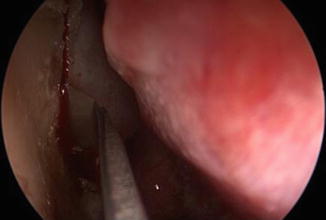
1. Endoscopic vision of a small scar tissue area where the previous DCR was performed


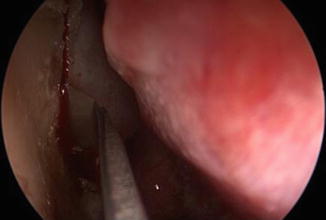
2. The incision through Tullio laser on the anterior portion of the head of the middle turbinate
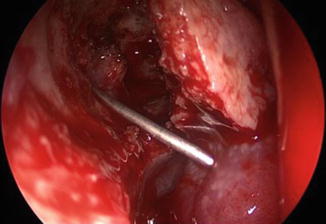
3. Creation of the superior flap close to the lacrimal sac corresponding area (1/2)


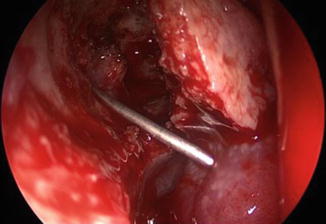
4. Creation of the superior flap close to the lacrimal sac corresponding area (2/2)


5. Copious purulent discharge from the lacrimal sac
6. Irrigation of the lacrimal pathway


7. Insertion of Bika (1/2)


8. Insertion of Bika (2/2)
8.4 Conclusions
Although several studies have focused on endoscopic or external DCR, few have compared revisional differences between previous endoscopic and external DCRs [12].
For revisional cases, endonasal DCR has several advantages:
Absence of additional scarring
Maintenance of the mechanism of lacrimal pumping by the orbicular muscle
Reduction of injury to structures of the medial canthus
Less bleeding
Shorter hospitalization
Technical facility because of anterior removal of the lacrimal bone
The possibility of correcting other conditions during the same surgical procedure, including septal deviation synechiae, granulation tissue, rhinosinusitis, nasal polyposis, and incomplete bone removal
Direct visualization of the site and amplitude of the nasolacrimal fistula
The endoscope provides excellent intranasal visualization and enables the surgeon to open the lacrimal sac with relative ease from inside the nasal cavity.
Reported success rates for endoscopic revision range from 70 to 90 % using a simple revision [13–15, 7, 16]; the second revision usually has a relatively low success rate (50 %).
The causes of failure for external or endoscopic DCR (septal deviations, incomplete removal of lacrimal bone, synechiae, granulation tissue, membrane and scar formation at rhinostomy) are easier identified and corrected at the time of revision surgery and are more accurately treated using direct endoscopic visualization [12].
Although stenting is controversial in primary surgery because of the possible induction of granulation [17, 18], it can help to prevent obliteration of the rhinostomy opening, especially in revisional cases, and to prevent restenosis of the lacrimal opening.
We conclude that it is important to correct abnormal nasal findings and to make a larger ostium during revisional DCR than during the previous procedure. Additionally, patients who had an unsuccessful first revision are more likely to have an unsuccessful additional surgery, so it is important to identify the causes of surgical failure and to correct them, especially during the first revisional surgery [12].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








