Fig. 1
Algorithm in patients presenting with suspicious infectious gastroenteritis
2 Infectious Enteritis and Colitis
2.1 Salmonellosis
Gastroenteritis infection with non-typhoidal salmonella often results in gastroenteritis which is indistinguishable from that caused by other bacterial or viral pathogens. It is usually self-limited, and fever and diarrhoea resolve within 3 and 7 days, respectively. In a minority of patients (< 5 %), particularly neonates, infants, elderly and immunocompromised patients, carriage of the pathogen and/or a bacteraemia is prolonged with endovascular or localised (intra-abdominal, central nervous system, pulmonary) infections.
Sonographic features of Salmonella enterocolitis have been described both in children and adults. The first report described ileocaecal wall thickening and lymph node enlargement in a patient with typhoid fever (Puylaert 1989). Further series confirmed that Salmonella enteritis is usually seen as symmetric and homogeneous thickening (up to 7 mm; range 5–11 mm) of the wall of the terminal ileum and proximal colon (Fig. 2), sometimes with a small amount of free peritoneal fluid and more often associated with enlarged mesenteric lymph nodes (Hennedige et al. 2012; Mathis and Metzler 1992). However, sometimes colonic involvement may be seen in the absence of ileal involvement mimicking a pseudomembranous colitis (Adeniran et al. 2005).
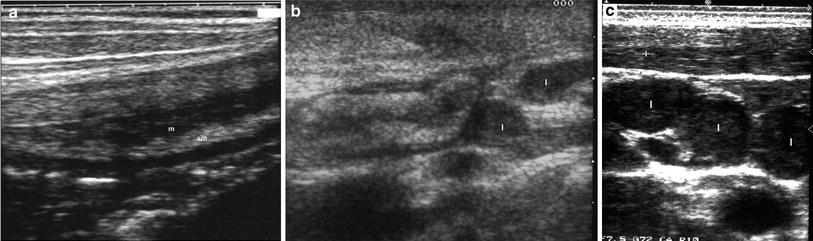
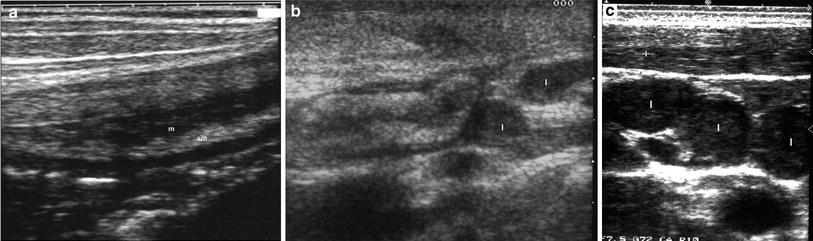
Fig. 2
Sonographic features of gastroenteritis infection with non-typhoidal salmonella in a 16-year-old female. Ultrasound showed marked wall thickening of ileum a, b and caecum, confined to mucosa (m) and submucosa (sm) and multiple enlarged mesenteric lymph nodes (l) distributed in “rosary-like” appearance c
In children, increased colonic wall thickening has been observed in up to 40 % of cases. The mean thickness was 6.2 mm, resulting predominantly from a gross submucosa oedema. Peristalsis has been described to be either increased or attenuated. Ascites has been observed in 60 % of patients and enlarged mesenteric lymph nodes in less than 10 % of patients (Ueda et al. 1999). In children, the sonographic detection of ascites and the increased colonic wall thickening correlated well with serum levels of C reactive protein and stool occult blood and, therefore, these may be useful signs by which to determine the severity of salmonella enterocolitis. However, whether they have also a prognostic factor is still unknown. In this regard, the persistence of positive stool culture 3 months after infection may result in the persistence of slight bowel wall thickening and in enlarged intra-abdominal lymph nodes (Fig. 3). Sonographic detection of ascites or intra-abdominal fluid in children with infectious enteritis, can distinguish Salmonella enteritis from colitis due to Rotavirus where ascites is usually absent (Ueda et al. 1999; Bass et al. 2004).
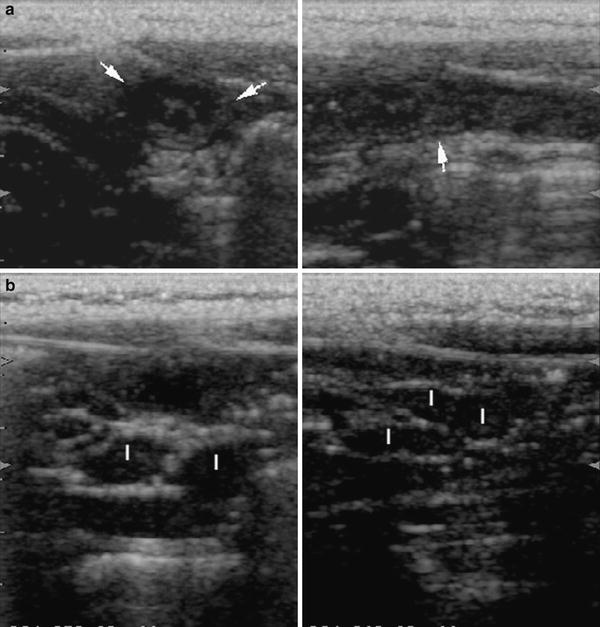
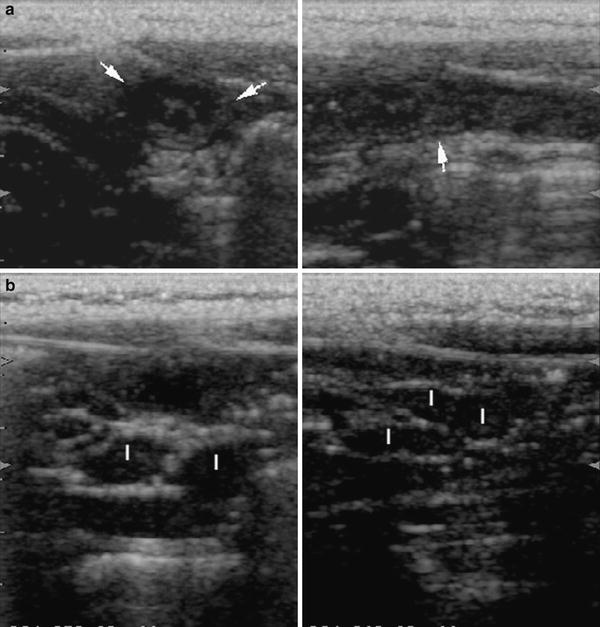
Fig. 3
Presence of a slight bowel wall thickening (arrows) and b enlarged intra-abdominal lymph nodes (l) in a 10-year-old patient with persistence of positive stool culture 3 months after infection with Salmonella
Typhoid fever is a systemic infectious disease caused by Salmonella typhi, characterised by fever, paradoxical bradycardia, abdominal pain and a rose coloured rash. Sonographic findings of typhoid fever in children and young patients (4–20 years) have been assessed in an endemic area in India. In a series of consecutive patients suspected to be having typhoid fever, the most frequent findings at abdominal ultrasound performed within three days of the onset of fever were splenomegaly (100 %), ileal and caecal thickening (85 %), mesenteric lymphadenopathy (77 %) and thickened gallbladder walls (62 %) (Mateen et al. 2006). A high rate of mesenteric lymphadenopathy (70 %) in typhoid fever has been also reported in another study form Pakistan (Nakachi et al. 2003) and in adult patients in an Italian area with high incidence of Salmonella typhi infection. In this study, the wall thickening of the ileum and/or ascending colon was reported in 36 % of patients and mesenteric lymph node enlargement in 56 % of patients (Tarantino et al. 1997).
2.2 Shigellosis
Shigellosis is the main bacterial cause of dysentery and should be taken into consideration in patients presenting with bloody diarrhoea. It is an acute bacterial infection caused by Shigella species (S. dysenterie, S. flexneri, S. sonnei) usually involving the distal colon and progressively decreasing in the more proximal segments of the large bowel. Sporadic case reports have depicted the sonographic features of shigelliosis. A diffuse wall thickening (8 mm) with distinct layer stratification in the descending and sigmoid colon in an 81-year-old woman was observed, ruling out the presence of an ischaemic colitis on the basis of clinical history and sonographic findings (Fujii et al. 2001).
2.3 Yersiniosis
Yersiniosis is bacterial zoonosis caused by infection with one or other of two enteropathogenic Yersinia species: Y. enterocolitica or Y. pseudotuberculosis, which are transmitted to humans predominantly via the oral route. The most frequent clinical manifestations of Y. enterocolitica are enteritis or enterocolitis and mesenteric adenitis presenting with fever, abdominal pain and diarrhoea, which is often bloody and persists for an average of 2 weeks, but may last up to many months during which symptoms diminish. In older children and adults right-sided abdominal pain and fever may be the predominant symptoms and may be confused with appendicitis. This presentation is much more common with Y. pseudotuberculosis, which is characterised by mesenteric adenitis and terminal ileitis. In a small proportion of cases, skin rash, joint pains, bacteriaemia can occur. The results of routine laboratory tests are often nonspecific and isolation of these micro-organisms from faeces is difficult, being impaired by their slow growth and overgrowth of other bacteria. Serologic tests, namely specific IgA and IgG antibodies to Yersinia or antigen detection in biopsies may be used, but are not widely available (Stolk-engelaar et al. 1996). Therefore, in patients with yersiniosis, abdominal ultrasound can be of assistance by excluding acute appendicitis and showing inflammatory changes in the terminal ileum and proximal colon. In the acute phase of the disease, sonography reveals thickening of the bowel wall (usually ranging from 7 to 10 mm), which is characterised by regular contours and hypoechoic echopattern (Fig. 4). Enlarged lymph nodes are always present, in numbers of 2–6 per patient, and detectable in the right iliaca fossa and along the iliac vessels (Matsumoto et al. 1991). The lymph nodes are usually sharply demarcated, oval or roundish, hypoechoic, with a variable diameter usually not exceeding 25 mm, sometimes presenting as an abdominal mesenteric mass with coalescent lymph nodes containing areas of necrosis or as an abscess (Jelloul et al. 1997; Pallister and Rotstein 2001; Perdikogianni et al. 2006) (Video). In patients with Yersinia sepsis, particularly if affected also by alcoholism, malnutrition or iron overload, ultrasound may reveal liver abscesses (Strungs et al. 1995; Leyman et al. 1989).
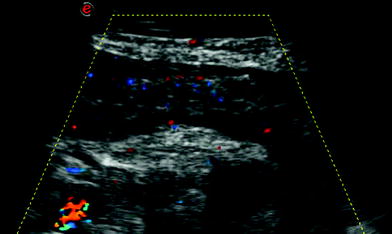
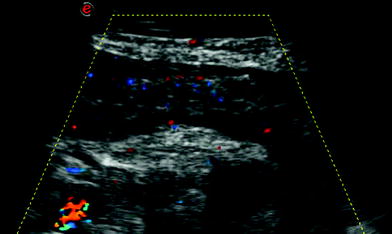
Fig. 4




Infectious ileocecitis due to Yersina enterocolitica in a 21-year-old male with clinical signs of appendicitis. Ultrasound showed wall thickening of ileum with hypoechoic echopattern and increased vascularization, a complex mesenteric mass with a small fluid area (Video) within, and enlarged mesenteric nodes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








