Chapter 15 Obscure Gastrointestinal Bleeding
Introduction
Obscure gastrointestinal (GI) bleeding accounts for approximately 5% of all GI bleeding and is defined as bleeding from an unknown source that persists or recurs after negative endoscopic diagnostic evaluation.1 A negative diagnostic evaluation is commonly agreed on as consisting of negative upper endoscopy (esophagogastroduodenoscopy [EGD]) and colonoscopy with careful evaluation of the terminal ileum. Obscure GI bleeding is subcategorized as overt or occult. Obscure-overt GI bleeding is persistent or recurrent visible evidence of bleeding (hematemesis, hematochezia, or melena), whereas obscure-occult GI bleeding is persistent or recurrent positive fecal occult blood, iron deficiency anemia, or both, when there is no evidence of visible blood loss to the patient or health care provider.2
Etiology of Obscure Gastrointestinal Bleeding
Obscure GI bleeding has numerous possible causes and may originate from the upper GI tract (proximal to the ligament of Treitz), the mid-GI tract (ligament of Treitz to the terminal ileum), or the colon. Most causes (approximately 75%) of obscure GI bleeding are found between the ligament of Treitz and the ileocecal valve—in other words, in the small bowel.3 Arteriovenous malformations (AVMs) of the small bowel account for 30% to 40% of obscure GI bleeding and are the most common source of obscure GI bleeding in older patients (Fig. 15.1).4 In persons 30 to 50 years of age, tumors such as GI stromal tumors, leiomyomas, leiomyosarcomas, schwannomas, carcinoids, lymphomas, and adenocarcinomas predominate (Fig. 15.2). Younger individuals most commonly have obscure bleeding from Crohn’s disease or Meckel’s diverticula–associated ulceration (Fig. 15.3).5 Nonsteroidal antiinflammatory drug (NSAID) enteropathy has been associated with erosions, ulcers, and strictures of the small bowel and can also be a potential cause of obscure GI bleeding.6 Less common causes of obscure GI bleeding include Dieulafoy’s lesions, hemosuccus pancreaticus, Strongyloides stercoralis infection, radiation-induced enteritis, and pseudoxanthoma elasticum (Table 15.1).7–11

Fig. 15.2 Gastrointestinal stromal tumor as seen by double-balloon enteroscopy.
(Courtesy of Professor Roberto De Franchis.)
Table 15.1 Etiology of Obscure Gastrointestinal (GI) Bleeding
| UPPER GI LESIONS |
| MID–GI TRACT LESIONS |
| Younger than 40 Years of Age |
| Older than 40 Years of Age |
| LOWER GI LESIONS |
NSAID, Nonsteroidal antiinflammatory drug.
Investigating Obscure Gastrointestinal Bleeding
A review of medications (including over-the-counter medications) may reveal inadvertent use of NSAIDs or products containing acetylsalicylic acid (ASA) and NSAIDs. A family history of cancer occurring at an early age, particularly colorectal or endometrial, may suggest the presence of hereditary nonpolyposis colorectal cancer. Skin, nail, and oral mucosal changes may suggest the presence of several disorders associated with obscure GI bleeding or iron deficiency anemia, including telangiectasias, which may reflect hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome); dermatitis herpetiformis, which may reflect celiac disease; or other conditions with cutaneous and GI manifestations (e.g., Kaposi’s sarcoma, Peutz-Jeghers syndrome, tylosis, pseudoxanthoma elasticum, Ehlers-Danlos syndrome, blue rubber bleb nevus syndrome, Henoch-Schönlein purpura, neurofibromatosis, malignant atrophic papulosis, and Klippel-Trenaunay-Weber syndrome).2
Diagnostic Investigations
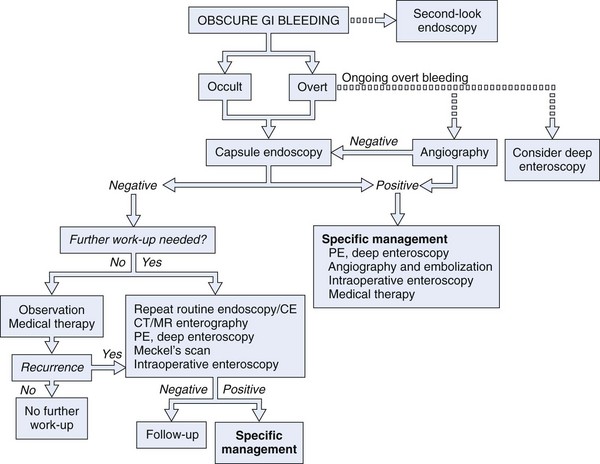
Numerous diagnostic investigations may be performed to identify the etiology of obscure GI bleeding. Endoscopic investigations include repeat EGD and colonoscopy, push enteroscopy, capsule endoscopy (CE), deep enteroscopy using balloon-assisted or non–balloon-assisted techniques, and intraoperative enteroscopy (IOE). Radiologic testing includes barium studies such as small bowel follow-through and enteroclysis, nuclear medicine studies such as tagged red blood cell (RBC) scan and Meckel’s scan, computed tomography (CT) and magnetic resonance (MR) imaging in combination with enteroclysis (CT and MR enterography), and angiography (Fig. 15.4).
Endoscopic Investigations
Repeat Upper Endoscopy (Esophagogastroduodenoscopy) and Colonoscopy
Second-look upper endoscopy may be helpful in identifying lesions potentially overlooked or unrecognized at the time of the initial endoscopic evaluation.12 Data suggest that 20% of lesions leading to obscure GI bleeding may be overlooked and are within reach of a standard upper endoscope.13 Commonly overlooked lesions in the upper GI tract include Cameron’s erosions or ulcerations in large hiatal hernias, isolated gastric fundal varices, peptic ulcers, AVMs including gastric antral vascular ectasia (watermelon stomach), and Dieulafoy’s lesion (Fig. 15.5).14–16 An aortoenteric fistula should be considered in patients with prior abdominal aortic aneurysm repair. Although the reported yield of repeat colonoscopy is low (3% to 6%), it may be helpful in selected patients when the original colonoscopy examination was documented to have had a mediocre or poor preparation, the extent of the examination was not to the cecum, or the terminal ileum was not evaluated.17 Lesions missed or unrecognized during colonoscopy may include AVMs, polyps, solitary rectal ulcers, rectal varices, and neoplasms.
Push Enteroscopy
Push enteroscopy permits evaluation of the proximal small intestine to a distance that is approximately 50 to 100 cm beyond the ligament of Treitz. Dedicated videoenteroscopes (160 to 250 cm in length) are commercially available, but if these instruments are not available at the endoscopy site, a pediatric or standard adult colonoscope can be used instead.18 The use of an overtube, back-loaded onto the endoscope insertion tube, may help limit looping of the enteroscope within the stomach and facilitate deeper small bowel intubation.19 The diagnostic yield of push enteroscopy is reported to increase with greater depth of scope insertion. When using a pediatric or adult colonoscope, the reported diagnostic yield in the evaluation of obscure GI bleeding ranges from 13% to 38%. With the use of a dedicated videoenteroscope, reported diagnostic yield rates increase to 26% to 80%.13,20,21
With the development of endoscopic devices for dedicated videoenteroscopes, such as biopsy forceps, snares, thermal probes (contact and noncontact), and injection needles, push enteroscopy is preferred over radiologic diagnostic modalities because of the ability to obtain tissue, perform polypectomy or hemostasis if necessary, and mark lesion sites with India ink tattoo.13 However, push enteroscopy does not allow for the visualization of the entire small bowel, and complications, including perforation and mucosal laceration, have been reported with the use of an overtube. With the advent of CE and “deep” enteroscopy, diagnostic push enteroscopy is less commonly used.
Capsule Endoscopy
CE is an endoscopic technology that is capable of obtaining endoscopic images from the entire small bowel.22,23 CE is safe, easy, minimally invasive, and patient-friendly and has become a first-line tool in imaging small bowel pathologies. With this realization, there has been rapid uptake and wide acceptance of this revolutionary endoscopic technology for detecting small bowel abnormalities.24
The Pillcam SB video capsule endoscope (Given Imaging Ltd, Yoqneam, Israel) is a wireless capsule (11 mm × 26 mm) composed of a light source, lens, complementary metal oxide semiconductor imager, battery, and wireless transmitter. The Pillcam SB has a battery life of approximately 7 to 8 hours in which time the capsule captures two images per second (approximately 60,000 total images per examination) in a 140-degree field of view and 8 : 1 magnification.25 The smooth outer coating of the capsule allows easy ingestion and prevents adhesion of intestinal contents, whereas the capsule moves via natural peristalsis from the mouth to the anus. Endoscopic images are transmitted via sensor arrays to a recording device worn as a belt by the patient. The recorded images are downloaded into a Reporting and Processing of Images and Data (RAPID) computer workstation and reviewed as a continuous video by the physician. The PillCam SB 2 video capsule offers advanced optics and a wider field of view for imaging the small bowel. It has the same dimensions as the PillCam SB and captures nearly twice the mucosal area per image compared with the PillCam SB. The PillCam SB 2 also provides Automatic Light Control for optimal illumination of each image.
Olympus (Olympus Corporation, Tokyo, Japan) has introduced a wireless capsule endoscope (EndoCapsule) with similar features. The Pillcam SB, Pillcam SB 2, and EndoCapsule have been approved by the U.S. Food and Drug Administration (FDA) (Fig. 15.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree