Chapter 4 Endoscopes, Guidewires, and Accessories
Endoscopes
Side-Viewing Endoscopes
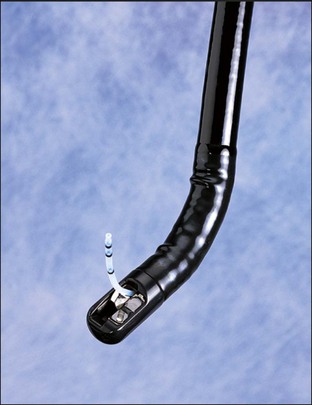
Duodenoscopes are side-viewing video endoscopes that are equipped with an elevator and are used routinely for diagnostic and therapeutic ERCP procedures. The elevator facilitates cannulation of the papilla and placement of some accessories (Fig. 4.1), while large diameter working channels of therapeutic duodenoscopes (4.2 and 4.8 mm) allow the use of large accessories. Many current ERCP endoscopes combine a large, “therapeutic” channel with a standard-size insertion tube. Smaller, 7.4-mm pediatric duodenoscopes with a 2.2-mm channel are available for examination in neonates. Unfortunately, the small channel limits the use of the endoscope to mostly diagnostic purposes since the use of smaller accessories restricts the therapeutic potential of this endoscope. In general, the standard adult duodenoscope can be used in most children above the age of 2. A jumbo-size duodenoscope (5.5-mm channel) was previously available as a “mother/baby” scope system. However, this system was difficult to manipulate and is now rarely used.
Forward-Viewing Endoscopes
Upper endoscopes, colonoscopes, and enteroscopes are occasionally used in patients with altered anatomy such as previous choledochoduodenostomy, Billroth II gastrectomy, or in patients with hepaticojejunostomy. Since conventional forward-viewing endoscopes do not have an elevator, they are limited with respect to control of accessories during cannulation or therapy. In addition, visualization of the ampulla may be limited. When using a colonoscope, “long”-length accessories may be needed, as not all standard biliary accessories are of adequate length. Initial experience with a prototype oblique-viewing endoscope (Pentax Medical, Montvale, N.J.) (viewing angle of 45 degrees, field of view of 130 degrees, 3.8-mm-diameter instrument channel, accessory elevator, and a working length of 120 cm) allowed duct access and therapy in two patients with surgically altered anatomy.1 In both patients, prior multiple attempts at ERCP with standard duodenoscope and colonoscope had failed.
Balloon-Assisted Enteroscopes
Single-balloon (Olympus America Inc., Lehigh Valley, Pa.) and double-balloon (Fujinon, Tokyo) enteroscopes enable deep intubation of the small bowel. These endoscopes have a specialized disposable overtube with an inflatable balloon that anchors the endoscope in place during shortening maneuvers. Double-balloon enteroscopes have a second balloon on the endoscope insertion tube. Balloon-assisted enteroscopes enable diagnostic and therapeutic ERCP in most patients with altered surgical anatomy (see Chapter 29).2 However, very limited accessories are available for therapeutic interventions because these enteroscopes have a 200-cm working length and small-diameter working channels. A “short” double-balloon enteroscope (Fujinon, Tokyo) has a 2.8-mm working channel and a 152-cm working length allowing all ≤7 Fr diameter standard biliary accessories to be used.3,4 Again, the combination of a forward view and the lack of an elevator limits success rate in patients with intact papilla for all enteroscopy-assisted procedures.
Echoendoscopes
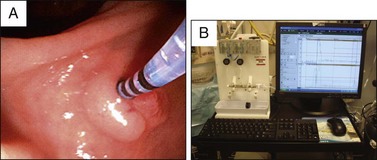
Curvilinear echoendoscopes (GF-UC140 or GF-UCT 140, Olympus America Inc., Lehigh Valley, Pa.; Pentax, Montvale, N.J.) have been used successfully to obtain access to biliary or pancreatic ducts in patients with failed ERCP or those with inaccessible papillae (see Chapters 30 and 31).5 Therapeutic curvilinear echoendoscope (Pentax, Montvale, N.J. and Olympus America Inc., Lehigh Valley, Pa.) with 3.8-mm working channel allows passage of standard ERCP accessories for transmural access and drainage of pancreatic fluid collections with ability to place large diameter (10 Fr) stents. A 19- or 22-gauge fine needle aspiration needle or cautery device (Cystotome, Cook Endoscopy, Winston-Salem, N.C., standard needle knife) can be used for puncture and entry at the defined location under real-time ultrasound guidance (see Chapter 53). The Cystotome (Fig. 4.2) is a modified needle-knife sphincterotome that consists of an inner wire with a large-diameter needle-knife tip, a 5 Fr inner catheter, and a 10 Fr outer catheter equipped with a diathermy ring at its distal tip. The proximal end of this device includes a handle with connectors for active cords and a fitting to provide for injection of contrast. The Cystotome is discussed in more detail in Chapter 30.
Accessories
Accessories are devices or pharmacologic agents that assist in the endoscopist’s accomplishment of diagnostic or therapeutic procedures. Cannulation of the desired duct is a prerequisite to successful diagnostic and therapeutic ERCP. A variety of devices are currently available to gain duct access.6 In particular, the use of sphincterotomes/guidewires and precut sphincterotomes has increased the ability to achieve deep cannulation of the desired duct.
Standard Cannulation Catheters
Standard ERCP cannulas are 5 Fr to 7 Fr catheters, with straight, tapered, or rounded tips that accept up to a 0.035-inch guidewire (Fig. 4.3, A). Use of a double- or triple-lumen device or the attachment of a side-arm adaptor will allow contrast injection without removal of the guidewire. The use of tapered (4.5 Fr–4 Fr–3.5 Fr) or ultratapered (5 Fr–4 Fr–3 Fr) tip catheters may improve ductal access. However, some tapered tip cannulas will only accommodate a smaller-caliber guidewire (0.018 to 0.025 inch). No published studies are available that directly compare cannulation success rates between standard and tapered catheters. There is a higher risk of submucosal injection using tapered tip catheters.
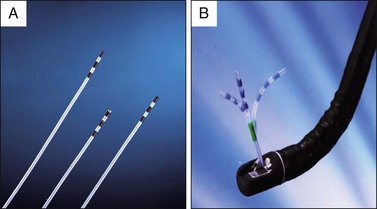
Fig. 4.3 A, ERCP cannulas. B, Swing-tip ERCP cannula.
(A, Courtesy Cook Endoscopy, Winston-Salem, N.C. B, Courtesy Olympus America Inc., Center Valley, Pa.)
Standard cannulas with or without guidewires are limited in their ability to vary the angle of approach to the papilla. The Swing-tip catheter (Olympus America Inc., Center Valley, Pa.) (Fig. 4.3, B) overcomes the limitations of conventional catheters and offers the endoscopist the ability to bend the cannula tip in either the up-down or left-right directions, thereby facilitating biliary cannulation7,8 or selective entry into the right or left hepatic ducts. The Cremer needle tip catheter (Cook Endoscopy, Winston-Salem, N.C.) is 1.8 mm in diameter and has a metal needle tip that facilitates minor papilla cannulation (Fig. 4.4, A and B). The standard pancreaticobiliary manometry catheter is a water-perfused 5 Fr catheter with a tip diameter of 3.5 Fr and is used during sphincter of Oddi manometry studies (Fig. 4.5, A). A variety of catheter types can also be used. Some manometry catheters have a longer “nose” to help maintain catheter position. The standard catheter has three side ports spaced 2 mm apart for simultaneous pressure measurement. The Lehman manometry catheter (Cook Endoscopy) sacrifices one port for aspiration of water from the pancreatic duct during infusion to prevent overfilling; this reduces the risk of post-ERCP pancreatitis (PEP).9 Standard water-perfused motility recording systems are used for sphincter of Oddi manometry. More recently, a compact water perfusion pump has become available (Mui Scientific, Mississauga, Canada) (Fig. 4.5, B). A micro transducer catheter that does not require water perfusion has also become available. Early data suggest that this catheter is associated with a lower risk of PEP.10 A detailed discussion on currently available sphincter of Oddi manometry devices can be found in a recent technology status evaluation report by the American Society for Gastrointestinal Endoscopy (ASGE).11

Fig. 4.4 A, Cremer cannula. B, Endoscopic view showing Cremer cannula and minor papilla.
(A, Courtesy Cook Endoscopy, Winston-Salem, N.C.)
Sphincterotomes
Pull-type (Erlangen) sphincterotomes were designed for performance of biliary sphincterotomy. They consist of a Teflon catheter containing a continuous wire loop with 2 to 3 cm of exposed wire exiting at a variable distance from the tip (Fig. 4.6, A). Early precut sphincterotomes were pull-type and the cutting wire extended to the tip (Fig. 4.6, A). The other end of the wire is insulated and connected to an electrosurgical unit. Over the last decade or so, endoscopists have recognized the need to angle the catheter upward to selectively enter the bile duct.12 Subsequently, prospective randomized trials comparing standard catheters with sphincterotomes have shown a cannulation rate of 84% to 97% with sphincterotomes compared to 62% to 67% with standard catheters.13,14 In addition, since sphincterotomy is performed in a large percentage of ERCPs, sphincterotomes have become the primary biliary cannulation device in ERCP.
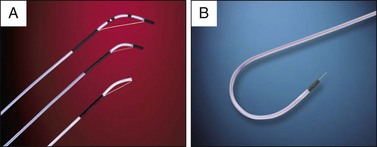
Fig. 4.6 A, Standard and precut sphincterotome. B, Needle-knife sphincterotome.
(Courtesy Cook Endoscopy, Winston-Salem, N.C.)
When sphincterotomy is performed a variety of generator currents can be used: cutting, auto-cut, coagulation, or blended. Limited data suggest that the use of a pure cutting current is associated with a lower risk of PEP15 while the use of an auto-cut mode is associated with a lower risk of intraprocedural bleeding and eliminated the “Zipper cut” phenomenon during sphincterotomy. When performing pancreatic sphincterotomy, pure cutting current is often used to reduce the risk of pancreatic duct injury and subsequent stenosis.
Rotatable sphincterotomes are designed to rotate the tip so that one can alter the desired trajectory of cannulation. Preliminary data suggest that this may be useful in improving cannulation, especially in patients with unusually oriented or distorted papillae16 or in patients with Billroth II–type anatomy. Rotatable sphincterotomes may also help orient the cutting wire during sphincterotomy. However, no published data are available to support this. A wire-guided sphincterotome with a cutting wire oriented in the opposite direction relative to standard sphincterotome is available for use in Billroth II–type anatomy (Cook Endoscopy). In addition, a sphincterotome with an S-shaped tip is also useful in patients with surgically altered anatomy.17
Guidewires are used with a standard catheter or sphincterotome to achieve deep cannulation of the bile and pancreatic ducts. In some reports, wire-guided cannulation is associated with increased cannulation success rate and a lower risk of PEP.18–20 A randomized controlled trial found no difference in cannulation success and adverse event rates between 5 Fr and 4 Fr sphincterotomes.21 For further information on biliary cannulation see Chapter 13.
Access Sphincterotomes
Precut or “access” sphincterotomy refers to a variety of endoscopic techniques used to gain access to the bile or pancreatic duct after conventional methods of cannulation have failed (see Chapter 14). Needle-knife and precut sphincterotomes are the two most commonly used devices to gain access into the bile duct. The needle-knife sphincterotome was first described by Huibregtse in 1981 and is essentially a bare wire that protrudes 4 to 5 mm from the end of a Teflon catheter (Fig. 4.6, B). There are several publications using this device. Newer versions include additional lumens for guidewire passage or contrast injection (double lumen) and both wire and contrast injection (triple lumen). The precut sphincterotome was first reported by Soehendra and the Hamburg group in 1996 (Fig. 4.6, A). This sphincterotome allows “papillary roof incision.”22 A double-lumen version has been recently introduced.23 It has the advantage of having separate lumens for contrast and guidewire. Biliary sphincterotomy can be immediately completed by using the same instrument and is facilitated by having a preloaded hydrophilic tip wire. A new needle-knife sphincterotome has an insulated tip to prevent energy dispersion from the tip of the incising needle.24 The coated-tip needle knife is believed to prevent unintentional deep cuts or perforations because it enables users to keep the sphincterotome tight in the papillary orifice. The optimal device for precut sphincterotomy is unknown because there are limited data comparing different precut techniques and devices.25
Guidewires
Ideal guidewire characteristics for gaining access to the duct of interest and traversing stricture are different than those for advancement and exchange of accessories. Guidewires with slippery and flexible leading tips are generally used for cannulation and to gain access through tight biliary or pancreatic strictures. On the other hand, stiff and taut guidewires are best used for advancement of devices such as biliary stents or dilators. Stiff and taut wires also minimize lateral deviation and facilitate forward axial transmission of forces. Friction can aid in maintaining wire tension but hinders both wire and device movement. A variety of guidewires are currently available (Table 4.1) and these vary in materials, length, diameter, and design to optimize performance.26
Table 4.1 Currently Available Guidewires for ERCP Applications
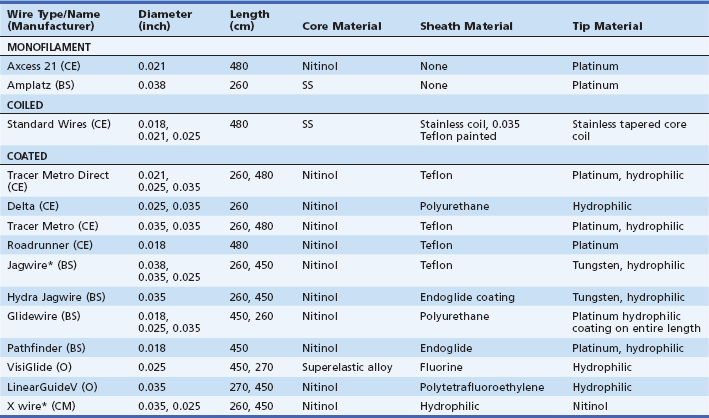
*Available in a stiff version.
Adapted with permission from Cortas GA, Mehta SN, Abraham NS, et al. Selective cannulation of the common bile duct: a prospective randomized trial comparing standard catheters with sphincterotomes. Gastrointest Endosc. 1999;50:775-779.
In general, three guidewire designs are available for ERCP applications: (1) Monofilament wires are designed for rigidity and made of stainless steel. (2) Coiled wires are stiff and flexible and have an inner monofilament core and an outer spiral coil made of stainless steel. Inner core and outer spiral coil design provides stiffness and flexibility, respectively. Most coiled wires are Teflon (DuPont, Washington, Del.) coated to minimize resistance and to optimize traversing tortuous biliary strictures because of combined stiffness and flexibility. (3) Coated or sheathed wires have a monofilament core made of stainless steel or nitinol and an outer sheath made of Teflon, polyurethane, or another lubricious polymer. The outer sheath material improves radiopacity, slipperiness, and electrical insulation properties. Coated wire tip flexibility depends on the taper of the inner core. Many wires have a platinum-tipped core to improve fluoroscopic visualization. The configuration of the guidewire can be straight or angled (J-shaped) (Fig. 4.7, A). Some wires have graduated or continuous markings for visual endoscopic measurement or movement detection. Most wires are only minimally steerable in the radial direction.
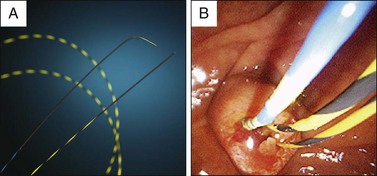
Fig. 4.7 A, Straight and angled-tip guidewires. B, Endoscopic view showing the markings on the guidewires.
(A, Courtesy Boston Scientific, Natick, Mass.)
Guidewires are advanced under fluoroscopic monitoring through a catheter or sphincterotome, which imparts stiffness and direction. Guidewire passage is easier after flushing water through dry or contrast-filled devices by minimizing friction, since contrast is “sticky.” Moistening hydrophilic portions of a guidewire prevents drying and sticking. Maintenance of wire position is critical for safe and effective use of over-the-wire accessories such as dilators and stents. The risk of wire displacement can be minimized by using guidewires that have graduated or continuous markings or movement detection, printed distance markers, and movement guides (Fig. 4.7, B). In addition, fixation of the proximal end (outside the patient) on an immobile accessory device can also decrease the risk of wire dislodgement.
Currently available guidewire types include conventional, hydrophilic, and “hybrid,” with diameters ranging from 0.018 to 0.035 inches and lengths ranging from 260 to 480 cm,27 and are summarized in Table 4.1. Wire lengths longer than 400 cm are used for “long-length” exchange of devices. Only coated wires should be used during electrocautery applications.
Data are limited regarding the relative efficacy of specific wires for ERCP applications. Clinical experience suggests that coated and hydrophilic wires improve ERCP success rates in difficult papillae or strictures. Completely hydrophilic wires (Glidewire, Boston Scientific, Terumo®, Tokyo) are slippery and can make catheter exchange difficult, leading to inadvertent displacement from ducts or strictures. However, newer combination (hybrid) wires such as Jagwire, Hydra Jagwire (Boston Scientific); FX, X (ConMed, Utica, N.Y.); ViziGlide (Olympus America Inc.); and Metro (Cook Endoscopy) provide a combination of a slippery tip with a nonslippery stiffer shaft (Fig. 4.7, A) As mentioned earlier, recent data suggest that biliary cannulation using a guidewire through a sphincterotome lowers the risk of PEP, presumably because of less trauma to the papilla and limited pancreatic injection.18–20,28 Teflon coated wires are least expensive. Hybrid wires are more user friendly but more expensive. A useful and detailed review of guidewires can be found in a recent ASGE technology assessment report.26
Exchange Assistance Devices (Short-Wire ERCP Systems)
Multiple devices are frequently required for successful therapeutic ERCP. Frequently, an exchange or series of exchanges over a previously placed guidewire is required to introduce subsequent devices. Several exchange assistance devices have been developed by different manufacturers to facilitate exchange of over-the-wire accessories in order to reduce reliance on the assistant. These devices employ the use of short-length (260-cm) guidewires and may increase efficiency while reducing fluoroscopy time.29 Potential problems with exchange assistance devices include a restriction in the choice of accessories, difficulty in reusing the same accessory during the procedure, and cost. A detailed discussion on currently available short-wire systems can be found in a recent ASGE technology status evaluation report.30
Rapid Exchange Biliary System
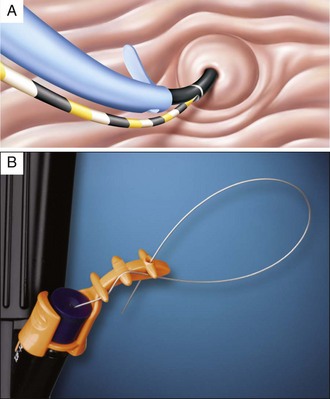
The Rapid Exchange (RX) Biliary System (Boston Scientific) is a monorail design that provides the endoscopist with control over the guidewire and subsequent exchanges. The system is composed of three integral units: a guidewire locking device (Fig. 4.8, A), a specially designed RX catheter, and a 260-cm-long guidewire. A locking device secures the position of the guidewire during exchange of over-the-wire accessories, advancement of accessories, and manipulation. The locking device can accommodate multiple guidewires that can be secured at any time and thus allows for multiple therapeutic interventions. Cannulas and sphincterotomes have a distal open channel (beginning 5 cm from the tip and extending proximally 30 cm) that allows the guidewire to exit at this point rather than at the hub of the endoscope. Once cannulation is achieved, the wire is separated from the catheter (Fig. 4.8, B) and is secured in the guidewire locking device at the biopsy port. A variety of RX accessories are available to use with this system.
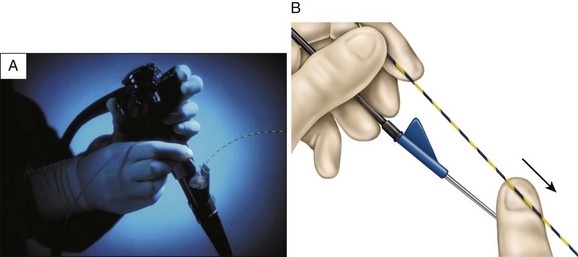
Fig. 4.8 Rapid exchange system. A, Locking device. B, Guidewire stripping from the catheter.
(Courtesy Boston Scientific, Natick, Mass.)
Potential benefits of RX Biliary System include shorter total procedural and postcannulation times and a reduction in use of fluoroscopy.31 However, cost is higher than standard long-length equipment and may limit the choice of accessories. Cost–benefit studies using the RX Biliary System are not available.
Fusion System
The main difference between this new system and the conventional design is that a side hole is placed 6 cm from the tip of the catheter (or any accessories from this line of products except the stent introducer system, in which the side hole is placed 2.5 cm from the tip) (Fig. 4.9, A). The guidewire is 185 cm long and most accessories are 220 cm long. To provide proper control of these much shorter accessories and guidewire, the system uses a special disposable biopsy valve with a locking mechanism to anchor the guidewire while performing exchanges (Fig. 4.9, B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree