal hemorrhage/exudate and papilledema, usually associated with encephalopathy, acute kidney injury, and microangiopathic hemolytic anemia.2,3 However, dramatic advances in both in-hospital and outpatient treatment of hypertensive emergencies have led to an improved prognosis, that is, a decrease in 1-year mortality from 80% in 1928 to 50% in 1955 and to less than 10% after 1990.4,5 Thus, terms such as malignant and accelerated hypertension have been replaced by hypertensive emergency and hypertensive urgency.
Marked elevations in systolic and diastolic BP, usually above 180/120 mm Hg, can be classified as either emergencies or urgencies. A hypertensive emergency is defined as a marked elevation in BP complicated by evidence of acute target organ damage, such as coronary ischemia, dissecting aortic aneurysm, pulmonary edema, hypertensive encephalopathy, cerebral hemorrhage, and eclampsia. In hypertensive emergency, BP should be reduced by at least 20 to 40 mm Hg within 10 to 30 minutes using parenteral drug therapy in an intensive care unit (ICU) to limit end-organ damage. Hypertensive urgency is a clinical setting of significant BP elevation without acute target organ dysfunction. The approach to hypertensive urgency is a gradual BP reduction within hours, usually with oral medications.4,6–8
Etiology and Pathogenesis
Hypertensive emergencies and urgencies can develop de novo in normotensive individuals or can complicate underlying primary or secondary hypertension.4,8 Box 37-1 shows the most common etiologies of hypertensive crises. In some hypertensive emergencies, an underlying condition is the clear cause of acute BP elevation. In acute glomerulonephritis, renal crisis (in patients with scleroderma), or renal artery stenosis, severe BP elevations are evoked through increased activity of the renin-angiotensin system (RAS). In pheochromocytoma, cocaine intoxication, or spinal cord injury, acutely elevated BP is the result of excess catecholamine release. In other patients, acute sustained elevations in BP itself are the etiologic factor resulting in conditions such as hypertensive encephalopathy or acute left ventricular failure and pulmonary edema. In some cases, however, it may be difficult to differentiate whether BP elevation is the cause or the result of a hypertensive emergency. Thus, a careful diagnostic evaluation of hypertensive emergencies and urgencies is essential to guide proper treatment.
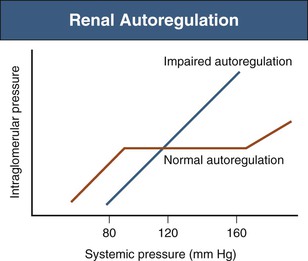
A hypertensive emergency can occur in various clinical settings, but the most common is chronic, often untreated or poorly controlled hypertension in a patient whose usual BP is above 180/120 mm Hg. In many of these patients, chronically elevated BP does not affect target organ perfusion because of autoregulation. Autoregulation is the ability of blood vessels to dilate or to constrict in response to changes in perfusion pressure and thereby maintain normal organ perfusion. This mechanism is present in the brain and kidneys and involves l-type calcium channels.9 Arteries from normotensive individuals can maintain flow over a wide range of mean arterial pressures, 80 to 150 mm Hg, associated with systolic BP of around 90 to 180 mm Hg. Chronic BP elevations cause compensatory functional and structural changes in the arteriolar circulation and shift the autoregulatory curve to the right, which allows hypertensive patients to maintain normal perfusion and avoid excessive blood flow at higher BP levels.3,10 Over time, the structural and functional changes in cerebral and renal arterioles may lead to a progressive inability of the arterioles to autoregulate properly8,9 (Fig. 37-1).
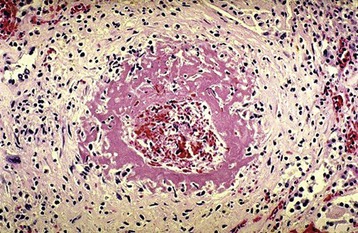
Target organ damage associated with hypertensive emergency results from the inability of autoregulatory mechanisms to maintain normal perfusion pressures in certain vascular beds (especially of brain and kidney) when BP rises above the autoregulatory range.10 The resultant endothelial injury causes a loss of endothelial antithrombotic properties, with activation of platelets and the coagulation cascade, increased vascular wall permeability, and vascular smooth muscle cell proliferation culminating in an increase of tissue ischemia and ultimately fibrinoid necrosis. This is coupled with activation of hormonal systems and release of vasoactive substances (RAS, catecholamines, endothelin, vasopressin) that maintain a vicious cycle of elevated BP and vascular injury.3,8
The typical structural changes associated with hypertensive emergencies are fibrinoid necrosis of small arteries and arterioles in the brain and kidney (Fig. 37-2). Other findings may show injury of the affected organs (e.g., cerebral edema).3,10 Hypertensive emergency may rarely present as a thrombotic microangiopathy, in particular if associated with scleroderma (see Chapter 29).
In normotensive or minimally hypertensive individuals, such as children or pregnant women, the symptoms and signs of a hypertensive emergency occur at lower BP levels than in hypertensive patients because adaptive chronic vascular changes are absent. In most patients, however, the development of a hypertensive emergency occurs in the presence of chronic hypertension. This may relate to other mechanisms contributing to impaired autoregulation, such as progressive arteriolar disease (both cerebral and renal circulation) and pharmacologically impaired autoregulation (e.g., use of dihydropyridine calcium channel blockers, or furosemide).
Epidemiology
The exact incidence of hypertensive emergencies and urgencies or the demographic distribution is not known, but an estimated 1% to 2% of individuals with hypertension develop hypertensive crises.11 One study with more than 14,000 emergency department (ED) visits showed that hypertensive urgencies accounted for 76% and emergencies for 24% of hypertension-related visits.12 In this study, the most common presentations of hypertensive emergency were associated with cerebral infarction (24.5%), acute pulmonary edema (22%), hypertensive encephalopathy (16%), and acute heart failure (14%), followed by myocardial infarction (12%), cerebral hemorrhage (5%), eclampsia (5%), and aortic dissection (2%). In a different series of 435 hypertensive ED visits, 40% were hypertensive urgencies, almost all with some degree of preexisting kidney disease, and 60% were emergencies.13 Hospitalization for hypertensive emergency occurs at a rate of 1 to 2 cases per 1 million population per year in the United States.10
In developed countries, widespread use of antihypertensive agents has reduced the incidence of hypertensive emergencies, as supported by indirect observations.10 Use of any antihypertensive drug reduces the risk of hypertensive emergency because poor treatment compliance and outpatient BP control are predictors of subsequent hypertensive crises.14 Further, hospitalization for hypertensive emergency is more common in developing countries, ethnic minorities of developed countries,5 and individuals of low socioeconomic status who often have poor BP control.
Diagnostic Evaluation
The primary goal of the diagnostic process is differentiation of a true hypertensive emergency from a hypertensive urgency, because of the different therapeutic approaches. The second goal is rapid assessment of the type and severity of ongoing target organ damage. In some hypertensive emergencies, the history (e.g., acute head trauma, preeclampsia, scleroderma) or overt symptoms and signs (e.g., chest/back pain, dyspnea, throbbing abdominal mass) may guide the diagnosis; whereas in other cases (e.g., severe hypertension with altered mental status), the evaluation is more comprehensive.
The diagnostic approach begins with the patient’s history, with attention to duration, severity, and treatment of preexisting hypertension and associated conditions6,8 (Box 37-2). BP measurements should be performed in both arms (if possible, in both sitting and standing positions) and a leg2 (see Chapter 33). A careful examination and assessment of cardiac, pulmonary, peripheral vascular, and neurologic systems with assessment of mental status should follow, along with a thorough funduscopic (ophthalmoscopic) examination for hemorrhages, exudates, and papilledema.
Signs of secondary hypertension should not be missed in this initial examination. For example, an abdominal bruit may indicate renovascular hypertension; a palpable abdominal mass suggests abdominal aneurysm or polycystic kidneys; a radial-femoral pulse delay suggests aortic coarctation; abdominal striae and central obesity are observed with Cushing syndrome; and exophthalmos may indicate hyperthyroidism. Patients with features of hemolytic anemia and thrombocytopenia should be evaluated for causes of thrombotic microangiopathy.
The initial laboratory studies in a hypertensive emergency include a complete blood count with peripheral smear, urinalysis, creatinine and urea concentration, and electrolyte values.6,8 Comparison of kidney function with a patient’s recent measurement is important. Severe hypertension accompanied by acute deterioration in kidney function, microscopic hematuria with red blood cell casts, or nephritic urine sediment suggests acute glomerulonephritis. If a secondary form of hypertension is suspected, samples for plasma renin activity, aldosterone concentration, and plasma free catecholamines and metanephrines should also be drawn before
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree