Chapter 44 Benign Biliary Strictures and Leaks
Introduction
Accidental injuries of the bile ducts leading to biliary leaks and strictures may occur during any surgical procedure involving the biliary tract. However, the main cause of injury of the bile ducts at the present time is laparoscopic cholecystectomy (LC). Although LC has proved to be superior to open cholecystectomy in terms of shorter hospitalization, lower overall morbidity, faster recovery, and better cosmetic outcome, the risk of bile duct injury during LC is two to six times greater compared with open cholecystectomy.1,2 Bergman and colleagues3 described four types of postoperative bile duct injuries, as follows:
Epidemiology
LC was first performed by Mouret in France in 1987. The technique was standardized by two other French surgeons, Dubois in Paris and Perissat in Bordeaux.4,5 This new technique spread very rapidly around the world; in the United States, the percentage of cholecystectomies done laparoscopically grew from zero in 1987 to almost 80% in 1992.6 The advent of LC also induced an estimated increase of at least 25% in the overall number of cholecystectomies performed,7,8 so that the likely number of cholecystectomies performed at the present time in the United States is 800,000 per year.9 The number of iatrogenic injuries to the bile duct has increased accordingly.10
Many reasons may explain the increased incidence of biliary complications at the beginning of the laparoscopic era, most related to the new technical skills required to perform laparoscopically what had been done by open surgery: bidimensional vision, loss of tactile sensations, different visual approach of the hepatic pedicle, difficult hemostatic maneuvers, abuse of electrocoagulation, and lack of confidence with the new instrumentation.11 The rate of injuries seemed to be related to the surgeon’s learning curve and his or her personal experience. An inversely proportional relationship between the number of cholecystectomies performed and the rate of injuries was suggested by earlier reported series.1,12 In a review of 77,604 LCs performed in the United States, the incidence of biliary injuries decreased from 0.6% to 0.4% (P < .001) for surgical teams having an experience of more than 100 LCs.1 A Belgian survey11 suggested the number of 50 LCs as the threshold of a completed learning curve; however, the same authors emphasized that one-third of the biliary injuries in their country had occurred with surgeons with an experience of more than 100 LCs. When reviewing several multicenter series published before 1995, totaling 198,267 LCs, the incidence of biliary injuries was 0.55% in 13 European series and 0.49% in 17 series outside Europe.13
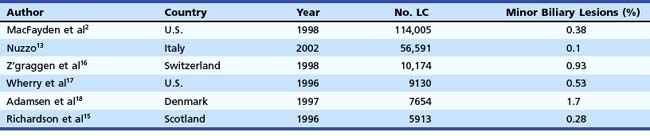
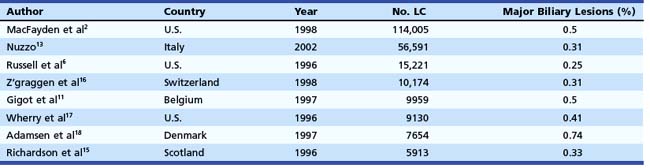
In the mid-1990s, the incidence of biliary injury seemed to be three times higher for LC than for open cholecystectomy. However, these figures most likely underestimated reality because there was a tendency not to declare all the lesions, as revealed by the low rate of reply to most surveys and by the increasing number of reported lesions in direct proportion with the collected replies.14 At the present time, the incidence of biliary injuries has not substantially changed, even if a trend toward reduction has been reported by some authors.6,15 The estimated overall incidence is 0.25% to 0.74% for major biliary lesions (Table 44.1) and 0.1% to 1.7% for minor biliary lesions (Table 44.2).16–18 These figures are only partially explained by the still increasing number of LCs performed around the world and by the activity of young surgeons at the beginning of their learning curve. However, at least one-third of biliary injuries may be ascribed to technical mistakes during surgery.19 The learning curve is not the only risk factor of LC.
Table 44.1 Incidence of Major Biliary Lesions (Bergman’s Type B, C, and D) during Laparoscopic Cholecystectomy (LC) (Multicenter Surveys)
Pathogenesis
Unrecognized CBD stones are one of the major risk factors of cystic duct leakage after LC. The mechanism and the cause of a biliary injury remain unexplainable in at least one-third of cases.13 In more than 50% of cases, the injury occurs during the dissection of the cystic duct or during separation of the gallbladder neck from the CBD. Misinterpretation of the cystic duct and the CBD is the most common cause of injury.12 Excessive traction on the gallbladder neck, especially if the tissues are not inflamed, may facilitate the injury of the CBD. Conversely, when the area is acutely or chronically inflamed or when a stone is trapped into the gallbladder infundibulum, the risk of CBD injury is higher during the dissection of the gallbladder neck from the hepatic pedicle. Other recurrent reasons for bile duct injury are related to incorrect hemostatic maneuvers in case of bleeding from the cystic artery; inappropriate use of electrocautery; and other specific maneuvers, such as intraoperative cholangiography, cystic duct dilation, and transcystic CBD instrumental exploration.
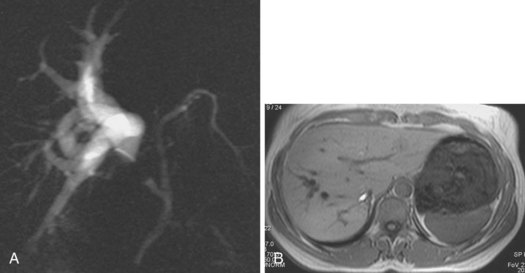
An anatomic anomaly is often reported by the surgeon as having caused a biliary injury. Variations of the biliary anatomy, especially at the level of the main hepatic confluence, are present in 50% of patients (see the section on interpretation of intrahepatic cholangiography). Surgeons must be aware of such variations and must keep in mind the danger of injuring aberrant ducts originating in the right liver during dissection of the gallbladder pedicle. Aberrant ducts must not be interpreted as accessory ducts because the biliary distribution within the liver parenchyma is of a terminal type; this implies that there are no intrahepatic anastomoses between the ducts and that every injury of an aberrant duct would determine functional exclusion of the corresponding liver area. Injury to a small aberrant duct may still be considered a minor lesion; however, it would cause a bile leak into the peritoneal space with all the related consequences. Another cause of injury is clipping or ligation of an aberrant duct. This injury does not involve a bile leak but entails the functional exclusion of the corresponding liver area leading to its progressive atrophy and hypertrophy of the remaining liver parenchyma. This possible event may be clinically totally asymptomatic and noted only by an increase in biochemical parameters of cholestasis and cytolysis (Fig. 44.1). Although there is no indication of treatment in asymptomatic cases, if the obstructed ducts become infected, recurrent cholangitis is the typical clinical manifestation often requiring operative reestablishment of an adequate bile flow.
Treatment
Endoscopic Retrograde Cholangiopancreatography and Biliary Leak
The presence of a bile leak invariably indicates a break in the continuity of the biliary system. However, the severity of the injury (ranging from simple leakage of the cystic stump to complete transection of the bile duct) and the complexity of its repair are extremely variable. The magnitude of the bile output does not usually help in presuming the origin and the size of the leak. A direct cholangiogram is of utmost importance for accurate anatomic depiction and to classify the type of injury to plan therapy. The usefulness of magnetic resonance cholangiopancreatography (MRCP) in the delineation of postoperative biliary leaks20 and of iatrogenic strictures21 has been reported. However, in contrast to ERCP, MRCP has no therapeutic capability. MRCP may be recommended in anatomic situations in which the endoscopic approach is presumably difficult or occasionally impossible, such as in patients with a Billroth II anatomy and with Roux-en-Y hepaticojejunostomy.
In case of external biliary fistula through an abdominal drain, it is not advisable to start the procedure by injecting contrast medium through the drain (fistulography). In most instances, especially in minor lesions, the contrast medium freely flows into the peritoneal space without depicting the biliary tree. The presence of contrast medium overlapping the area involved by the lesion may hinder the correct interpretation of subsequent cholangiography and occasionally disguise the picture entirely. In contrast, fistulography is indicated whenever endoscopic cholangiography shows an incomplete filling of the biliary system resulting from a complete transection of the main bile duct or lack of visualization of a sectorial or segmental intrahepatic branch. As an alternative to contrast medium, which occasionally might not fill the missing branch, air may be used to obtain a pneumocholangiogram.22
The technique of ERCP in the setting of a suspected biliary injury does not substantially differ from the routine examination. Special attention should be paid to the injection of contrast medium, however, which should be slow and careful to allow precise delineation of the lesions. Massive injection of the biliary tree should be avoided. Minimal injection and early filling x-ray films are also important in detecting small residual CBD stones, which are present in 20% of patients with biliary leakage originating from the cystic duct stump. If the suspected lesion is located in an intrahepatic biliary branch, it is of paramount importance to obtain a complete intrahepatic cholangiogram; to achieve an adequate pressure of injection, especially if a sphincterotomy has been previously performed, the use of an occlusion balloon catheter is advisable. Intrahepatic biliary anatomy is better shown by multiple x-ray films taken in different projections. Percutaneous transhepatic cholangiography and MRCP should be reserved for patients in whom ERCP fails technically or fails to show the intrahepatic biliary anatomy because of proximal ductal disruption.23
Interpretation of Intrahepatic Cholangiography
The main biliary confluence is formed by the union of the right and left hepatic ducts that drain the bile originating in the right hemiliver and the left hemiliver. The main confluence is often incorrectly called bifurcation in the English literature; actually, although the portal vein and the hepatic artery carrying the blood to the liver have bifurcations, the fusion of ducts collecting the bile from the liver with a flow directed toward the CBD generates a confluence. According to the segmental liver anatomy described by Couinaud,24 the left hepatic duct collects the bile originating from segments II and III (left anatomic liver lobe or left lateral sector) and from segment IV (quadrate lobe). One or more small ducts originating from segment I (caudate lobe) also join the left hepatic duct close to the main confluence. The anatomic variations occurring in the left hepatic system are rare and are irrelevant in this perspective. The right hepatic duct is shorter than the left hepatic duct and follows the same axis of the common hepatic duct. The right hepatic duct originates from the confluence of the right anteromedial sectorial duct (segments V and VIII) and of the right posterolateral sectorial duct (segments VI and VII). The right anteromedial duct is recognizable thanks to its orientation, which follows the same axis of the right hepatic duct, whereas the right posterolateral duct joins the right anteromedial duct on its medial aspect with a typical umbrella handle–like shape.
This normal anatomy (called “modal” by Couinaud) is present in approximately 60% of the population (Fig. 44.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree