Fig. 4.1
Subtypes of laterally spreading tumors (LSTs). (a) LST-G (H; homogenous type). (b) LST-G (MIX; mixed type). (c) LST-NG (F; flat elevated type). (d) LST-NG (PD; pseudo-depressed type)
For en bloc resection of lesions with a large size (e.g., >20 mm) and/or submucosal fibrosis, conventional EMR is inadequate. If multi-fragmental resection is performed, histologic examination is difficult, and furthermore the local recurrence rate could be higher than that of patients with en bloc resection. Based on their retrospective study of clinicopathological analysis of lateral spreading tumors >20 mm in the colorectum, Uraoka et al. reported that the indications for ESD were as follows: (1) LST-NG (depressed type involving pseudo-depressed type) >20 mm, (2) LST-G (mixed type) >40 mm, (3) lesions with a non-lifting sign, (4) local recurrence/residual tumor following endoscopic resection >10 mm, and (5) lesions with involvement of the ileocecal valve or dentate line [1].
The indication for ESD is determined by visual endoscopic features by using chromoendoscopy, magnifying endoscopy, and occasionally endoscopic ultrasonography (EUS). EUS is used for special cases of scarred lesions or those with suspicion of massive submucosal invasion by magnifying endoscopy. Recently, equipment-based image-enhanced endoscopy (IEE) such as narrow-band imaging (NBI), flexible spectral imaging color enhancement (FICE), and i-scan has replaced chromoendoscopy to some extent. Biopsy is not necessary because the prediction of malignancy is completely accomplished by chromoendoscopy, and biopsy may cause unnecessary submucosal fibrosis which makes the following ER more difficult and more risky. Despite extensive effort to preoperatively stage a lesion, this is not possible in all gastrointestinal (GI) neoplasms, and it sometimes becomes necessary to resect a lesion for accurate histologic evaluation.
Instruments Used to Carry Out the Procedure
The colon is a long complicated organ, and anatomic features vary from person to person. In addition, due to the presence of adhesions in some cases, it could be difficult to maneuver a scope freely. Therefore, in order to perform colorectal ESD safely and surely, it is necessary to possess knowledge and understanding of endoscopes and the accompanying instruments.
Endoscope
It is preferable for the endoscopes to be equipped with a water-jet system to wash away blood or mucus from the area of interest. ESD is principally carried out by using a single-channel upper gastrointestinal endoscope with a water-jet system (GIF-Q260J; Olympus Medical Systems Co, Tokyo, Japan), because of ease of manipulation of a more narrow scope. In case of tumors located in the proximal colon which are not reachable by the upper endoscope, a slim colonoscope with a water-jet system (PCF-Q260JI; Olympus Medical Systems Co, Tokyo, Japan) is used.
Knife
Various types of knives have been developed by Japanese endoscopists, and improvements continue to be made. Since their mechanical and electrical properties are different in how they cut, each knife must be used to understand the specific characteristics of a particular device. ESD devices are classified into those with non-insulated and insulated tips (Fig. 4.2a, b). Both knives also have a variety of merits and drawbacks.




Fig. 4.2
ESD knives. (a) Non-insulated type: FlexKnife (Olympus Medical Systems, Tokyo, Japan), DualKnife (Olympus Medical Systems, Tokyo, Japan), TriangleTipKnife (TT knife) (Olympus Medical Systems, Tokyo, Japan), Splashneedle (PENTAX Medical, HOYA Corporation), HookKnife (Olympus Medical Systems, Tokyo, Japan), Jet B-knife (Zeon Medical Inc.), needle knife (Olympus Medical Systems, Tokyo, Japan), FlushKnife/FlushKnife BT (Fujifilm Corporation). (b) Insulated type: IT knife2 (Olympus Medical Systems, Tokyo, Japan), IT knife nano (Olympus Medical Systems, Tokyo, Japan), SAFEKnife (Fujifilm Corporation), Mucosectom (PENTAX Medical, HOYA Corporation), ClutchCutter (Fujifilm Corporation) (All figures courtesy of Fujifilm Corporation, Olympus Medical Systems, PENTAX Medical, or Zeon Medical Inc.)
A variety of non–insulated tip-type knives exist, including the needle knife (KD-1L-1; Olympus Medical Systems, Tokyo, Japan), FlexKnife (KD-630L; Olympus Medical Systems, Tokyo, Japan), DualKnife (upper length KD-650L and colonoscope length KD-650Q; Olympus Medical Systems, Tokyo, Japan), HookKnife (upper length KD-620LR and colonoscope length KD-620QR; Olympus Medical Systems, Tokyo, Japan), FlushKnife (Fujifilm Corporation), Splashneedle (PENTAX Medical, HOYA Corporation), Jet B-knife (Zeon Medical), and TriangleTipKnife (TT knife) (KD-640 L; Olympus Medical Systems, Tokyo, Japan).
When using a non-insulated tip-type knife, it is important to visualize the submucosa directly and place the knife parallel to the muscularis propria in order to prevent a deep cut and perforation. It is possible to cut and dissect the submucosal layer in as much detail as desired using these devices, and they can be manipulated in every direction for resection. However, this dissection is time-consuming, and it is easy to make mistakes that can cause perforation. The needle knife is the oldest and simplest knife that sharply cuts the tissue at the tip of the knife. However, when applied in a perpendicular direction to the intestinal wall, the knife can easily penetrate the entire bowel wall resulting in perforation. The HookKnife has a right angle bend at the tip of the needle knife. The direction of the hook can be controlled via handle rotation, which helps in the important task of keeping the hook oriented in a parallel orientation with the bowel wall to prevent perforation. The FlexKnife has a soft, thick, and looped knife tip, which acts well to prevent perforation. Furthermore, the tip of the outer sheath is rolled over by 1 mm, which functions as a stopper to keep the depth of tissue incision constant.
Currently available insulated tip-type knives include the IT knife (KD-610L; Olympus Medical Systems, Tokyo, Japan), SAFEKnife (Fujifilm Corporation), ClutchCutter (Fujifilm Corporation), and Mucosectom (PENTAX Medical, HOYA Corporation). The devices can cut and dissect the submucosal layer of the lesion using not the tip but the “blade” portion of the knife. This makes the dissection faster, although maneuvering these knives is slightly difficult. The basic technique for using insulated tip types of devices involves the ability to pull or slide the device laterally from side to side. The IT knife has a ceramic ball at the tip of a needle knife, which insulates the tip, so that cutting is achieved not by the tip but by the blade of the needle. The best way to use it is to place the ceramic ball in the submucosal layer to hook the mucosa or the submucosal connective tissue and then pull back on the knife. This is the only way to cut smoothly using an IT knife, so the knife sometimes has to be applied blindly, which risks complications such as bleeding and perforation. Recently, a scissors-type device such as the ClutchCutter (Fujifilm Corporation) has been developed, which can grasp, cut, or coagulate the targeted tissue using electrosurgical current, and is currently in investigation to see if it ameliorates some of the risks of ESD.
The selection of electrosurgical knives depends on the operator’s preference and expertise. The endoscopist must master the basic techniques necessary to manipulate each knife, and it is important to first be skilled in the use of one knife. With time will come the ability to choose the appropriate knife for different maneuvers.
Electrosurgical Unit
The electrosurgical unit we use is the ICC 200 (ERBE Elektromedizin, Tübingen, Germany), ESG-100 (Olympus Medical Systems, Tokyo, Japan), or VIO 300D (ERBE Elektromedizin, Tübingen, Germany) (Fig. 4.3). It is necessary to place the output electrical power on a lower setting than that used for the stomach because the colon wall is very thin, and there is a real danger of perforation.
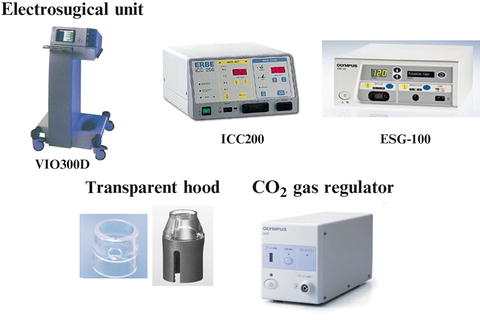
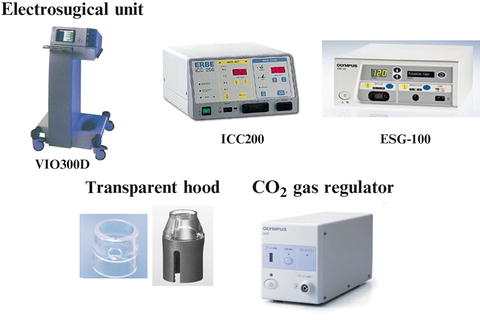
Fig. 4.3
ESD accompanying instrument: Electrosurgical unit, VIO300D (ERBE Elektromedizin, Tübingen, Germany)/ICC200 (ERBE Elektromedizin, Tübingen, Germany)/ESG-100 (Olympus Medical Systems, Tokyo, Japan); transparent hood: Transparent soft attachment (Olympus Medical Systems, Tokyo, Japan)/small-caliber tip transparent (ST) hood (Fujifilm Corporation); CO2 gas regulator (Olympus Medical Systems, Tokyo, Japan) (All figures courtesy of ERBE Elektromedizin, Fujifilm Corporation, or Olympus Medical Systems)
Transparent Hood
A transparent soft attachment which fits the tip of an endoscope (D201-11804, Olympus Medical Systems, Tokyo, Japan) or small-caliber tip transparent (ST) hood (Fujifilm Corporation) is attached to the tip of the endoscope to provide a constant endoscopic view even in the submucosal space and to apply countertraction to the connective tissue for submucosal dissection. It is essential for maintaining good position of the endoscope and visualizing the dissection line for the safe performance of ESD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








