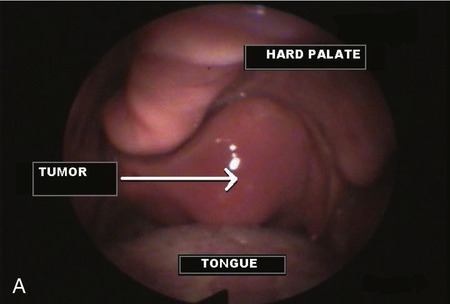
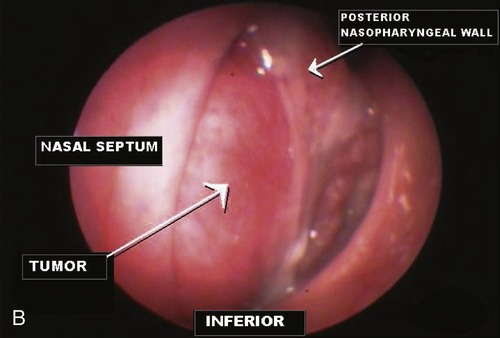
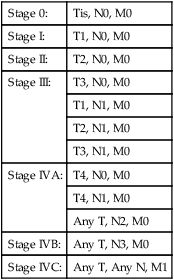
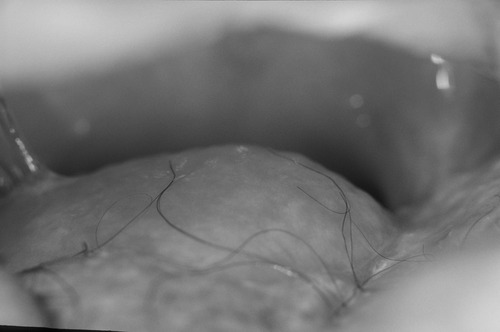
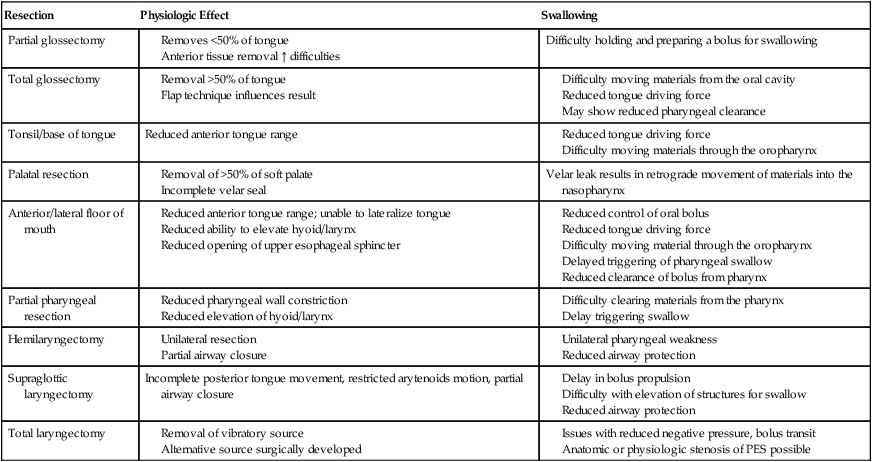
1. Define cancer and describe its potential impact on the individual patient. 2. Describe the various treatments for head/neck cancer and their side effects. 3. Describe factors that contribute to dysphagia in patients being treated for head/neck cancer. 4. Describe the dysphagia characteristics that might be associated with head/neck cancer treated with different modalities. 5. Elaborate on dysphagia-related complications seen in patients treated for head/neck cancer. 6. Discuss the when, what, and why aspects of dysphagia intervention for patients being treated for head/neck cancer. What are the anticipated outcomes for the various dysphagia interventions? Cancer is the result of cell growth that is out of control. In simple terms, cells become abnormal and grow rapidly, forming extra, unwanted, and potentially destructive tissue. This proliferation of cell growth is called hyperplasia. The abnormality that causes cancer cells results from damaged DNA within cells. This damaged DNA may be inherited or it may result from exposure to an environmental cause such as smoking. In fact, the primary risk factors for head and neck cancer (with the exception of nasopharyngeal cancer) have been identified as tobacco (including smokeless tobacco), heavy alcohol use, poor oral hygiene, and mechanical irritation.1 One potential problem caused by these abnormal cancer cells is that they can travel to various places in the body, begin to grow and proliferate, and replace normal body cells. This traveling of cells is referred to as metastasis. Metastasis may occur when cancer cells enter the bloodstream or the lymph system and travel to a different part of the body. Cancer usually forms as a tumor, which technically means a swelling or enlargement, although not all cancers form tumors and not all tumors are cancerous. Some tumors are benign rather than malignant. Different types of cancers grow at different rates, create different problems, and respond to different treatments. One way to conceptualize cancer is as a group of diseases with different symptoms and signs. Symptoms are noticed by a patient and taken as an indication that something is not right in the body. Signs are also indicative of health problems but are more definitive of disease as observed by a physician or other health care professional. Symptoms and signs of cancer may change as the disease changes over time. The specific symptoms and signs depend on the location of the cancer; the size of the tumor; direct impact on any surrounding organs, blood vessels, or nerves; and any metastasis of the cancer. Both general and specific symptoms have been associated as warning signs of cancer. These are summarized in Box 6-1. Different problems may be encountered depending on the type and location of a cancer. The symptoms listed in Box 6-1 provide general categories of problems that may be encountered. Pain is perhaps the most feared of cancer-related problems. Pain does not result from all cancers, but when it does occur it may be the result of tumor growth or result from the treatments used to eradicate the cancer. Another common problem is fatigue. Like pain, fatigue may result either directly from the cancer or as a side effect of cancer treatment. Box 6-2 summarizes some of the salient characteristics that may be associated with cancer-related fatigue. Cancers may also contribute to significant weight loss and impaired immune function. These problems are not mutually exclusive because malnutrition also contributes to impaired immune function. Impaired immune function contributes to increased complications, poor wound healing, and opportunistic infections. Together, poor nutrition and impaired immune function may contribute to a less-optimistic outcome for patients with cancer. An estimated 30% to 50% of patients with head/neck cancer demonstrate some degree of malnutrition.2 Up to half of patients with head/neck cancer reveal some degree of weight loss when cancer is first diagnosed.3,4 Average weight loss has been estimated between 5% and 10% of baseline body weight.4,5 Weight loss may result from reduced ingestion or digestion of food and/or impaired absorption or utilization of nutrients by the body in the presence of adequate food and liquid intake. This latter situation may be complicated by the need for increased caloric intake resulting from increased energy expenditure in some patients with cancer. Thus some patients have a biologic need for more caloric intake, but as a result of poor food and liquid intake, absorption, or utilization they actually have a significantly reduced caloric reservoir. This can become a vicious cycle leading to cachexia. Weight loss may be accompanied by anorexia, nausea and/or constipation, and fatigue. Box 6-3 summarizes some of the more general consequences of malnutrition in patients with head/neck cancer. A common procedure involved in evaluating cancer is staging. In simple terms, staging is the process of determining how far the cancer has spread. This process is important in determining the best treatment options, estimating complications or comorbid conditions, and formulating a prognosis. Although more than one system is available for cancer staging, the TNM system is used most often.6 T (tumor) describes the size of the tumor and extension into any neighboring tissues. N (nodes) describes any spread of the cancer into nearby lymph nodes. M (metastasis) describes spread of the cancer to other organ systems within the body. A number or additional letter after each letter is assigned to provide more detail. In general, lower numbers mean smaller, more localized cancers. Higher numbers mean larger, spreading cancers. Therefore a T1N0M0 tumor is small, has not invaded neighboring lymph nodes, and has not spread to other body organ systems. Conversely, a T4N2M1 tumor is large, has invaded neighboring lymph nodes, and has metastasized to other body organ systems. Box 6-4 lists TNM definitions for oropharyngeal cancer. Similar, but not identical, definitions are used for hypopharyngeal and laryngeal cancers. One difference is the inclusion of anatomic subsites for these latter areas. After TNM description, cancers may be grouped together into stage classifications. In general, five stages are used (stage 0 through 4). Stage 4 has three subdivisions (A, B, and C). A lower stage classification indicates a smaller, nonmetastasized cancer. A higher stage classification indicates a more serious, widespread cancer. Box 6-5 shows the staging system based on TNM descriptions. Many cancers of the head/neck region can be cured if they are found early. Choice of treatment and outcome frequently depend on many factors, including location and stage of the cancer, the patient’s age and general health status, the experience of the medical team treating the patient, and available facilities. Although curing the cancer is a primary goal, the patient’s posttreatment function and quality of life are also important considerations in choosing the type of treatment because each treatment has potential side effects and sequelae. Another aspect to consider is whether the treatment is intended to be palliative or curative. Three primary options are frequently used in the treatment of head/neck cancers: surgery, radiation, and chemotherapy. These may be used in isolation or in various combinations depending on the type of cancer and the goals of treatment. Surgery and radiation therapy are considered the only curative therapies for cancer in the head/neck region. Chemotherapy is used in the neoadjuvant or adjuvant setting but is not considered a curative therapy.7 Surgery refers to removal of the cancerous tumor and some of the surrounding healthy tissue, referred to as the margin. Surgery is intended to remove as much of the primary tumor as possible and leave no trace of cancer cells in the margin. However, this is not always possible, and surgery often is combined with radiation therapy and/or chemotherapy. In some cases, more than a single surgery may be required to remove the cancer or restore the anatomic or functional deficit caused by the primary surgery. For example, if the cancer has spread to the lymph nodes in the neck, the lymph nodes will be removed. This is called a lymph node dissection or a neck dissection. In other situations reconstruction may be required. This involves moving tissue from another part of the body to fill a gap created by the cancer resection. A variety of procedures have been described to relocate tissue to the head/neck region. Generally referred to as flaps, these are often named for the location from which the replacement tissue is taken. Therefore a pectoralis major flap would be constructed from tissue obtained from the pectoralis major muscle. Other flaps might include a lateral thigh flap, a radial forearm flap, or similar procedures. Figure 6-2 depicts a pectoralis major flap on the left side. Figure 6-3 shows a flap reconstruction of the floor of the mouth and tongue. In some situations bone tissue may be relocated to reconstruct bony deficits in the mandible, or if a majority of the mandible is removed an implant may be used to replace the missing bone (Figure 6-4). If surgical reconstruction is not feasible, a prosthodontist may be consulted to construct artificial dental or facial parts to fill a space created by the initial surgery. If the primary tumor surgery creates a risk to breathing, a tracheotomy may be performed. If severe swallowing problems are anticipated, a gastrostomy may be performed. Either or both of these procedures may be performed at the time of the primary cancer surgery if the surgical team anticipates airway or swallowing problems as a direct result of the surgery. Surgery is a primary treatment consideration for all small cancers. Contraindications to surgical removal of a small tumor are the possibility of significant deficits to function (speaking, chewing, swallowing) or cosmetic defects. Advanced cancers often require a combination of surgery and/or radiation or chemotherapy. Various surgical approaches may be used depending on the location and size of the cancerous tumor. Box 6-6 lists some of the more common surgeries associated with head/neck cancer treatment. Surgery, like other cancer treatments, has a number of side effects that can be problematic for patients. Side effects typically depend on the location and type of surgery. Some of these are temporary and others are more permanent. All side effects have an impact on the patient’s quality of life. Box 6-7 lists some of the more frequent side effects from cancer surgery in the head/neck region. The length of time after surgery was performed is an indicator of the prominent side effects. For example, edema will be pronounced in the acute postoperative period. Edema may be accompanied by pain. As the primary surgical site heals, scarring may reduce movement of anatomic structures spared and in the vicinity of the surgery. In addition, if cranial nerves are damaged during the primary surgery or as a result of postoperative scarring, the patient may sustain motor or sensory deficits from nerve damage. Radiation therapy uses high-energy x-rays to kill cancer cells. Death of the cancer cells leads to shrinkage of the tumor. Radiation therapy may be used as the primary treatment for small tumors, after surgery to destroy residual small pockets of cancer cells, or before surgery to shrink tumors in the hope of more successful surgical removal with fewer residual deficits. Radiation may be administered in two ways: external-beam radiation and internal radiation. External-beam radiation involves aiming a high-energy radiation beam at the tumor and surrounding tissues. External-beam radiation may be applied on a conventional, once-daily schedule or on an altered fractionation schedule. The latter form of radiation therapy may increase acute toxicity, but late effects are similar between these two techniques.7 A newer form of external-beam radiation is known as intensity-modulated radiation therapy. This procedure allows more effective doses of radiation to be delivered to the tumor while hitting less healthy tissue around the tumor. This method is intended to result in fewer side effects. Other recent advances in radiotherapy include radiosensitization (using drugs to make cancer cells more sensitive to radiation) and hyperfractionation (giving radiation in small doses several times per day). In general, treatment strategies leading to a lower dose of radiotherapy or radiotherapy to more confined anatomic regions results in less-severe and more transient dysphagia.8–10 Side effects from radiation therapy are common both during treatment (acute toxicity) and after treatment (late effects or late toxicity). Some of these effects are transient and others are persistent. In addition, certain side effects may be latent—that is, they may not appear for a substantial period (in some cases years) after the completion of radiation therapy. Many side effects of radiation therapy to the head/neck region contribute directly to dysphagia and resulting decline in nutritional status. If these occur during treatment, patients may experience interruptions in therapy. Box 6-8 lists several side effects that may occur from radiation therapy to the head/neck region. Chemotherapy refers to the use of drugs to kill cancer cells. These agents are typically very powerful drugs that can cause several unpleasant side effects. Chemotherapy may be administered by mouth, intravenously, by injection into a muscle or under the skin, or by injection directly into the tumor. Chemotherapy may be used to palliate symptoms in patients with incurable disease or as an adjuvant to radiation therapy, surgery, or both. Chemotherapy may be used before or after surgery (and/or radiation therapy). Chemotherapy has been used in combination with radiation therapy to treat certain laryngeal cancers in an attempt to preserve the larynx (avoid a total laryngectomy) and subsequent voice functions. As previously mentioned, certain drugs may be used in combination with radiation therapy as a form of radiosensitization. Although these approaches are promising, many combined therapies are still considered experimental. One negative aspect of combined therapies is the risk of increased severity or a wider range of side effects. For example, large clinical studies reported increased acute toxicity in patients receiving concomitant chemoradiation therapy.11 However, at least one review has concluded that posttreatment swallowing dysfunctions noted in patients receiving concomitant chemoradiation therapy were similar to those seen in patients receiving only radiation therapy.12 Box 6-9 lists several possible side effects from chemotherapy in the treatment of head/neck cancer. Each patient should be evaluated for the presence of one or more of these possible side effects resulting from primary cancer treatments that may affect swallowing function. Many—in fact, a majority—of patients treated for head/neck cancer have some degree of swallowing difficulty. Some dysphagia symptoms result directly from the cancer and thus may be present before medical treatment, whereas others are the result of various treatments for the cancer. In general, patients receiving radiation therapy (alone or in combination with surgery) are at greater risk for swallowing difficulties than are patients receiving surgical treatments without radiation.13–15 Dysphagia subsequent to cancer treatments may be described as resulting from reduced swallowing efficiency, which may be complicated by anatomic changes within the swallow mechanism. Reduced swallow efficiency is characterized by reduced movement of structures within the swallowing mechanism, leading to prolonged duration of various aspects of the swallow and reduced opening of the pharyngoesophageal segment.16,17 The reduction of movement during swallowing contributes to post-swallow residue along the swallowing mechanism and poor clearance of saliva.12,18 Food and saliva residue may build up over time, increasing the risk of aspiration or necessitating frequent expectoration by the patient. Surgery for head/neck cancer results in the loss, rearrangement, or reconstruction of structures that are important for swallowing function. A traditional rule for predicting dysphagia after surgery for head/neck cancer is the “50% rule.”19,20 This “rule,” which seems to result from experiences with oral cancers, suggests that removal of less than 50% of a structure will not result in a significant and permanent swallowing problem. However, this rule has been challenged with the introduction of surgical reconstruction techniques as clinicians report good postoperative swallowing function after surgical flap reconstruction.21,22 Thus individual patient characteristics should be carefully examined both before and after surgery to identify and manage any resulting swallowing impairments.23 A general guideline is that the more tissue removed or relocated, the higher the probability for postsurgical dysphagia. Of course, this guideline requires modification when combined modalities are used (radiation therapy and/or chemotherapy in addition to surgery). The following text provides a brief overview of certain dysphagia characteristics that may result from surgery involving various aspects of the swallowing mechanism. Table 6-1 presents a summary of certain surgeries with the associated physiologic impact and anticipated swallow deficit. TABLE 6-1 Common Swallowing Disorders Resulting from Various Surgeries to Treat Head/Neck Cancer Generally speaking, the oral cavity involves the anterior aspect of the tongue, floor of the mouth, submental structures, the mandible, and the maxilla. Oral surgeries often involve more than a single structure. For example, a mandibulotomy may be required to gain adequate surgical access to tumors in the floor of the mouth or other areas of the oral cavity. In general, surgeries for oral cancers may limit mastication, bolus formulation and containment, and bolus transport from the front to the back of the mouth. Surgeries restricted to the tongue often result in transient dysphagia with good functional outcome; however, this may depend on the extent of the tissue removed and the shape of the reconstructed tongue if flap reconstruction is completed.24,25 When present, swallowing problems resulting from limited tongue resections involve bolus control and transport difficulties and may be transient. With more extensive resections involving the tongue and floor of mouth with or without flap reconstruction, dysphagia may be expected for varying periods. Such dysphagia typically involves problems with mastication, bolus control, transport to the posterior oral cavity and, in some cases, airway protection as a result of loss of control of the bolus within the oral cavity.26–28 In addition, pain may result from alterations to the temporomandibular joint. In cases of dramatic resection and reconstruction of the mandible, limitations in the pharyngoesophageal segment may result from reduced upward pull from the hyolaryngeal complex that attaches to the mandible. Conversely, some patients with resection limited to oral structures will have functional pharyngeal aspects in swallowing and will do well if compensations can be used for oral deficits. Video 6-1 on the Evolve site demonstrates functional pharyngeal aspects of swallowing in a patient with significant tongue reconstruction. Contrast liquid is delivered to the pharynx by a small straw connected to a syringe to compensate for limited oral control. Note the increase in residue resulting from thicker materials. Also note the patient’s spontaneous compensations to adjust for limited tongue movement.
Dysphagia and Head/Neck Cancer
CANCER AS A DISEASE
What Is Cancer?
Diagnosis of Cancer
Staging
TREATMENTS FOR HEAD/NECK CANCERS
Surgery
Radiation Therapy
Chemotherapy
DYSPHAGIA IN PATIENTS WITH HEAD/NECK CANCER
Dysphagia from Surgical Intervention
Resection
Physiologic Effect
Swallowing
Partial glossectomy
Difficulty holding and preparing a bolus for swallowing
Total glossectomy
Tonsil/base of tongue
Reduced anterior tongue range
Palatal resection
Velar leak results in retrograde movement of materials into the nasopharynx
Anterior/lateral floor of mouth
Partial pharyngeal resection
Hemilaryngectomy
Supraglottic laryngectomy
Incomplete posterior tongue movement, restricted arytenoids motion, partial airway closure
Total laryngectomy
Surgery for Oral Cancers
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Dysphagia and Head/Neck Cancer