Neesh Pannu, Marcello Tonelli
Epidemiology and Prognostic Impact of Acute Kidney Injury
Over the last decade, there has been a paradigm shift in our understanding of acute kidney injury (AKI). Although the condition was initially described and defined as a complete loss of kidney function, it is now widely recognized that lesser degrees of kidney injury have important implications for health. AKI represents a heterogeneous clinical syndrome with multiple causes rather than a specific disease. However, whether occurring in isolation or in critically ill patients with multiple organ failure, AKI (as defined by small, often reversible changes in kidney function) is consistently associated with an increased risk of adverse outcomes.1 This chapter reviews the incidence, risk factors, and outcomes associated with AKI as well as recent evidence linking AKI to the development of chronic kidney disease (CKD).
Incidence of Acute Kidney Injury
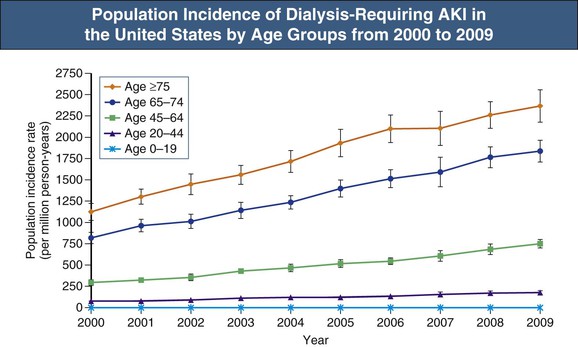
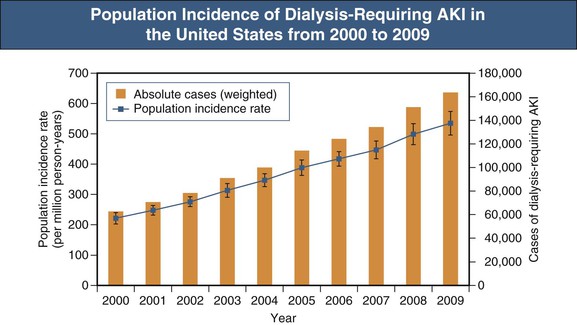
The incidence of AKI in unselected hospitalized patients has been estimated to be 0.4% to 18% depending on the definitions used, and AKI accounts for 1% to 4% of all hospital admissions. Several large U.S. studies suggest that the incidence of AKI in hospitalized patients has increased dramatically over the last several decades; one study suggested that the number of hospitalizations of patients with a diagnosis of acute renal failure (ARF; defined by International Classification of Diseases, Ninth Edition [ICD-9] codes) increased from 35,000 in 1979 to 650,000 in 2002—an increase of 13% per year.2 Available studies are based on ICD-9 diagnostic codes, which are highly specific for AKI (defined as a 100% increase in serum creatinine) but are relatively insensitive, especially for milder forms of AKI. Thus the reported incidence of AKI in these studies is likely a gross underestimate of the true incidence. Also pointing to an increased burden of AKI in the general population are the observed 10% annual increase in acute dialysis episodes in the United States between 2000 and 2009 and the twofold increase in the number of deaths attributable to AKI over a similar period (Fig. 72-1).3 The reasons underlying the increased incidence of AKI have not been determined but are likely related to increasing patient age and a higher burden of comorbidity, including a higher prevalence of CKD. Although these studies showed a decrease in attributable mortality over time, AKI survivors had prolonged hospital length of stay and a greater requirement for posthospitalization care,4 therefore incurring significantly increased health care costs.5
The incidence of AKI as determined by use of consensus definitions based on serum creatinine (SCr) and urine output has been best characterized in critically ill populations in which laboratory and urine output data are frequently measured. Despite the use of common definitions for AKI in these populations, multicenter studies have reported the incidence of AKI to be 10% to 67%, likely reflecting case mix differences among health care systems and countries.
Causes of Acute Kidney Injury
The causes of AKI in hospitalized patients have not been well characterized. However, several smaller studies have reported acute tubular necrosis (nephrotoxic and ischemic) and prerenal causes to account for the majority of patients (see also Chapter 69).6 Other potentially modifiable causes of AKI include more widespread use of radiocontrast and other nephrotoxic medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, diuretics, and chemotherapeutic agents. Exposure to potentially nephrotoxic medications is particularly common in patients with CKD, which further suggests that AKI could have increasingly important effects on the incidence of CKD.
Risk Factors for Acute Kidney Injury
Risk factors for AKI have been determined in a variety of clinical settings, including cardiac surgery, contrast-induced AKI, and critically ill populations; however, risk prediction models that accurately predict the occurrence of AKI have been elusive. Diabetes and volume depletion as a result of drugs, gastrointestinal losses, and intercurrent illnesses are well described risk factors for AKI. Nonmodifiable risk factors common to all populations are presented in Box 72-1. Recent observational studies have more accurately quantified the risk associated with some of these factors.
Age
The incidence of AKI is highest in people aged 65 and older, and an independent association exists between AKI and older age (Fig. 72-2).2,3 In a community-based prospective study, the very elderly (aged 80 to 89) were 55 times more likely to develop AKI than adults younger than the age of 50.7 The association between age and AKI is found in studies that use administrative data (ICD-9 codes) to define AKI, and also in large databases in which inpatient and outpatient SCr values are used to define AKI. There are several possible reasons for this association: (1) structural and functional changes associated with age that lead to diminished nephron reserve and reduced renal capacity for autoregulation; (2) accumulation of comorbidities (e.g., vascular disease, diabetes, hypertension, CKD), which increases susceptibility to AKI; and (3) increased exposure among the elderly to medications (ACE inhibitors, NSAIDs, diuretics) and procedures (surgery, diagnostic testing with radiocontrast) that are associated with the development of AKI.8
Chronic Kidney Disease
Chronic kidney disease appears to be among the most potent risk factors for AKI after exposure to radiocontrast, major surgery, and other medical conditions. A U.S. study demonstrated a direct relationship between underlying CKD stage and AKI in which renal replacement therapy (RRT) was required,9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree