Establishment of a Hysteroscopy Program
Michael S. Baggish
Prior to establishing any program, a gynecologist, or a nuclear group of gynecologists, must be suitably trained in diagnostic and operative hysteroscopy. This should include preceptorship training. Thoughtful front-end planning is recommended before initiating a hysteroscopy program. Organization beforehand will minimize frequently costly and always aggravating mistakes. The endeavor should be reduced to component parts, which are best transmitted by the written word. Diagrams, photographs, and equipment brochures should be kept in a file entitled, for example, “Hysteroscopy Project.” An accurate budget should be constructed based on available funds and should be matched line for line with quoted costs. Again, word of mouth is a poor substitute for written documentation.
Although simulator devices may be useful to improve hand–eye coordination, the actual performance of several diagnostic and operative hysteroscopies is essential to develop the necessary skills to perform the operation well. Simple problems that can make or break a successful operation include (a) navigating the cervical canal and internal cervical os, (b) distending the uterine cavity, and (c) obtaining a clear view of the uterine contents. Unfortunately, simulation techniques do not incorporate the above three functions into their programs. The most critical problem that the surgeon must overcome is a suboptimal visual field. Without seeing the uterine cavity clearly, one cannot rule out disease nor can one perform surgery.
Location for Performance of Hysteroscopy
Several sites may be used for this procedure. In the previous chapters, mention has been made of the office, surgicenter, and operating room as the most likely locations for the performance of hysteroscopy. One might also consider that examinations could conceivably be done in the clinic, emergency room, labor and delivery unit, or inpatient treatment room. Fixed or at least stable locations for the more fragile and heavier equipment should be established in areas where the largest numbers of cases are anticipated. Portable equipment setups should be prepared for use in less likely sites.
For office endoscopy, select the most spacious examining room available and make certain it is adequately wired with three-prong electrical outlet receptacles. An electrically controlled examining table is a necessity because raising
and lowering the patient is an anticipated routine during hysteroscopy (Fig. 33.1). A high-intensity, multipositional examining light, preferably wall mounted, is paramount if one anticipates doing contact hysteroscopy. Space should be allocated for a double- or triple-tiered mobile table where prep solutions, swabs, and accessory instruments are placed in addition to the light generator, CO2 insufflator, hand-held Hyskon Pump (Cook Ob-Gyn), or low-viscosity infusion fluid. Adequate counter, cupboard, and shelf space will pay dividends, as will a sink with running water.
and lowering the patient is an anticipated routine during hysteroscopy (Fig. 33.1). A high-intensity, multipositional examining light, preferably wall mounted, is paramount if one anticipates doing contact hysteroscopy. Space should be allocated for a double- or triple-tiered mobile table where prep solutions, swabs, and accessory instruments are placed in addition to the light generator, CO2 insufflator, hand-held Hyskon Pump (Cook Ob-Gyn), or low-viscosity infusion fluid. Adequate counter, cupboard, and shelf space will pay dividends, as will a sink with running water.
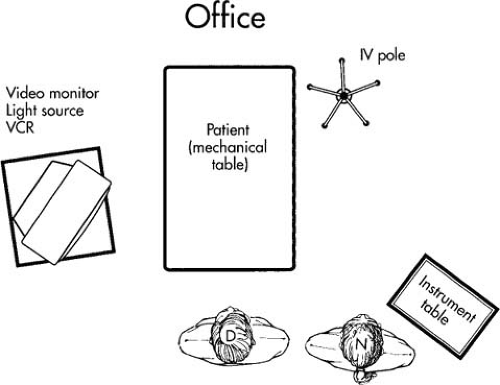 FIGURE 33.1 Placement of personnel and equipment for office hysteroscopy. VCR, videocassette recorder; IV, intravenous, D, doctor; N, nurse. |
Surgicenter and operating suite locations already have the requisite accoutrements necessary for the performance of diagnostic and operative hysteroscopy. However, dedicated storage space for the concentration of equipment must not be taken for granted. A special shelf, cabinet, or cart should be procured to keep all the hysteroscopy equipment in one place; otherwise things tend to get lost or damaged. Even with the best intentions, new and less experienced nursing assistants will from time to time be called on to help with hysteroscopy procedures. If the location of everything that is needed to do the operation is known, the sequence of events will progress smoothly rather than helter-skelter (Fig. 33.2). Again a shelved, mobile cart is a handy place in which to locate light sources, insufflators, endoscopes, accessories, and supporting packs. When hysteroscopy is ready to begin, the cart is simply wheeled up to the operating table, the fiberoptic cable and connecting tubes are plugged in, and the surgeon is ready to go (Fig. 33.3).
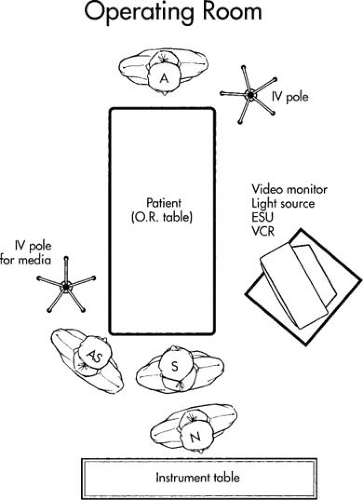 FIGURE 33.2 Placement of personnel and equipment for operative hysteroscopy. A, assistant; IV, intravenous; O.R., operating room; ESU, electrosurgery unit; VCR, videocassette recorder; AS, assisting surgeon; S, surgeon; N, nurse.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





