15
Depression, Erectile Dysfunction, and Coronary Heart Disease: An Interlinked Syndrome in Men
Case History
Mr. S. is a 54-year-old man who came for a consultation for his loss of libido and erectile dysfunction. He gives a 5-year history of fatigue, and was diagnosed to be hypothyroid and is on Levoxyl. He has consulted many physicians across the country seeking help for his sexual dysfunction symptoms. He admitted to being depressed about his situation, and was prescribed Celexa 40 mg by his psychiatrist. He has a history of angina, and recently underwent angioplasty and had stents introduced by his cardiologist. His urologist has been managing his erectile dysfunction, and the patient was prescribed Viagra. He felt dizzy after taking Viagra, and was thought to have an idiosyncratic reaction to the medication. Subsequently, he was switched to injection Caverject. The response was inadequate and he was subsequently put on an intramuscular compounded mixture of Trimix (prostaglandin, phentolamine, and papaverine). Other medications include Tenormin, Ativan, Lipitor, and a host of vitamins.
Past surgical history include liposuction, arthroscopy, cervical spine decompression, and angioplastic stent insertion. Physical examination findings include blood pressure (BP) 130/86, weight 225 pounds, body fat content 27.8%, and normal testicular and phallic examination. Laboratory results include total testosterone 230 ng/dL, free testosterone 48.4ng/dL (hypogonadal range), dihydrotestosterone 57ng/dL (normal), insulin-like growth factor-I (IGF-I) 264ng/dL (normal: 90–360), prolactin 10ng/dL (normal: 2–18), prostate-specific antigen (PSA) 0.6 (normal). Baseline electrocardiogram shows poor R wave progression, with S-T depression in V5,6. Review of angiographic studies shows two-vessel disease. Depression screening with the Geriatric Depression Scale (GDS) reveals a score of 10/15.
It is well known from epidemiology studies that the prevalence of depression, erectile dysfunction (ED), and coronary heart disease (CHD) increases with age.1,2 Physicians tend to consider them as separate entities, partly because physicians specialize in their respective fields. However, men presenting with problems in one organ system may already be aware of comorbid states in other organ systems, but may choose not to discuss them with their physicians. The National Institutes of Health recognized ED as a medical identity following a Consensus Development Conference in 1992,3 but it was not until the introduction of specific type 5 phosphodiesterase inhibitors that men began seeking help in large numbers. A similar situation occurred with depression before safe and effective treatments were available, and patients shunned treatments or were treated inappropriately. The symptoms related to depression, ED, and CHD are closely interlinked. An older patient presenting with symptoms of depression may have comorbid ED and/or comorbid CHD. Likewise, an older patient who presents with ED may have underlying CHD as well as depression.
This triad of depression, ED, and CHD in aging men is referred to as the DEC syndrome, and this chapter discusses the considerable overlap and interlinks among these three components. When a patient presents with one component of the DEC syndrome, physicians should also screen for the other two components (Fig. 15–1). The root cause of the syndrome may be a combination of arteriosclerosis, neurochemical imbalance, and hypogonadism that occurs with aging. The timing of symptoms coincides with hypogonadism in the andropause.4 Although testosterone replacement may improve depression,5 it should not be the first line of treatment. Likewise, although testosterone may improve coronary flow,6 patients with coronary problems should not be offered testosterone as first-line therapy, but may be offered supplementary testosterone if hypogonadism is present and if there are no contraindications.
FIGURE 15-1. The interlinked DEC (depression, erectile dysfunction, coronary heart disease) syndrome. The presence of one of these may be a harbinger of a larger, multifactorial problem.
Older Men with Depression Are More Likely to Develop Coronary Heart Disease
In general, the prevalence of depression in older women is higher than that in older men.7,8 There may be several reasons for this, including the possibility that men are less likely to report symptoms. However, it should be noted that rates of completed suicide are much higher in older men than in older women.9 Epidemiology studies reveal that in older men the prevalence of symptomatic depression is ∼15 to 25%, and the prevalence of major depression is ∼1.5 to 2%.7 CHD is the leading cause of death worldwide. The lifetime risk of developing CHD at age 40 is 50% for men and 33% for women. The cardioprotective role of estrogens in women is fairly well established.10 For several years, researchers have been arguing that testosterone provides cardioprotection for men.6 Thus, a complex relationship exists between depression in later life and CHD. Several prospective studies have suggested that depression may predispose an individual to an increased risk of developing CHD. For example, the Normative Aging Study, which included 1305 older men, demonstrated that depression is positively associated with the risk of CHD.11 In another longitudinal study, after 40 years of follow-up, investigators have found that depression appears to be an independent risk factor for incident CHD in male medical students.12 Ariyo and coworkers13 also found that depressive symptoms constitute an independent risk factor for the development of CHD and total mortality in older Americans. Figure 15–2 shows the association of increasing CHD and death with depression.
Depression can even increase the risk for cardiac mortality in subjects with and without cardiac disease at baseline.14 Some community surveys have observed an increase of ischemic heart disease among those with depression who were initially free of disease.15 Investigators have also found after long-term follow-up that history of depression in itself increases the risk of myocardial infarction and mortality.16,17 On the other hand, a multicenter study reported that baseline depressive symptoms were not related to subsequent cardiovascular events, but rather to prognosis.18 Table 15–1 is an example of a screening tool, the GDS, commonly used to screen for depression. This tool is particularly useful for older individuals.
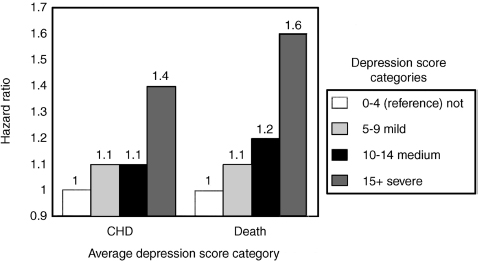
FIGURE 15-2 The association of coronary heart disease (CHD) and death rates with depression. (Adapted from Ariyo AA, Haan M, Tangen CM, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans: Cardiovascular Health Study Collaborative Research Group. Circulation 2000;102:1773–1779, with permission.)
| Choose the best answer for how you have felt over the past week (“Yes” or “No” for each): |
| Are you basically satisfied with your life? |
| Have you dropped many of your activities and interests? |
| Do you feel that your life is empty? |
| Do you often get bored? |
| Are you in good spirits most of the time? |
| Are you afraid that something bad is going to happen to you? |
| Do you feel happy most of the time? |
| Do you often feel helpless? |
| Do you prefer to stay at home, rather than going out and doing new things? |
| Do you feel you have more problems with memory than most? |
| Do you think it is wonderful to be alive now? |
| Do you feel pretty worthless the way you are now? |
| Do you feel full of energy? |
| Do you feel that your situation is hopeless? |
| Do you think that most people are better off than you are? |
Scoring: A “Yes” answer to items 2–6, 8–10, 12, 14, 15 is one point each. A “No” answer to items 1, 7, 11, 13 is one point each. A score of 0-5 is normal; a score of 6–15 suggests depression.
Older Men with Coronary Heart Disease Are More Likely to Suffer from Depression
It seems natural to think that a person with a chronic disorder is more likely to be depressed; thus, older men with coronary heart disease are more likely to be depressed. Studies have found that ∼45% of patients have been found to have either major or minor depression after a myocardial infarction (MI).19
Depression in older men with CHD can affect not only morbidity but also mortality. For instance, older post-MI patients with depression have nearly four times the risk of dying within the first 4 months after discharge.20 Therefore, there is an independent link between depression and cardiac mortality after MI. Bush et al21 reported that even minimal symptoms of depression could increase mortality risk after acute MI. Conversely, the national survey from 1971 to 1992 reported that depression was not a significant risk factor for CHD mortality.22 We hypothesize several biological reasons for the increased vulnerability of depressed patients to CHD and increased mortality: hypothalamic-pituitary-adrenocortical and sympathomedullary hyperactivity, diminished heart rate variability, ventricular instability and myocardial ischemia in reaction to mental stress, and alteration in platelet receptor and reactivity.23
Depression is underrecognized and undertreated in older men with CHD despite its consequences for prognosis. The clinical implication is that older men recovering from an MI should be evaluated for depression.19 The selective serotonin reuptake inhibitors (SSRIs) remain the most commonly prescribed class of antidepressants, but they may contribute to ED. As a result they may paradoxically exacerbate existing depression because the patient might not have expected the side effect of ED from SSRI, and the further loss of libido from the medication can be devastating. The mechanism of SSRIs on decreasing sexual functioning is dose related and may vary among patients based on serotonin and dopamine reuptake mechanisms, induction of prolactin release, anticholinergic effects, inhibition of nitric oxide synthase, and the propensity of the SSRI to accumulate over time.24 The use of tricyclic antidepressants such as amitriptyline, nortriptyline, and desipramine have particularly diminished in older men due to adverse anticholinergic and cardiovascular effects.25,26 Finally, treating depression may actually lower cardiovascular mortality, but studies are lacking at this point.25,26
Association of Erectile Dysfunction with Depression
Erectile dysfunction is a common condition among older men. The Massachusetts Male Aging Study, a cross-sectional, community-based, random survey of men in the Boston area, determined that the combined prevalence of minimal, moderate, and complete ED is ∼52%.27 According to the study, the age group of greatest concern for developing ED is between 40 and 70 years. Indeed, in that group, the prevalence of complete ED tripled, from 5 to 15%. The study also found that ED was directly correlated with hypertension, diabetes, alcoholism, anger, and depression. The probability of ED with treated hypertension was 0.15, with treated diabetes was 0.29, with excessive alcohol was 0.29, with anger was 0.35, and with severe depression was 0.9. This contrasts with the general risk of ED of 0.09 (p> .01).
Patients with ED are more likely to be clinically depressed, and patients with clinical depression often have ED. The Massachusetts Male Aging Study determined that ED was associated with depression. After controlling for potential confounders, moderate-to-complete ED was 1.82 times more likely in those who exhibited depressive symptoms as compared with those who did not display symptoms (p < .01).28
The study from the Johns Hopkins Sexual Behaviors Consultation Unit also revealed that approximately one in three men presenting with sexual dysfunction had comorbid psychiatric problems, including alcoholism and psychosocial stress.29 Men with ED had high levels of depressive, somatic, and anxious symptoms and scored very high on measures of overall psychological distress.
One possible explanation of how clinical depression can lead to the development of ED may be that depression causes overactivity of the autonomic nevous system. The overactive autonomic nervous system can then produce the inability to initiate or maintain relaxation of the corporal smooth muscle tissue because of increased adrenergic tone in the penile organ.30 Certain antidepressants such as fluoxetine, paroxetine, and sertraline can also result in side effects that can include ED. Many other substances and medications in addition to antidepressants can cause ED, including tobacco, antihypertensives, alcohol, anxiolytics, mood stabilizers, and antipsychotics.27,31 It is difficult to interpret the significance of antidepressant-induced ED because there are many confounders. In general, SSRIs can adversely influence orgasm, libido, and arousal.32 According to a study, bupropion may have the lowest overall rate of sexual dysfunction as compared with other antidepressants.33 The sustained-release formulation of bupropion had a sexual dysfunction rate of 25%. In contrast, the SSRIs Prozac (fluoxetine), Paxil (paroxetine), Zoloft (sertraline), and Celexa (citalopram) as well as Effexor (venlafaxine) and Remeron (mirtazapine) averaged ∼40%. When the different classes of antidepressants are compared, it appears that men report the least problems with sexual dysfunction while taking tricyclic antidepressants.31
Depressive symptoms in men with ED may improve with successful ED treatment.34 Sildenafil is efficacious for ED in men with mild-to-moderate depression. Improvement of ED is associated with marked improvement in depressive symptoms and quality of life (Fig. 15–3).35
Correlation of Erectile Dysfunction with Coronary Heart Disease
Erectile dysfunction may be due to compromised blood flow. An erection occurs as a result of increased blood flow to the corpus spongiosum of the penis upon vasodilatation. This is also mediated through neuronal control systems that are dependent on the autonomic nervous system. Arteriosclerosis can affect the penis as it does any other organ, and accounts for ED in approximately half of all affected men over the age of 50 years.36 If blood flow is inadequate, it usually signals vascular problems, especially if neurogenic controls are intact. The narrow vessels of the penis may be more prone to arteriosclerotic blockage than the larger vessels of the heart.37
Patients presenting with ED often have hypertension, and thus have a significantly higher prevalence of cardiovascular complications.38 Antihypertensive medication such as β-blockers can impair circulation, mask hypoglycemic symptoms, worsen asthma, and induce ED in older individuals. A study by Greenstein et al39 demonstrated a significant correlation between ED and the number of coronary vessels involved by arteriosclerosis. ED and CHD share some modifiable risk factors (e.g., smoking and overweight) in men free of ED and heart disease after 6 to 10 years of follow-up.40 Fig. 15–4 shows the relationship between CHD and ED.
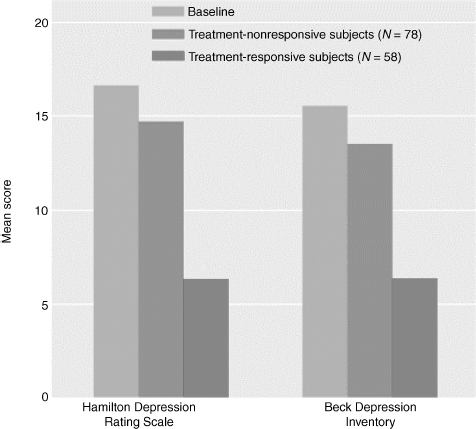
FIGURE 15-3. The effect due to sildenafil (Viagra) of improvement in erectile dysfunction on depressive symptoms. Sildenafil decreases both the Hamilton Depression Rotrip Scale as well as the Beck Depression Inventory. (Adapted from Seidman SN, Roose SP, Menza MA, et al. Treatment of erectile dysfunction in men with depressive symptoms: results of a placebo-controlled trial with sildenafil citrate. Am J Psychiatry 2001;158:1623–1630, with permission.)
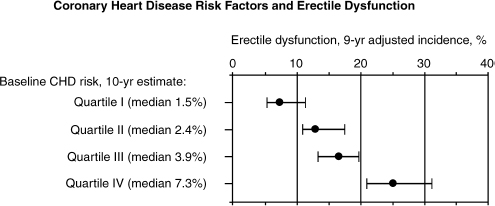
FIGURE 15-4. The association of erectile dysfunction and coronary heart disease risk factors. (Adapted from Feldman HA, Johannes CB, Derby CA, et al. Erectile dysfunction and coronary risk factors: prospective results from the Massachusetts Male Aging Study. Prev Med 2000;30:328–338, with permission.)
Many managed care formularies have put restrictions on the availability of sildenafil. Unrestricted availability of licensed treatments for ED may encourage men to present for investigation, enabling early detection of CHD.37
Clinical Implications of the DEC Syndrome in Older Men
It is certainly possible that older men present with isolated and unrelated symptoms of depression, ED, and CHD. However, epidemiology studies suggest that these three conditions overlap.27 The existence of one symptom should lead the physician to suspect that the patient may be suffering from the other two as well. However, it may be very difficult to determine which of the three disorders may have caused the others (e.g., did the depression come first and cause ED?). A mutually reinforcing two-way model has been proposed.1 Health status, demographics, lifestyle, medications, and psychosocial events can adversely influence the DEC syndrome, and may even be responsible for its etiology. Here are some guidelines for clinicians dealing with men over the age of 50:
• Older men presenting with CHD should be screened for symptoms of depression. There are simple and quick geriatric instruments such as the GDS that have been proven to be sensitive and specific for an older population.41
• Older men presenting with depression or ED should also be routinely screened for risk factors associated with CHD. It is good practice to do a baseline electrocardiogram, as treatment with some antidepressants, such as the tricyclic antidepressants amitriptyline and nortriptyline may have side effects including dysrhythmias, atrioventricular (AV) blocks, ventricular ectopics, and supraventricular tachycardia. Other side effects can also include dry mouth, exacerbation of glaucoma, postural hypotension, dizziness, and faintness. A thallium stress test can also rule out concomitant coronary problems.
• Depression in older men may sometimes also be associated with hypogonadism, and it is prudent to check testosterone levels, especially if depression is associated with symptoms including fatigue, loss of libido, and memory problems.4
• Older men presenting with ED should be asked about symptoms of depression. Sometimes it is the medication for the treatment of depression rather than the depression itself that causes the ED. A complete history of medication use is important to acquire.
Discussion of the Case History
Mr. S. typifies a patient with the DEC syndrome. He may at the same time be hypogonadal because of Leydig cell failure from aging. The root cause of this syndrome is a combination of vasculopathy and hypotestosteronemia. He has had narrowing of his coronary arteries, which required stent placements and as such it will not be surprising to find that his penile vasculature will be compromised, leading to vascular ED. The positive response to Viagra and PPR suggests that he does have vascular problems. Beta-blockers used to treat hypertension (Tenormin) may further compromise his ED, and so the patient was switched to an angiotensin-converting enzyme (ACE) inhibitor (Altace). He was put on a therapeutic trial of androgen replacement, but his response was described as marginal. His depression improved with the androgen replacement. The patient was taught how to self-administer the PPR injection. Key to the management of this patient is control of cardiac risk factors including the control of hypercholesterolemia and blood pressure, weight loss, and nutrition and exercise counseling. The patient was also educated about realistic goals in that he had to play a part in improving his own quality of life by paying attention to diet and exercise and that there was no single magic pill for his problem. He is at the moment considering revascularization surgery for his penis.
Conclusion and Key Points
The prevalence of depression, ED, and CHD increases with age, and the symptoms related to these three illnesses are closely interlinked. When a patient presents with one component of the DEC syndrome, the term used to refer to this triad of comorbid conditions, physicians should also screen for the other two components. Studies have shown that depression may predispose an individual to an increased risk of developing CHD, and older men with CHD are more likely to be depressed. Likewise, patients with ED are more likely to be clinically depressed, and patients with clinical depression often have ED. Furthermore, patients presenting with ED are often hypertensive, and thus have a significantly higher prevalence of cardiovascular complications.
Multifactorial problems require multifactorial approaches, and the care of older men can improve if physicians are aware of this interlinked syndrome. The care of older men may sometimes be fragmented, as patients presenting with depression, for example, may be seen by psychiatrists who may not have the capabilities to screen for CHD. Likewise, it may be possible that urologists attending to issues pertaining to ED may not have the time to deal with treatment options for depression. It is important to remember the acronym DEC, as it can serve to remind the specialist to refer the patient to the primary care physician or to other specialists for treatment of the other two components of the DEC syndrome. Primary care physicians should be attending to all three components and should not neglect the other components when an older patient presents with a relevant symptom such as depression, ED, or angina. It may sometimes be impossible to address all problems at one sitting, and the primary care physician may want to schedule additional appointments to deal with the other issues. Multifactorial problems require multifactorial approaches, and the care of older men can improve if physicians are aware of this interlinked syndrome.
REFERENCES
1. Goldstein I. The mutually reinforcing triad of depressive symptoms, cardiovascular disease, and erectile dysfunction. Am J Cardiol 2000;86:41F–45F
2. Roose SP, Seidman SN. Sexual activity and cardiac risk: is depression a contributing factor? Am J Cardiol 2000;86:38F–40F
3. NIH Consensus Development Panel on Impotence. Impotence. JAMA 1993;270:83–90
4. Tan RS, Philip PS. Perceptions of and risk factors for andropause. Arch Androl 1999;43:97–103
5. Barrett-Connor E, Von Muhlen DG, Kritz-Silverstein D. Bioavailable testosterone and depressed mood in older men: the Rancho Bernardo Study. J Clin Endocrinol Metab 1999;84: 573–577
6. Ong PJ, Patrizi G, Chong WC, et al. Testosterone enhances flow-mediated brachial artery reactivity in men with coronary artery disease. Am J Cardiol 2000;85:269–272
7. Jeste DV, Alexopoulos GS, Bartels SJ, et al. Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry 1999;56:848–853
8. Blazer D, Hughes DC, George LK. The epidemiology of depression in an elderly community population. Gerontologist 1987;27:281–287
9. Brown GK, Bruce ML, Pearson JL. High-risk management guidelines for elderly suicidal patients in primary care settings. Int J Geriatr Psychiatry 2001;16:593–601
10. Roeters van Lennep JE, Westerveld HT, Erkelens DW, van der Wall EE. Risk factors for coronary heart disease: implications of gender. Cardiovasc Res 2002;53:538–549
11. Sesso HD, Kawachi I, Vokonas PS, Sparrow D. Depression and the risk of coronary heart disease in the Normative Aging Study. Am J Cardiol 1998;82:851–856
12. Ford DE, Mead LA, Chang PP, et al. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med 1998;158:1422–1426
13. Ariyo AA, Haan M, Tangen CM, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans: Cardiovascular Health Study Collaborative Research Group. Circulation 2000;102:1773–1779
14. Penninx BW, Beekman AT, Honig A, et al. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry 2001;58:221–227
15. Glassman AH, Shapiro PA. Depression and the course of coronary artery disease. Am J Psychiatry 1998;155:4–11
16. Pratt LA, Ford DE, Crum RM, et al. Depression, psychotropic medication, and risk of myocardial infarction: Prospective data from the Baltimore ECA Follow-Up. Circulation 1996;94: 3123–3129
17. Barefoot JC, Schroll M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation 1996;93:1976–1980
18. Wassertheil-Smoller S, Applegate WB, Berge K, et al. Change in depression as a precursor of cardiovascular events: SHEP Cooperative Research Group (Systolic Hypertension in the Elderly). Arch Intern Med 1996;156:553–561
19. Romanelli J, Fauerbach JA, Bush DE, Ziegelstein RC. The significance of depression in older patients after myocardial infarction. J Am Geriatr Soc 2002;50:817–822
20. Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation 2002;105:1049–1053
21. Bush DE, Ziegelstein RC, Tayback M, et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol 2001;88:337–341
22. Chang M, Hahn RA, Teutsch SM, Hutwagner LC. Multiple risk factors and population attributable risk for ischemic heart disease mortality in the United States, 1971–1992. J Clin Epidemiol 2001;54:634–644
23. Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998;55:580–592
24. Rosen RC, Lane RM, Menza M. Effects of SSRIs on sexual function: a critical review. J Clin Psychopharmacol 1999; 19(1):67–85
25. Mamdani MM, Parikh SV, Austin PC, Upshur RE. Use of antidepressants among elderly subjects: trends and contributing factors. Am J Psychiatry 2000;157:360–367
26. Kroenke K. A 75-year-old man with depression. JAMA 2002; 287:1568–1576
27. Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994;151:54–61
28. Araujo AB, Durante R, Feldman HA, et al. The relationship between depressive symptoms and male erectile dysfunction: cross-sectional results from the Massachusetts Male Aging Study. Psychosom Med 1998;60:458–465
29. Fagan PJ, Schmidt CW Jr, Wise TN, Derogatis LR. Sexual dysfunction and dual psychiatric diagnoses. Compr Psychiatry 1988;29:278–284
30. Krane RJ, Goldstein I, Saenz de Tejada I. Impotence. N Engl J Med 1989;321:1648–1659
31. Gitlin MJ. Psychotropic medications and their effects on sexual function: diagnosis, biology, and treatment approaches. J Clin Psychiatry 1994;55:406–413
32. Keller Ashton A, Hamer R, Rosen RC. Serotonin reuptake inhibitor-induced sexual dysfunction and its treatment: a large-scale retrospective study of 596 psychiatric outpatients. J Sex Marital Ther 1997;23:165–175
33. Croft H, Settle E Jr, Houser T, et al. A placebo-controlled comparison of antidepressant efficacy and effects on sexual functioning of sustained-release bupropion and sertraline. Clin Ther 1999;21:643–658
34. Muller MJ, Benkert O. Lower self-reported depression in patients with erectile dysfunction after treatment with sildenafil. J Affect Disord 2001;66:255–261
35. Seidman SN, Roose SP, Menza MA, et al. Treatment of erectile dysfunction in men with depressive symptoms: results of a placebo-controlled trial with sildenafil citrate. Am J Psychiatry 2001;158:1623–1630
36. Benet AE, Melman A. The epidemiology of erectile dysfunction. Urol Clin North Am 1995;22:699–709
37. Kirby M, Jackson G, Betteridge J. Friedli K. Is erectile dysfunction a marker for cardiovascular disease? Int J Clin Pract 2001; 55:614–618
38. Burchardt M, Burchardt T, Anastasiadis AG, et al. Erectile dysfunction is a marker for cardiovascular complications and psychological functioning with hypertension. Int J Impot Res 2001;13:276–281
39. Greenstein A, Chen J, Miller H, et al. Does severity of ischemic coronary disease correlate with erectile function? Int J Impot Res 1997;9:123–126
40. Feldman HA, Johannes CB, Derby CA, et al. Erectile dysfunction and coronary risk factors: prospective results from the Massachusetts Male Aging Study. Prev Med 2000;30:328–338
41. Yesavage JA. Geriatric depression scale. Psychopharmacol Bull 1988;24:709–711
< div class='tao-gold-member'>









