Distending Media for Panoramic Hysteroscopy
Michael S. Baggish
Because of the substantial thickness of the uterine walls, a potential rather than true space forms the human uterine cavity. The endometrial mucosal lining has a tendency to bleed on contact; therefore, distention is necessary to view objects within the uterus when using the panoramic mode. Hysteroscopic distension may be obtained by filling the uterine cavity with either liquid or gaseous media. The only practical gaseous distension medium is carbon dioxide. On the other hand, several types of sterile fluids may be used to distend the uterus. It is convenient to divide the solutions into electrolytic and nonelectrolytic (Table 16.1). Those containing sodium (Na) and chloride (Cl) make up the electrolytic category whereas the other does not contain anions or cations. Table 16.2 lists various solutions including their content of Na, Cl, and their respective osmolalities. Separate from all other liquid media is the viscous polysaccharide Hyskon (32% dextran).
Gaseous Media
Carbon Dioxide
Carbon dioxide (CO2) has essentially the same index of refraction as air and provides a very clear view of the endometrium. Since it is a gas, it is easy to infuse and the least messy of all intrauterine distention media. CO2 is a good choice when small diagnostic sheaths (3 mm) are used, even if clearance around the telescope is limited. It is best suited for office panoramic hysteroscopy. Likewise, there is no problem in cleansing of instruments postoperatively as is the case with Hyskon. CO2 may be the medium of choice for panoramic hysteroscopic investigation of the endocervix. CO2, however, must be insufflated by means of a specialized apparatus designed for hysteroscopy and producing flow rates in the order of milliliters per minute (Fig. 16.1). Under no circumstances should laparoscopic insufflation equipment, which allows gas to flow at a rate of liters per minute, be used for hysteroscopy. Deaths have been reported when CO2 has been infused without proper flow and pressure regulation. The hysteroscopic insufflator should be calibrated regularly (every 6 to 12 months) for accuracy of pressure and flow readings.
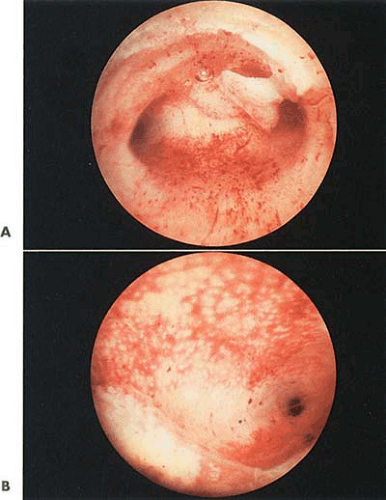
The most common mistake for inexperienced endoscopists is to instill CO2 at too high a flow rate, which produces obstructive bubbles of gas. It has been recommended that an initial flow rate of 30 mL/min is best to dilate and view the cervix followed by an increase to 40 to 50 mL/min flow to view the uterine cavity. The maximal flow rate should not exceed 100 mL/min (Fig. 16.2). The key to success with CO2 is a tight fit of the endoscope to the cervix and prevention of mucosal contact, which produces bleeding. CO2 hysteroscopy should be abandoned because of a foaming interaction between blood and gas (Fig. 16.3). Although many CO2 insufflators have pressure gauges exceeding 200 mm Hg, the upward pressure limit during CO2 endoscopy should rarely exceed 100 to 150 mm Hg. Although most hysteroscopy equipment sets include suction collars to be applied to the cervix to prevent the loss of CO2, the practicality of these devices is questionable; furthermore, they frequently provoke bleeding, which makes the hysteroscopic examination technically impossible. It is preferable to guide the endoscope through the cervix and gingerly slip just through the internal os (Figs. 16.4 and 16.5).
CO2 media is the least advantageous medium for operative hysteroscopy. A combination of CO2 for small-sheath diagnostic hysteroscopy followed by Hyskon for the operative portion of the case is a highly satisfactory approach (Fig. 16.6). Some of the newer CO2 insufflators can be automatically adjusted to cut off at an intrauterine pressure of 150 mm Hg and also to maintain continuous flow, which keeps the uterine walls reliably separated. Lindemann et al. have described experiments on German shepherd dogs that received direct femoral vein insufflation of CO2. At flow rates of 200 mL/min, minimal variations in pulse rate and breathing were observed. Toxic effects occurred at flow rates of 400 mL/min, and the animals died within 1 minute when 1,000 mL/min were insufflated.
When CO2 is used for uterine distention, the patient should never be placed in the head down (Trendelenburg) position. Reports in recent literature have described mill
wheel murmurs occurring sporadically in women undergoing CO2 hysteroscopy. It would be prudent for the gynecologist’s assistant to routinely auscult the heart to rule out CO2 embolus. Obviously, hearing the characteristic back-and-forth murmur necessitates immediately curtailing the hysteroscopy. More ominous events have been reported with gas embolism (e.g., cardiovascular collapse, respiratory arrest, and cyanosis). These conditions typically herald air embolism rather than CO2 embolus. Prior to the infusion of any gas or, for that matter, any medium, the plastic or rubber tubing should be routinely purged of air. Finally, sudden drops in CO2 monitored by the anesthesiologist suggest the occurrence of gas embolism.
wheel murmurs occurring sporadically in women undergoing CO2 hysteroscopy. It would be prudent for the gynecologist’s assistant to routinely auscult the heart to rule out CO2 embolus. Obviously, hearing the characteristic back-and-forth murmur necessitates immediately curtailing the hysteroscopy. More ominous events have been reported with gas embolism (e.g., cardiovascular collapse, respiratory arrest, and cyanosis). These conditions typically herald air embolism rather than CO2 embolus. Prior to the infusion of any gas or, for that matter, any medium, the plastic or rubber tubing should be routinely purged of air. Finally, sudden drops in CO2 monitored by the anesthesiologist suggest the occurrence of gas embolism.
TABLE 16.1 Comparison of Hysteroscopic Media | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Paschopoulous et al. compared saline versus CO2 as distending media for diagnostic hysteroscopy in 74 women. In the CO2 group, 89.7% completed the procedure versus 97.14% in the saline group. The diagnostic accuracy of the hysteroscopy was similar in both groups. The media were comparable in regard to patient discomfort. Litta et al. reported similar findings comparing CO2 and saline as distension media.
TABLE 16.2 Electrolyte Content and Osmolality of Hysteroscopic Distending Solutions | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Viscous Liquid Nonelectrolytic
Hyskon
Thirty-two percent dextran with a molecular weight of 70,000 is a crystal-clear, viscid fluid (Fig. 16.7). This electrolyte-free, branched polysaccharide has the consistency of honey in the liquid state and assumes the characteristic of airplane glue when dried. The advantages of this material as a medium to distend the uterus are multiple. It is the easiest material with which the beginner can learn panoramic hysteroscopy, since it consistently and promptly dilates the cervix canal and uterine cavity. The thickness of Hyskon diminishes the likelihood of massive retrograde leakage characteristic of other liquid media (Fig. 16.8). Most important, Hyskon mixes poorly with blood (is nonmiscible) and remains reasonably clear optically during the procedure. Because of its clarity, Hyskon is one of the best media to use for performing operative hysteroscopy, since debris can be easily aspirated and, if required, the cavity can be flushed with fresh material. By observing the flow of fragments of blood and cellular material suspended in the Hyskon, the endoscopist can rapidly and accurately identify the tubal ostia (Figs. 16.9 and 16.10). Finally, Hyskon is an excellent lubricant and may be used to facilitate dilatation of the cervix by dipping the dilators in the material before
engaging them in the external os. However, this same benefit may also create a hazard when the Hyskon spills onto the floor of the operating room, since it can cause personnel to slip and fall.
engaging them in the external os. However, this same benefit may also create a hazard when the Hyskon spills onto the floor of the operating room, since it can cause personnel to slip and fall.
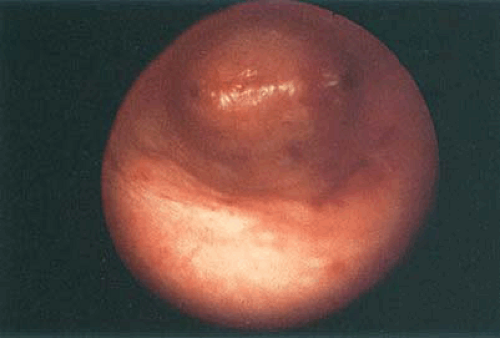
 FIGURE 16.3 The thickness of the endometrium under CO2 hysteroscopy may be estimated by depressing the sheath into the posterior wall of the uterus and observing the groove placed in the endometrium. |
Hyskon is not easy to instill through the narrow (5-mm) diagnostic sheaths, and it does require some degree of force to instill it even through the larger-diameter operative sheaths (Figs. 16.11 and 16.12). The ideal way to instill Hyskon into the uterine cavity is by the simple, handheld Hyskon pump attached to wide-bore, Luer-lock Hyskon tubing (Cook OB/GYN, Spencer, IN). An assistant can turn the screw mechanism at variable pitch to deliver either a smaller or greater volume of Hyskon within any given time frame (Fig. 16.13). The volume of instilled Hyskon must be carefully monitored. Every gram of Hyskon that is absorbed into the vascular space exerts a positive osmotic pull of approximately 20 mL of interstitial fluid. For example, if 100 mL of 32% Hyskon entered the circulation, the plasma volume would rapidly expand by 640 mL. At some point normal pulmonary wedge pressure will be exceeded, eventuating in pulmonary edema. Several studies have monitored total Hyskon volume instilled into the uterus together with Hyskon blood levels and operative time. Although no significant direct relationship between volume of Hyskon instilled and Hyskon reaction can be demonstrated, clearly volumes of 500 to 700 mL should induce warning signs and trigger the deployment of protective measures (e.g., cessation of the procedure and central venous pressure and
osmolality measurements). In particular, operative procedures that damage the endometrium and open up venous sinuses are most prone to affect vascular uptake of Hyskon.
osmolality measurements). In particular, operative procedures that damage the endometrium and open up venous sinuses are most prone to affect vascular uptake of Hyskon.
In addition to volume expansion, Hyskon (dextran) prolongs the bleeding time and coagulation mechanism by multipronged actions on fibrinogen, factor VIII, and platelets. Finally, since dextran 70 is a mixture of molecules ranging from 25,000 to 125,000, glomerular filtration may be adversely affected. The triad of pulmonary edema, bleeding diathesis, and anuria represents the full force of a Hyskon reaction at its worst. Although several articles have hypothesized a toxic effect of Hyskon on the lungs, the evidence for this is nonexistent and is in fact not plausible. The Hyskon reaction is explicable based on the exaggerated physiologic actions of dextran. Historically, Hyskon has proven to be an
exceedingly safe medium. Rarely, a true anaphylactoid reaction may occur. The latter should be treated by the prompt administration of 1:1,000 aqueous adrenaline followed by a short course of corticosteroids. An anaphylactoid event is far less likely to happen than a similar idiosyncratic reaction to the injection of a local anesthetic drug. On completion of hysteroscopy, all instruments and channels must be repeatedly flushed with very hot water to prevent solidification of the Hyskon (see Chapter 15). If this is not done, the dried material will assume the consistency of cement within these small channels. Nevertheless, with exposure to heat, the material liquefies and can be flushed out of the instruments. Hyskon has evolved as an excellent medium for office hysteroscopy. An office hysteroscopy with Hyskon can be completed in 5 to 10 minutes with a minimum of equipment and mess (Fig. 16.13). Mixing Hyskon with low-viscosity media creates a solution of different optical indices and should be avoided.
exceedingly safe medium. Rarely, a true anaphylactoid reaction may occur. The latter should be treated by the prompt administration of 1:1,000 aqueous adrenaline followed by a short course of corticosteroids. An anaphylactoid event is far less likely to happen than a similar idiosyncratic reaction to the injection of a local anesthetic drug. On completion of hysteroscopy, all instruments and channels must be repeatedly flushed with very hot water to prevent solidification of the Hyskon (see Chapter 15). If this is not done, the dried material will assume the consistency of cement within these small channels. Nevertheless, with exposure to heat, the material liquefies and can be flushed out of the instruments. Hyskon has evolved as an excellent medium for office hysteroscopy. An office hysteroscopy with Hyskon can be completed in 5 to 10 minutes with a minimum of equipment and mess (Fig. 16.13). Mixing Hyskon with low-viscosity media creates a solution of different optical indices and should be avoided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree