Indications
• The tumor does not have findings suggesting massive submucosal invasion (more than 1,000 μm) by endoscopic examination
• Tumor diameter less than 20 mm
Contraindications
• Impaired organ function (cardiovascular, respiration, liver, kidney)
• Life expectancy less than a few years because of comorbidity
• Uncorrectable bleeding tendency
Contraindications of EMR
EMR is a less invasive treatment that is applicable even in poor-risk patients. However, there are times that serious complications occur such as perforation and bleeding, even for lesions that seem to have good prognosis with EMR. Therefore, patients should not undergo EMR if the risk of the procedure seems to be more than the benefit. Contraindications are described in Table 3.1.
Instruments Used to Carry Out the Procedure
Instruments required to carry out EMR are described in Table 3.2. Snare is a mandatory instrument for all EMR procedures. A high-frequency electrosurgical generator is also useful to prevent post-EMR bleeding. Injection needle and injection solutions are required to obtain submucosal elevation [6, 7]. The injection needle is 23 or 25 G and the needle length is 4 or 5 mm. Normal saline is widely used as an injection solution because of its inexpensiveness. On the other hand, a hypertonic solution such as glycerol or hyaluronic acid is helpful for larger and superficially elevated lesions as it achieves better and more sustained submucosal elevation [8, 9]. Endoclips are used for hemostasis and for closure of a post-EMR ulcer. Net forceps or basket forceps are used to retrieve the specimen.
Table 3.2
Instruments used to carry out EMR
• High-frequency electrosurgical generator |
• Snare |
• Needle for submucosal injection |
• Injection solution |
• Endoclips |
• Device for specimen retrieval |
Technique
EMR techniques are classified into two representative procedures: snare polypectomy and strip biopsy method. There have also been recent modifications to these procedures.
Snare Polypectomy (Fig. 3.1a)
Fig. 3.1
(a) The author illustrates the basic steps of snare polypectomy. (b) Polypectomy by strip biopsy method in a flat lesion. A submucosal injection raises the lesion after which a snare is used for polypectomy
This kind of procedure is especially useful for pedunculated lesions. An electrocautery snare is passed over the polyp and around the stalk of the polyp. The loop of the snare is tightened. An electric current is then passed through the snare loop. In case the stalk is thick, the stalk is ligated using an endoclip or endoloop before resection for prophylaxis of bleeding.
Strip Biopsy Method (Fig. 3.1b)
In this procedure, a solution is injected into the submucosa in order to lift the lesion prior to snarectomy. Strip biopsy method is applicable for sessile, superficially elevated (0–IIa based on Paris classification [10]), and depressed (0–IIc) lesions because snare polypectomy is difficult. Submucosal injection makes a space between the lesion and muscle layer and thus can prevent delayed perforation due to deep thermal injury.
Other Techniques
Cold Snare Polypectomy
This procedure was first reported by Tappero et al. in 1992 [11]. The lesion is resected by the same fashion as snare polypectomy but without conduction of electric current. The advantage of this technique is that it may reduce the risk of delayed perforation. A good candidate for this technique is a diminutive polyp. One randomized controlled study revealed similar post-procedural bleeding rates when cold snare polypectomy was compared to conventional snare polypectomy for the treatment of small colorectal polyps [12].
Precutting EMR
Precutting EMR is a technique in which partial or circumferential mucosal incision is performed using electrocautery devices prior to snaring [13, 14]. This technique enables secure margination of large and superficial lesions, and it is less time-consuming compared to the more technically difficult endoscopic submucosal dissection.
Tips and Tricks
For technical success of EMR, there are three important factors: positioning, submucosal injection, and snaring.
Positioning
When performing EMR, the ideal position of the lesion is 6 o’clock on the monitor because endoscopic forceps are delivered from this location. If the lesion locates itself on the opposite side, it is necessary to move the lesion to the ideal position by rotating the scope, by shortening the loop, and by changing the body position.
Submucosal Injection
Good submucosal elevation is a key to successful EMR. Ideal submucosal injection is one that makes snaring easy, better visualizes the lateral margins (especially the oral margin), and makes an adequate space between the lesion and muscle layer. For large lesions, the injection should be started from the oral side of the lesion (farthest from the scope) which is the more difficult area to visualize, and subsequent injections can be applied to the anal side of the lesion as necessary. A retroflex view is sometimes helpful for making an injection on the oral side.
Pitfalls
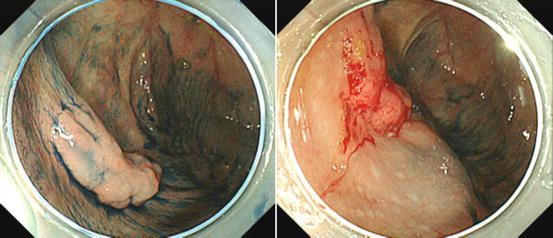
Non-lifting Sign
If the lesion invades into the submucosa massively, fibrosis may occur beneath the lesion. In such a situation, the lesion does not lift in spite of submucosal injection (non-lifting sign, Fig. 3.2). A non-lifting sign is diagnosed when the lesion itself does not elevate, whereas the surrounding mucosa lifts by adequate amounts of submucosal injection. This sign can predict pathological massive submucosal invasion with a sensitivity of 83 % and a specificity of 100 % [15]. EMR is contraindicated, and surgical resection is recommended when a non-lifting sign is present because EMR is not only non-curative but there is also an increased risk of perforation.