Fig. 6.1
Operating theater
6.5.3 Infiltration
Before making the mucoperiosteal flaps to discover the lacrimal bone, a submucosal infiltration with adrenaline solution is made, in order to reduce bleeding. The site of infiltration is localized to the nasal lateral wall, near the lacrimal area, anterior to the uncinate process (Figs. 6.2, 6.3, and 6.4).

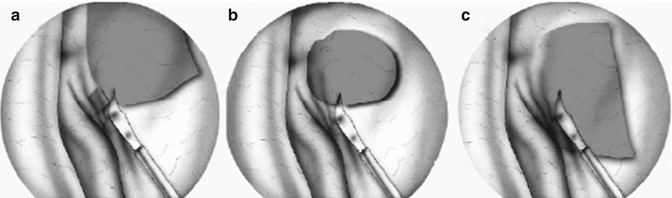
Fig. 6.2
Projection zone of the lacrimal sac. (a) Draw; (b) before surgery. TM middle turbinate, PU uncinate process, Atm middle turbinate axilla, Zps projection sac area zone

Fig. 6.3
Infiltration of the projection zone of the lacrimal area
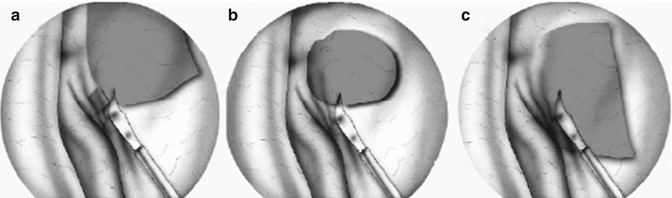
Fig. 6.4
Mucosal incision
6.5.4 Flaps Preparation
To identify the lacrimal sac region, the most important structure is represented by the uncinate process, because just anterior to it there’s the projection of the lacrimal sac. In our opinion the head of the middle turbinate, due to its great anatomic variability, is not a safe landmark. Many techniques are described to make mucoperiosteal flaps. We usually used to perform two flaps, one little posterior and one bigger superior. Until flaps are superiorly and posteriorly moved, the bony wall that recovers lacrimal sac is exposed. Mucosal incision could be produced with many instruments, such us cold knife, radiofrequency knife, and laser technique (Figs. 6.5 and 6.6).
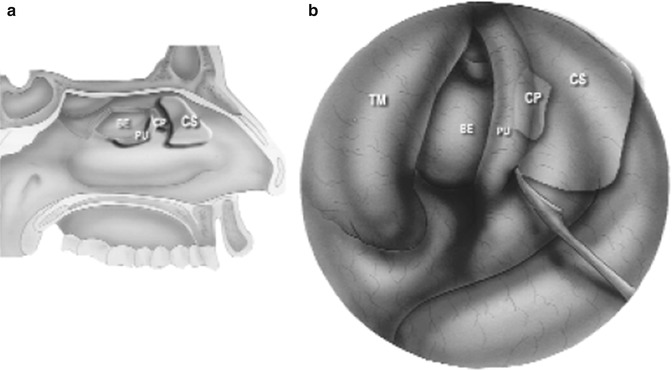
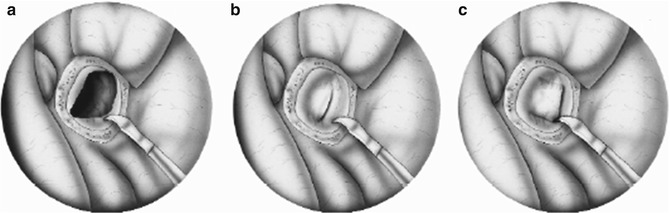
Fig. 6.5
Intraoperative view: the mucosal incision
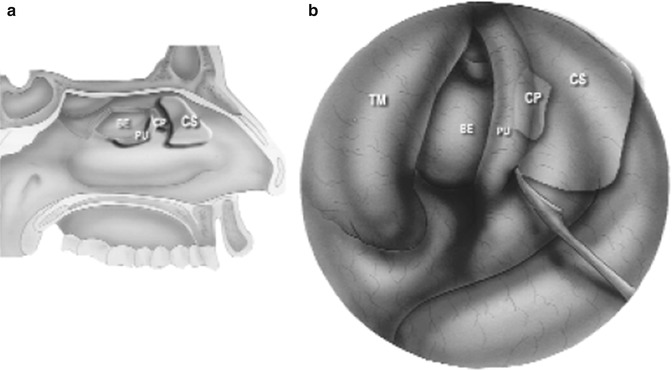
Fig. 6.6
Double mucosal flap technique
6.5.5 Laser
Currently, two techniques are used to perform endoscopic DCR: laser-assisted and “cold steel” with or without powered instrumentation. The laser method appears to be less effective than cold steel endoscopic DCR, with success rates ranging from 64 to 85 % compared with a rate of approximately 85 % for cold steel procedures. The inferior results achieved with laser DCR may be the result of the size of the ostia created, because small-ostia DCRs created by laser were found to have patency rates of only 64 % and 70 %, respectively, in two studies. Moreover, the heat generated from bone and mucosa ablation with a YAG/KTP laser may contribute to fibrosis and stenosis and consequent poor results [14].
6.5.6 Bone Drilling and Lacrimal Sac Exposure
The bony wall removal is represented by the ascending maxillary branch and lacrimal bone. In case of rich pneumatization of agger nasi, the bone removal could interest also some anterior ethmoidal cells. This step can be conducted with drill, laser, or other instruments common to sinus surgery instruments (Fig. 6.7). An interesting type of instrument is represented by piezosurgery, that we often use in this step. The peculiarity of this technology is that a better respect of soft tissue and no hot damage is produced, on the contrary of drill. This technology consents to make an exeresis of only bone tissue, with maximum respect of nerves, vessels, muscles, and in general soft tissue. The use of this instrument causes on the contrary a delay of surgical time (Fig. 6.8a, b).
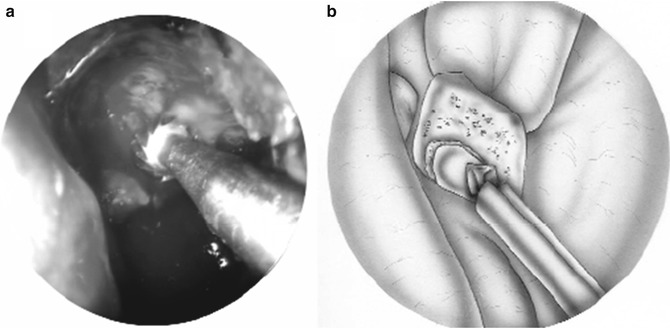
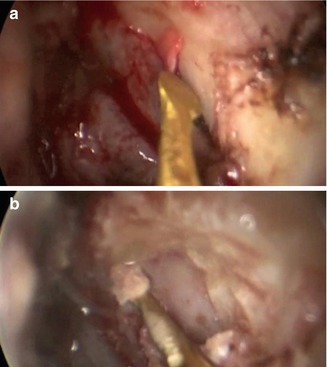
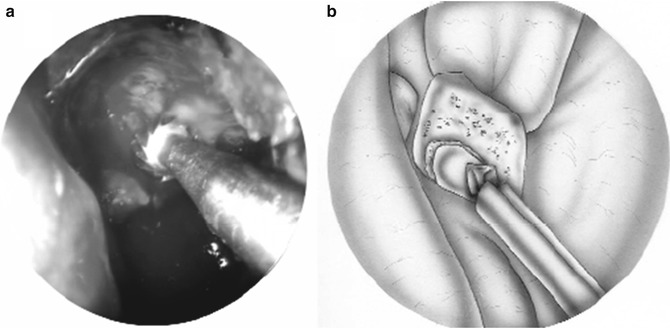
Fig. 6.7
Lacrimal bone drilling
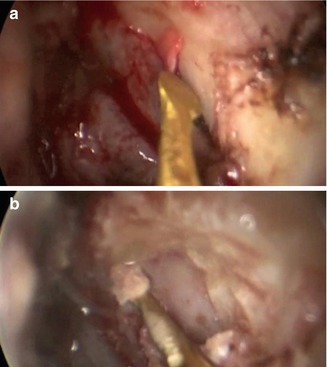
Fig. 6.8
(a, b) Lacrimal bone drilling with piezosurgery
6.5.7 Lacrimal Sac Opening
To identify with precision the medial wall of the lacrimal sac, a transillumination through the inferior lacrimal canaliculus with otic fibers can be made (Fig. 6.2b). Alternatively a sickle knife through the lacrimal canaliculi can be introduced, until sac is localized. External palpation of the lacrimal area is also a simple but effective method. Different surgical strategies to open the lacrimal sac are reported. We usually realize a mucosal posterior flap. The incision is made with a sickle knife (Figs. 6.9 and 6.10). In case of chronic dacryocystitis, with recidivant infections, a purulent secretion can be visualized in this step. An aspiration with toilette and repeated lavages of this area is done. This posterior mucosal flap is just apposed to the posterior mucoperiosteal flap, precedently realized, in order to maintain open the surgical stoma (Figs. 6.11 and 6.12). The superior mucoperiosteal flap is then repositioned under the drilled area. The use of stents is not routinely performed, but we use these in revision surgery or in fibrotic lacrimal sac (Figs. 6.13 and 6.14). Hospital dismissal in first day. The antibiotic therapy is not always recommended at home, while an accurate nasal hygiene with nasal irrigation is important. Postoperative follow-up is usually performed with endoscopic exam after 15 days and then after 2 months. In case of stent positioning, this is maintained into the nasal fossa for 2–4 months.