, Puja Gaur2 and Shanda H. Blackmon1
(1)
Division of General Thoracic Surgery, Mayo Clinic, 200 First Street SW, Rochester, MN 55905, USA
(2)
Division of Thoracic Surgery, Department of Surgery, Houston Methodist Hospital, 6565 Fannin Street, Houston, TX 77030, USA
Keywords
Esophageal reconstructionGastric conduitColon conduitJejunal conduitSpecial thanks to K.R. Shen for intraoperative images donated to this chapter.
There are several ways to create a neo-esophagus when resection of the esophagus is required. Table 10.1 lists options for conduits.
Table 10.1
Esophageal Tube Conduits
Conduit | Blood supply | Selection/placement |
|---|---|---|
Stomach | Gastroepiploic | First choice for total esophageal replacement |
Colon | Marginal artery of Drummond | Second choice for total esophageal replacement |
Free jejunum | Mesenteric anastomosis to LIMA/LIMV or cervical vessels | Isolated short-segment cervical esophageal reconstruction |
Pedicled jejunum | SMA | Optimal for Merendino resection (vagus-sparing resection) or short segmental resection |
Long-segment supercharged pedicled jejunum | Superior: Mesenteric anastomosis to LIMA/LIMV or cervical vessels Inferior: SMA | Second choice for total esophageal replacement |
Skin/forearm | Radial artery anastomosis to LIMA/LIMV or cervical vessels | Optimal for segmental neck resection, small area patch |
Myocutaneous flap | Flap artery anastomosis to LIMA, LIMV, cervical vessels, or AV loop | Last choice when no other options remain or when a small patch to augment a stricture or narrowing is needed |
Gastric Conduit
The stomach is always the first choice of esophageal reconstruction, when available (Fig. 10.1). The procedure involves four key steps:
Mobilization of the stomach
Division of the left gastric artery and short gastric vessels
Preservation of the gastroepiploic artery
Preparation for passage to the chest or neck for anastomosis
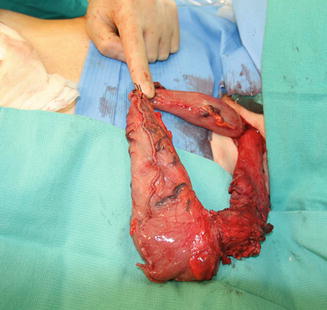
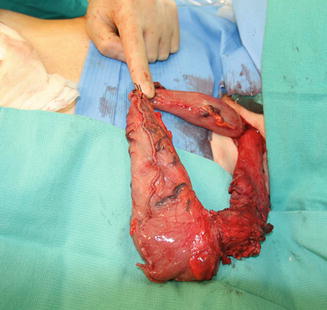
Fig. 10.1
Esophageal reconstruction using a gastric conduit. During a transhiatal esophagectomy the gastric conduit that will become the neo-esophagus is delivered into the neck. The esophagus is divided at least 5 cm proximal to the tumor to obtain a good margin. The cephalad portion of the conduit will also be excised and the specimen sent to pathology
Approaches for reconstruction of the esophagus using a gastric conduit include the Ivor Lewis esophagectomy, McKeown esophagectomy, transhiatal esophagectomy, or the minimally invasive approach. The details of these operations are described in Chap. 7.
Colon Conduit
We prefer to perform a supercharged colon conduit instead of a colon conduit alone, to avoid poor venous drainage, but, as an alternative, the colon can be used without supercharging. The procedure involves six key steps:
Identification of the segment of colon to be used
Mobilization of the colon
Division of vessels
Preservation of the marginal artery
Preparation for passage to the chest or neck for anastomosis
Creation of the anastomosis
Position
Supine position
For cervical anastomosis, the neck is extended and rotated to the right
For intrathoracic anastomosis, a subsequent left lateral position is used for right thoracotomy
The legs are prepared and draped in case vein from the leg is required for harvesting
Incisions
A midline laparotomy is typically used for colon preparation.
Operation
1.
Dissection of the colon:
(a)
Midline abdominal incision
(b)
Lysis of adhesions if present
(c)
Identification of the segment of colon for use as the conduit
(d)
Transillumination and mobilization of the bowel mesentery
(e)
Identification of the blood supply to the colon
(f)
A Wood’s lamp can be used to assess for adequate blood supply of the colon prior to transposition.
2.
Selection and division of colon blood supply branches:
(a)
Choose the arcade based on transilluminated visualization and length.
(b)
The ideal colonic arterial choice is depicted in Fig. 10.2 (a, left colon; b, transverse colon; c, right colon). There will be anatomic variations and shortened mesenteries from scar tissue.
Fig. 10.2
(a) Left colon resection to provide a conduit for esophageal reconstruction. (b) Transverse colon resection to provide a conduit for esophageal reconstruction. (c) Right colon resection to provide a conduit for esophageal reconstruction
(c)
For a supercharged colonic conduit, the vessel will eventually be connected by a microvascular anastomosis to the left internal mammary artery (LIMA) and left internal mammary vein (LIMV) or jugular vein (Fig. 10.3).
Fig. 10.3
(a) Preparing the colonic conduit. (b) The colon has been delivered to the neck in preparation for the microvascular anastomoses and subsequent esophagocolonic anastomosis
(d)
Open the mesentery to optimize length of available colonic graft (Fig. 10.4).
Fig. 10.4
(a) The colonic mesentery has been “unfurled” to allow the colon to reach the neck. (b) Schematic of the unfurled colonic mesentery
(e)
Do not divide this segment until the tunnel has been created and the donor vessels have been prepared, because once the blood supply has been divided, the clock starts for ischemia time.
3.
Preparing the neck; Dissection of the neck and blood supply:
(a)
Perform an incision anterior to the sternocleidomastoid muscle low on the neck, extending onto the chest either midline or to the left of midline (Fig. 10.5a).
Fig. 10.5
Neck incision to prepare the neck for the conduit. (a) Left oblique neck incision carried onto the chest para-median and to the left side of the patient to expose the internal mammary artery and vein and (b) resect the head of the clavicle, the head of the first rib, and perform a hemi-manubriectomy
(b)
Detach the sternocleidomastoid at the head of the clavicle.
(c)
Dissect around the left first rib about 3 cm lateral to the sternal border.
(d)
Divide the clavicle just lateral to the head and medial to the ligamentous attachments of the clavicle to the first rib. Divide the first rib 3 cm lateral to the sternal border; when supercharging the colon, allow enough space to dissect the LIMA for microvascular augmentation of the pedicled colonic flap.
(e)
A hemimanubrectomy is performed, angled to the left on top of the second rib. The manubrium, the head of the clavicle, and the proximal first rib are removed en bloc. Beware of the internal mammary artery, which will be located beneath the cartilaginous portion of the ribs, about 1 cm from the sternal border (Fig. 10.5b).
(f)
A rongeur is used to resect additional bone if needed; smooth the edges so that nothing sharp will injure the bowel or mesentery.
(g)
Prepare the recipient vessels for microvascular anastomosis. The LIMA is typically an adequate artery, but the LIMV may or may not be robust enough for use. If not, consider using the jugular vein. A saphenous vein graft can be used to lengthen the artery or vein, depending on the position of the conduit and recipient vessels.
4.
Creation of the tunnel for the conduit:
(a)
Create a substernal tunnel, if possible.
From the abdomen, make an incision on the anterior midline aspect of the diaphragm.
Create a substernal tunnel while attempting to stay extrapleural. (An intrapleural route may be necessary in some cases.) Allow enough space for the conduit and mesentery to pass unobstructed. (About 5 cm should be adequate.)
(b)
A posterior mediastinal route is an alternative.
(c)
If neither a retrosternal route nor a posterior mediastinal route is available, a subcutaneous route may be taken as a last resort.
5.
Delivery of the colon through the substernal tunnel:
(a)
Prepare a large camera bag or ultrasound probe cover.
(b)
Ensure that the tunnel is large enough to allow for the colon and mesentery, as well as postoperative edema.
(c)
Deliver the bag through the tunnel from bottom to top (Fig. 10.6).
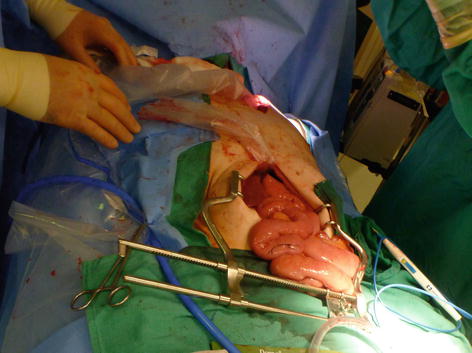
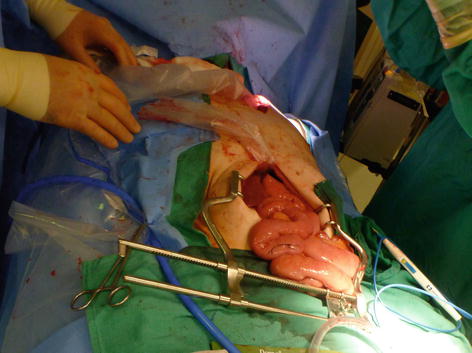
Fig. 10.6
A laparoscopic camera bag or ultrasound probe cover is passed through the tunnel created for the conduit
(d)
Trace the bowel back to the mesentery and place the untwisted segment of colon into the bag (Fig. 10.7); moisten the inside and outside of the bag. Feed the bag and colon into the tunnel from below while placing gentle traction from above. Suction can be placed inside the bag to facilitate delivery of the conduit if necessary.


Fig. 10.7
The prepared colonic graft is passed into the bag for delivery to the neck
6.
Microvascular anastomosis:
(a)
The vascular augmentation is performed prior to the esophagocolostomy.
(b)
A Wood’s lamp can be used to assess the vascularity of the colon prior to anastomosis (Fig. 10.8).


Fig. 10.8
A Wood’s lamp can be used to assess the perfusion to the colonic conduit prior to anastomosis
(c)
The operating microscope is used to prepare the recipient vessels.
(d)
A 2-mm to 4-mm coupler device is typically used to create the venous anastomosis.
(e)
Saphenous vein grafts can be used to compensate for length issues.
(f)
Venous anastomosis is performed prior to arterial anastomosis, to lessen congestion.
(g)
With the aid of the operating microscope, the arterial anastomosis is typically performed using 9-0 nylon sutures.
7.
Get Clinical Tree app for offline access

Esophagocolonic anastomosis:
Care is taken not to disturb the vascular anastomosis while the anastomosis is being performed. At least three anastomotic techniques are available to connect the esophagus to the colon:
(a)
Stapled, functional end-to-end. This technique is also referred to as the modified Collard or Orringer technique. The proximal segment of the esophagus is positioned adjacent to the segment of colon in a side-by-side fashion. The tip of the colon is stapled closed and the colon is passed behind the esophagus. A tacking suture is used to hold the bowel in this position. An enterotomy is created 45–60 mm from the terminal end of the colon and Endo GIA™ 60-mm (purple tristaple for Covidien or blue staple for Ethicon) single stapler ends are passed into the opened end of the esophagus and the antimesenteric enterotomy of the colon. By firing the stapler, a functional end-to-end anastomosis is created. The “hood” is closed with interrupted absorbable sutures, or alternatively with a TA™ stapler if there is adequate residual lumen.
(b)
Hand-sewn end-to-end or end-to-side (either single-layer or double-layer). An interrupted absorbable suture is typically used for this anastomosis (Fig. 10.9).
Fig. 10.9
After the neck has been prepared and the colon delivered, the esophagocolonic anastomosis is performed. If the conduit is supercharged, the enteric anastomosis is performed after the microvascular anastomosis. This image depicts the hemi-amnubriectomy, resection of the head of the clavicle, resection of the head of the first rib, and preservation of the ligamentous attachment between the first rib and clavicle. Anastomosis can be performed with a double-layer hand-sewn technique or stapled
(c)




Stapled with circular EEA™ device. The anvil is placed into the terminal end of the esophagus and a purse-string 3-0 Prolene suture is used to secure all layers of the esophageal wall tightly around the anvil. The circular stapler is passed into the proximal open end of the colon and through the antimesenteric side of the bowel to join to the anvil. Once the two devices are coupled and the stapler is fired, the rings are inspected and the terminal end of the colon is closed with a longitudinal staple line. This technique is not our choice for an anastomotic technique, as we have seen blow-outs of this staple line. It is important to be sure that the remaining defunctionalized limb is short because the limb may act as a pseudo–Zenker’s diverticulum if it is left too large.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








