Embryoscopy
Michael S. Baggish
Jacques Barbot
Few endoscopic techniques are either safe or advisable during pregnancy. However, in this regard the contact hysteroscope is a unique instrument because it requires no distending medium to be placed within the pregnancy environment, it provides vision even in the presence of mucus or other body fluids, it allows light contact with the epithelium or structure to be viewed, and it delivers true cold light. If examination is carried out in a careful, systematic manner, complications are minimal. Because the endoscope enters the uterus under direct vision, the risk of perforation is low. No perforations of the uterus have occurred in >1,000 examinations to date. The only side effect reported after examination during early or late pregnancy has been light bleeding. No pregnancy to date has been inadvertently terminated following endoscopic examination. Similarly, no patient developed an intrauterine infection as a result of contact endoscopy. Finally, unintentional rupture of the membranes secondary to contact endoscopy is rarely encountered.
Embryoscopy
Examination of intrauterine pregnancies between 4 and 10 weeks of gestation heretofore was not possible without invading the gestational sac. By means of the contact hysteroscope, the examiner may now view the living embryo without disrupting its environment (Figs. 21.1 and 21.2).
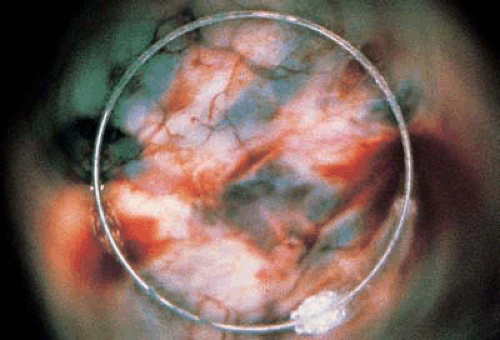
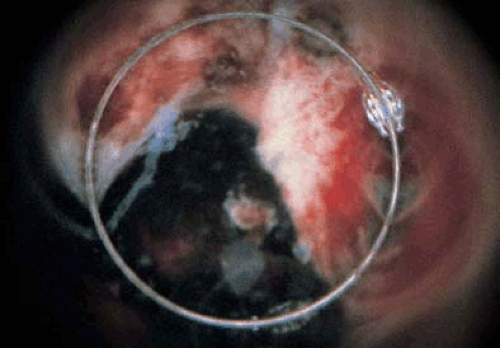
The technique of embryoscopy diverges from the routine of general contact endoscopy only after the hysteroscope has entered the uterine cavity. First, the gestational sac is located. This structure protrudes like a ball into the uterine cavity, and as the endoscope makes contact, it pushes off to the side. Light blue patches of chorion stud the otherwise white decidua capsularis (Fig. 21.3). Once the gestational sac is identified, the surface is gently scanned seeking an amniotic window. The latter can be seen in 70% to 80% of cases. The hysteroscope is placed onto this space; then, with a gentle side-to-side motion the window can be enlarged to accommodate the full 6- to 8-mm diameter of the endoscope (Fig. 21.4). If the observer’s movement is too rough, bleeding will be initiated and vision will be difficult; in virtually every case, this problem can be avoided. The embryo appears stark white as it comes into view against the dark background of the amniotic fluid. Since the chorioamnionic sac is intact and the light is absolutely cold, the natural activities of the embryo can be accurately assessed.
Hysteroscopic examination at early phases of development indicates that the embryo is actively moving. Precise observations of anatomic development and differentiation have been recorded. Gentle pressure of the endoscope on the amniotic window frequently can initiate movement. Because the embryo is so small and visualization occurs from the contact point to a distance of 5 mm, the view in this circumstance is magnified and panoramic.
At 4 weeks of development, bulbous eminences dominate the head of the conceptus. Initially, these structures were considered to be pathologic cysts, but are now recognized as normal landmarks (Fig. 21.5). Fusion of these structures starts at 5 to 6 weeks of development and is evidenced by the presence of cranial ridges, which subsequently leads to formation of the skull (Figs. 21.6 and 21.7). These ridges are well developed by 7 weeks. At 4 to 5 weeks, the first branchial cleft is another prominent visual structure (Figs. 21.8 and 21.9). By 7 to 8 weeks this closes to form the ear. Because no eyelids are present, the blue-black eyes are clearly visible and a retinal-type reflex may be seen in photographs but rarely during direct examination (Figs. 21.10, 21.11, 21.12).
Because the integument is very thin and virtually transparent, it has been possible to observe the pumping heart at approximately 4 weeks. The heart during this stage of development occupies most of the chest cavity and appears cherry red. The thorax virtually fuses with the abdomen where the umbilicus enters the latter (Figs. 21.13, 21.14, 21.15, 21.16).
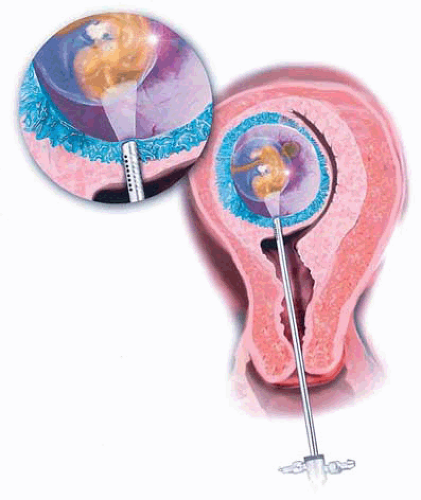 FIGURE 21.1 The hysteroscope makes contact with the embryonic sac. A window in the chorion is located, and direct contact with the amnion is made. |
During this embryonic period, the intestine naturally prolapses into the proximal cord, but does not represent an omphalocele (Figs. 21.17 and 21.18). Interestingly, bright-red blood can be seen spiraling through the umbilical arteries. The upper extremities appear initially as paddlelike structures, but, by 7 to 8 weeks, differentiate into unwebbed hands with distinct finger pads and nail beds (Figs. 21.19, 21.20, 21.21, 21.22). In contrast, the inferior extremities lag behind the upper limbs by 2 weeks and remain flipperlike appendages at 8 weeks. At 8 weeks the external genitalia are indifferent, and the most prominent feature seen is the phallus. The labioscrotal folds may be observed beneath the phallus in various states of fusion (Figs. 21.23, 21.24, 21.25).
The technique of embryoscopy does allow complete scanning of the embryo and can be a valuable tool for genetic counseling. Barbot in France has followed four women to term after performing embryoscopic examination to rule out structural abnormalities in the conceptus. Out of 110 examinations done at Mt. Sinai Hospital, Hartford, Connecticut, two patients have had delayed termination of pregnancy at 2 and 3 weeks after endoscopic study. Neither woman showed signs of threatened abortion in the interval between the endoscopic study and the eventual abortion. Although most of these examinations have been performed in women undergoing pregnancy termination, it has been consistently observed that the cervix promptly closes after withdrawal of the endoscope (Fig. 21.26).
Incomplete Abortion
Contact hysteroscopy is a feasible and safe method by which to examine the intrauterine milieu in the presence of products of conception, blood, and fluid (Figs. 21.27 and 21.28). Because the cavity is not distended by the endoscope, the hazard of pushing infected debris into the tubes or peritoneal cavity is eliminated. However, the differential diagnosis between incomplete abortion and other causes of uterine bleeding may be difficult; considerations should include threatened abortion, ectopic pregnancy, dysfunctional
bleeding, and uterine neoplasia. The question about when and if to perform curettage must be answered. Although dilatation and curettage is the most frequently performed operation in obstetrics and gynecology, it should not be construed to be free of complications. In particular, those problems related to future fertility (e.g., uterine synechiae, incompetent cervix, and perforation) are especially worrisome. Contact endoscopy gives a precise diagnosis in suspected cases of incomplete abortion.
bleeding, and uterine neoplasia. The question about when and if to perform curettage must be answered. Although dilatation and curettage is the most frequently performed operation in obstetrics and gynecology, it should not be construed to be free of complications. In particular, those problems related to future fertility (e.g., uterine synechiae, incompetent cervix, and perforation) are especially worrisome. Contact endoscopy gives a precise diagnosis in suspected cases of incomplete abortion.
Contact hysteroscopy may be carried out in an emergency room or private office using a 6-mm hysteroscope without the need of cervical dilatation. The appearance of fresh conceptual products is diagnostic: Chorion is slate blue; decidua is white but sprinkled with large, scarlet vessels; the placenta is deep reddish-brown (Fig. 21.29). No intact gestational sac (as in embryoscopy) is seen. In circumstances of ectopic pregnancy, the blue chorionic tissue is absent. Placental polyps lose their reddish hue and degenerate to a whitish color; the blue chorionic tissue also turns green. The polypoid structure of the tissue and the color changes described permit accurate diagnosis and direct the operator to the site of pathologic consideration. Barbot et al. in France avoid curettage unless bleeding is heavy. Weekly contact hysteroscopy is performed on an ambulatory basis (Fig. 21.30A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree