Chapter 6 Electrosurgery in Therapeutic Endoscopy
Introduction
Endoscopic electrosurgery involves the use of electrical current to achieve a desired tissue effect (cutting, tissue ablation, desiccation, or a combination of these). Electrical energy to produce heating and tissue effect has been a part of endoscopy since the early 1970s.1,2 Common indications include biliary sphincterotomy, polypectomy, hemostasis and ablation of vascular lesions such as arteriovenous malformations, radiation proctopathy, and other forms of vascular ectasia. Other forms of nonelectrosurgical thermal effect may be achieved without the direct use of electrical current, such as laser photoablation and heater probe. Incorrect use of electrical equipment may contribute to poor patient outcomes, such as postpolypectomy serositis; colonic perforation; and biliary sphincterotomy–associated complications such as acute pancreatitis, hemorrhage, and duodenal perforation.
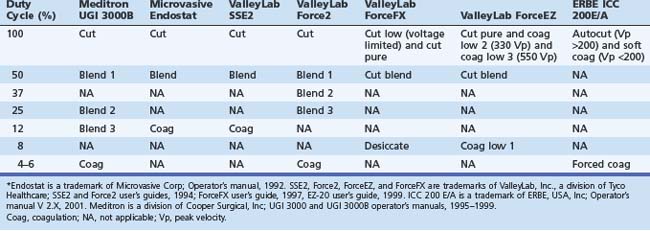
From the clinician’s point of view, this field has been hampered by problems with nomenclature (Table 6.1). First, there is often lack of uniformity in terms used by different manufacturers (e.g., blend may have quite different characteristics from one manufacturer’s generator to another). Second, the terms themselves may be misleading (e.g., a low duty-cycle waveform may be called pure coag but be capable of cutting tissue; this situation leads to statements such as “I only cut with coag”) Lastly, some terms in common usage are manufacturer specific (e.g., Endocut refers specifically to an ERBE [Marietta, GA] generator output). Usually a clinician becomes adept with the particular generator that he or she uses, and most modern generators have storable or preset parameters for common scenarios such as polypectomy and sphincterotomy. Problems may occur, however, when the clinician is confronted with a different generator (most likely to happen in an unusual and stressful environment, such as an emergency procedure in the operating room or emergency department or first list at a new appointment).
Electricity and Tissue
Early pioneers of electrosurgical devices discovered that applying an electrical current to biologic tissue might produce different effects. The first effect was electrolytic. Charged molecules in the tissue flowed toward the opposite poles of an electrode if the current applied was direct or alternated slowly. Alternating the current more rapidly eliminated the electrolytic effect and produced heating at a cellular level. However, a current alternating at less than 100 kHz resulted in undesired neuromuscular effects (the result of applying household current of 60 Hz is well known). Alternating at very high frequency (300 kHz) eliminates neuromuscular effects but retains the desired cellular heating effects. This thermal effect is the basis for all electrosurgery.3
Endoscopic Thermal Modalities
Bipolar (Multipolar) Electrosurgery
Bipolar (multipolar) electrosurgery uses technology similar to the monopolar circuit, but both electrodes are on the tip of the instrument. Current flows through a relatively small area of tissue, and there is no need for a return electrode on the patient’s skin. The common uses for this technology are coagulation of arteriovenous malformations and ulcer hemostasis. Bipolar (or multipolar) probes have been shown to be effective devices for hemostasis for bleeding peptic ulcers. Optimal results seem to be obtained by using forceful tamponade, large probes, low power settings (15 to 25 W) and prolonged contact times (10 seconds).4,5 This technique uses relatively low power outputs (approximately 16 W) with limited depth of injury.6 Bipolar snares, biopsy forceps, and sphincterotomes have been developed but are not widely used. A new, important use of bipolar current is radiofrequency ablation catheters employed to ablate Barrett’s esophagus. In this situation, the current moves from one adjacent electrode on a balloon catheter to another. This energy passes via the mucosa and is sufficient to obliterate the mucosa, while being superficial enough to prevent significant submucosal damage, minimizing stricture formation.
Argon Plasma Coagulation
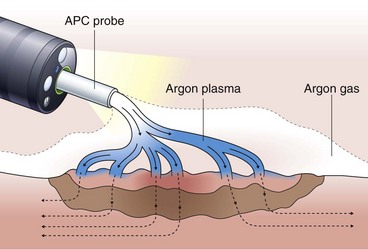
Argon plasma coagulation (APC) is a newer technique in flexible endoscopy with many potential applications, including tumor debulking,7 ablation of vascular malformations,8 and coagulation of peptic ulcer bleeding sites.9 It also has a role in “tidying up” residual adenoma after piecemeal polypectomy, although overuse in this setting suggests poor polypectomy technique. APC is a unique means of energy delivery (Fig. 6.1). Argon gas flows from the catheter tip and provides a medium for current flow from the catheter tip to an adjacent mucosal surface (and via the patient to a remote return pad). APC is a form of monopolar electrocoagulation, unique in its noncontact nature. It can be used effectively either tangential or perpendicular to the mucosal surface. Side-firing catheters are available, but the standard end-firing catheter can be used for tangential and perpendicular applications.
High current density at the mucosal surface leads to tissue effect. At high power output (e.g., 75 to 90 W), APC results in tissue debulking. At lower energy levels (e.g., 30 to 45 W), tissue desiccates with limited depth of injury.10 It has been theorized that as tissue desiccates, its electrical resistance increases, resulting in electrical arcing to adjacent, nondesiccated tissue. This mechanism could act to limit depth of injury. It has been shown, however, that APC can cause transmural injury at high power outputs,10 and there have been reports of perforation using this device.11,12 Nonetheless, the relative ease of use, nontouch technique, and relatively shallow depth of injury make this a versatile and useful instrument, especially in thin parts of the bowel such as small intestine and right colon.
Heater Probe
The heater probe unit (Olympus Corporation, Melville, NY) comprises a power source, catheter, and irrigation system. At the tip of the catheter is a heating coil within a polytef (Teflon) cap. This energy delivery is unique because it supplies a predetermined amount of energy (e.g., 30 J) to the cap without an electrical circuit flowing through tissue. Because this is a direct transfer of heat, it is an example of electrocautery, not electrosurgery. The main indications are ulcer hemostasis and coagulation of angiodysplastic lesions. Heater probe results in ulcer hemostasis in 80% to 90% of bleeding lesions.13 The energy and probe size are inadequate for tumor ablation indications, and this method cannot produce any electrosurgical cutting effect.
Principles of Electrosurgery
Tissue effect is determined by the rapidity of tissue heating. Rapid heating causes intracellular boiling and explosion of cells resulting in a cleavage plane (incision).14 In contrast, slow heating results in protein denaturization and desiccation or “coagulation” of tissue.15 Understanding the different characteristics of tissue heating under different circumstances is essential to understanding electrosurgery.
Variables in Electrosurgery
Many variables in electrosurgery can influence tissue effect.
Power Output
Two formulas, including Ohm’s law, elegantly relate all of the electrosurgical variables:
Power and voltage are also directly related (e.g., P = V2/I).
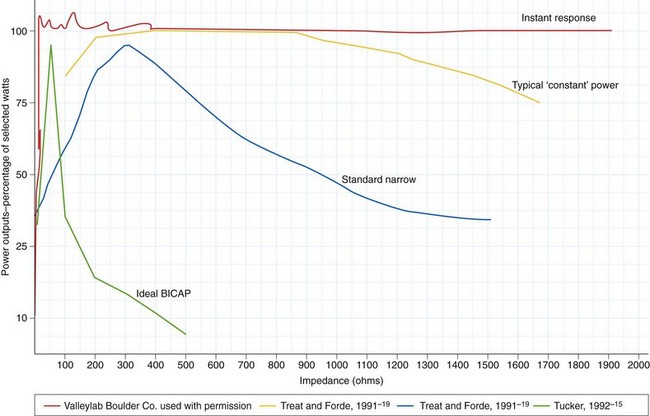
These formulas illustrate that there is a relationship between power output and tissue resistance. As the resistance (or impedance) in the tissue increases (as it desiccates), power falls off unless either current or voltage is increased. Manufacturers addressed this problem by developing microprocessor-controlled generators that could measure resistance in the circuit and adjust output automatically (within certain set parameters) to maintain the desired tissue effect.16 Some power outputs are constant over a wide range of resistance; when this is graphically represented, it results in the so-called flat or wide power curve (Fig. 6.2). The initiation of an incision is problematic for generators, especially if the electrode is pressed firmly against the tissue surface because this presents a large surface area with low current density and low tissue impedance. The generator must supply particularly high power output to initiate the formation of microelectric arcs and commencement of the cutting effect. This initial power output is often greater than the output needed to continue the incision. Microprocessors can recognize this situation and transiently provide a high power output to initiate cutting.