Fig. 7.1
Illustration of twin grasper forceps to acquire tissue and pull into the endoscopic cap prior to deployment of the OTSC (Courtesy of Ovesco Endoscopy)

Fig. 7.2
Image of the over-the-scope clip (OTSC) appearance when fully closed (Courtesy of Ovesco Endoscopy)
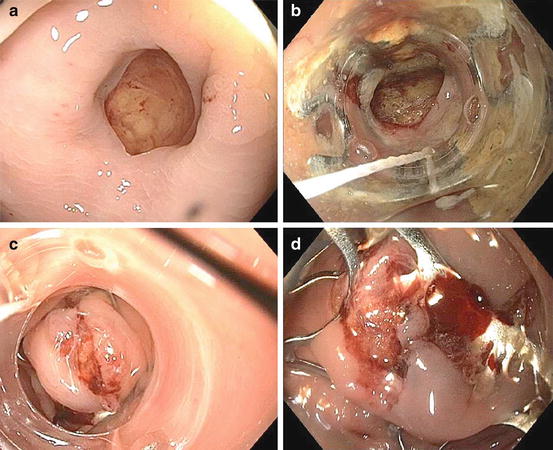
Fig. 7.3
(a) Colonic perforation from endoscope shown as mucosal defect with underlying fat. (b) Placement of OTSC endoscopic cap device over the mucosal defect. The metal clip can be seen through the clear endoscopic cap. (c) Post-deployment of the clip. The clip is entrapping the tissue and the clip no longer is seen on the exterior of the endoscopic cap. (d) Relook endoscopy showing complete full-thickness closure of the mucosal defect
OverStitch Endoscopic Suturing System
The OverStitch Endoscopic Suturing System is composed of an end cap, a needle driver handle, and an anchor exchange catheter (Fig. 7.4a). The distal tip of the endoscope is attached to the end cap, which has a hinged, curved, hollow needle body that opens and closes in an arc (Fig. 7.4b). The needle driver handle opens and closes the suture arm. The suture cassette contains a suture that is attached to a tissue anchor, which acts as the tip of the suturing needle, and attaches to the suture arm. After a suture is positioned through tissue, the anchor exchange catheter allows the tip of the needle to retract and pierce additional tissue [2] (VIDEO 1).
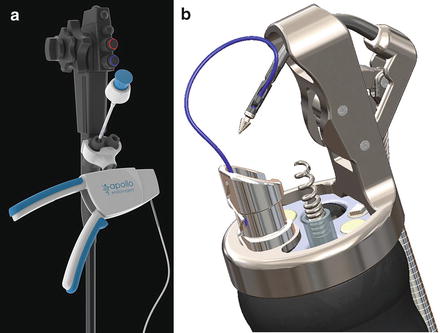
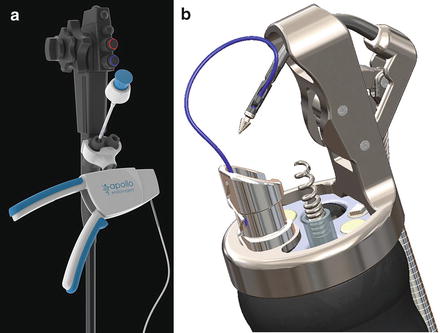
Fig. 7.4
(a) Needle handle driver attached to endoscope. (b) End cap device attached to the distal end of the endoscope (Both: Courtesy of Apollo Endosurgery)
One advantage of this suturing method is that it allows continuous or interrupted stitches to be made of various lengths [13, 20]. The endoscope does not need to be removed from the lumen for reloading needles or cinching. Furthermore, each stitch is finished with intracorporeal knot tying with a uniquely designed cinching device [20]. Since the technique is not suction based, the depth of tissue needle penetration can accurately be predicted [12].
Cardiac Septal Defect Occluders
The Amplatzer Septal Occluder is a dumbbell-shaped device composed of 2 self-expandable, umbrella-shaped disks made of nitinol mesh with polyester fabric that are constrained within a 70-cm delivery catheter and deployed over an endoscopically placed guidewire [14, 16]. The occluder is a US Food and Drug Administration-approved device for the closure of atrial septal defects [14]. The polyester fabric is sewn securely to each disk to help close the hole and serve as a foundation for growth of tissue over the occluder after placement [15, 16]. The device also possesses radiopaque marker bands that can be used under fluoroscopy [16]. Although the delivery catheter is too short to be passed through an endoscope, a guidewire can be inserted under endoscopic guidance. When the endoscope is withdrawn, the occluder can be reintroduced on the guidewire [16]. The device apposes the wall on each side of the defect, thus occluding it and creating a platform for subsequent tissue ingrowth and epithelialization [16]. These devices can be found in a variety of waist diameters and lengths depending on the defect that needs closure [2].
Tips and Tricks
Some instruments are available to facilitate the use of the OTSC including reloaders, twin graspers, and anchors. Reloaders allow for mounting of additional clips onto the applicator cap after the initial clip is deployed and can be used if more than one clip is to be placed during the same phase of the procedure [2]. The twin grasper is useful for large defects and chronic defects associated with induration in light of its ability to facilitate tissue apposition before clip deployment. The anchors are used to retract fibrotic tissue into the cap. Anchors consist of a long catheter with 3 retractable needle pins that pierce the tissue when deployed to anchor the tissue. Subsequently, the tissue can be pulled into the applicator cap and the clip can be deployed [2].
The key element to technical success is the positioning of the lesion within the OTSC cap [1]. Misfiring to one side of a lesion can affect successful deployment of a second clip over the defect.
Pitfalls
Clips such as the OTSC are more difficult to apply in cases of larger defects because of an inability to accomplish deep-tissue capture due to low closure force and restricted opening distance between the jaws of the clip [2]. Furthermore, in cases where the tissue is inflamed, indurated, and fibrotic such as the case of chronic fistulas, endoscopic clips are particularly troublesome and may result in challenging and protracted procedures, failure of adequate tissue apposition, and inability to properly deploy the OTSC [1, 2].
Clinical Outcomes and Results that Need Discussion
OTSC
Overall success rates of OTSC in the literature range from 75 to 100 % for closure of iatrogenic gastrointestinal perforations, 38 to 100 % for closure of gastrointestinal fistulas [11], 50 to 100 % for anastomotic leaks, and 71 to 100 % for bleeding lesions [10]. The OTSC system has been used to repair perforations at esophageal, gastric, small bowel, and colonic sites [21–23]. Voermans et al. [21] reported successful endoscopic closures by location: 100 % success for esophageal, 100 % for gastric, 75 % for small bowel, and 92 % for colonic perforations.
Another study examined the efficacy of the OTSC in the management of both acute and chronic colorectal postsurgical leaks and fistulas. The study included cases where the fistula orifice was less than 15 mm in maximum diameter and no abscess or luminal narrowing was seen. In 14 consecutive patients, the overall success was 86 % (7/8) in acute fistulas and 83 % (5/6) in chronic fistulas. Two cases of rectovaginal fistulas were included among the group studied [24]. Not only has this OTSC technique proven itself to be important in the management of acute and chronic gastrointestinal closures, its use has been shown to decrease the need for surgery and length of hospital stay [25].
OTSC has had expanding indications including stent fixation and fistula repair among others. A recent retrospective case series by Monkemuller et al. [8] evaluated outcomes of patients treated with the OTSC. Indications included gastrointestinal bleeding, gastrocutaneous fistulas, esophagotracheal and/or esophagopleural fistula, resection of submucosal tumor, stent fixation, and anastomotic leak after esophagectomy. A total of 20 OTSC system applications were used in sixteen patients with various GI defects with an overall success rate of 75 % (12 out of 16 patients). The highest success rates were found in patients with gastrointestinal bleeding (100 %), while lower rates were found in patients with esophagotracheal or pleural fistulas (four out of six patients, 66 %). These results were supported by data in a retrospective review by Baron et al. [1] which found that in 45 patients treated with OTSC, immediate hemostasis was achieved in 100 % of patients treated for gastrointestinal bleeding and anastomotic leaks and fistulas were closed in 65 % of patients.
The unique features of the OTSC including its higher stability and ability to grasp more tissue and apply a greater force make it conceptually superior to other endoscopic clipping devices [1, 10]. Von Renteln et al. [6] compared endoscopic clips and over-the-scope clips for closure of NOTES gastrostomies in animals and found that OTSC in combination with a twin grasper was able to safely and efficiently close NOTES gastrostomies up to 18 mm in diameter with a decreased risk of leakage and intra-abdominal infection when compared to closure with standard endoscopic hemostatic clips.
The relatively recent evolution of this technology means little literature regarding the long-term efficacy and potential complications of the over-the-scope clip. The OTSC is designed to be permanent. There are no current reports of complications arising in the gastrointestinal tract secondary to clip placement [10]. Voermans et al. [21] found 19/24 clips to be present on follow-up endoscopy six months following OTSC placement for perforations of the GI tract.
OverStitch Suturing System
The first case report of the endoscopic OverStitch device was for closure of a gastrocutaneous fistula that was refractory to closure with endoscopic clips and glue [12]. A sixty-six-year-old man had a persistent gastrocutaneous fistula following PEG removal. The OverStitch suturing device was mounted on a double-channel endoscope and introduced into the stomach where three separate stitches were made and the fistula was closed completely. In one month follow-up, the fistula had healed completely and without drainage [12]. Since then, the suturing system has been used successfully to close persistent gastrocutaneous fistulas, fix esophageal stents, suture ulcers, and close large post-ESD mucosal defects [12, 13, 20]. In the case of esophageal stents, endoscopic suturing is used to prevent spontaneous stent migration [20].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








