Chapter 35 COLPOCYSTOURETHROPEXY
Genuine stress urinary incontinence (SUI) is a specific entity directly related to an anatomic abnormality that results in impaired efficiency of the urethral sphincteric mechanism, allowing loss of urine with increased intra-abdominal pressure. Owing to recent advances in urodynamic studies and the appreciation of the pathophysiology of true SUI, the treatment of this problem has become better understood; consequently, the purpose of surgical repair and the means of achieving it can be clearly defined.
SURGICAL PRINCIPLES
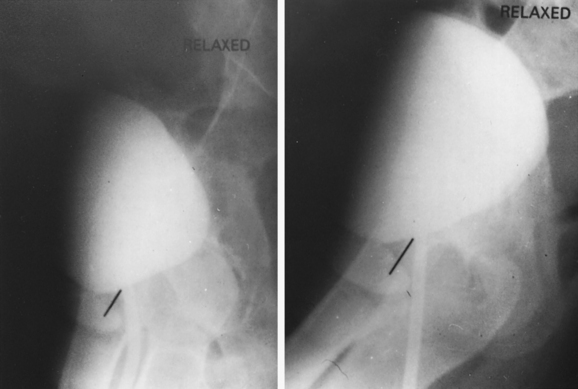
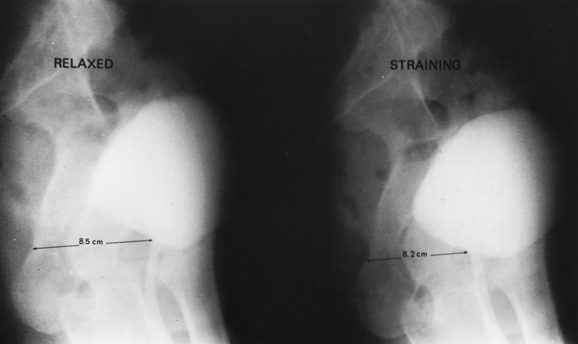
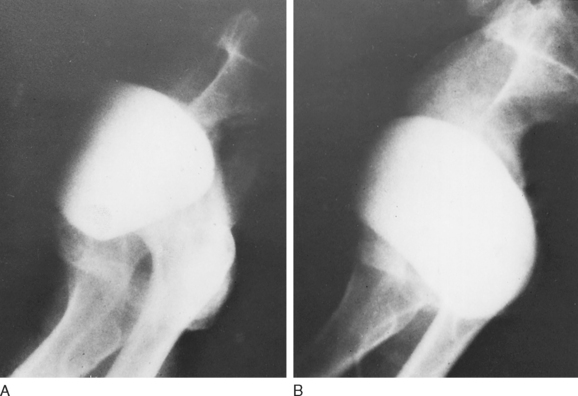
A lateral cystogram obtained with a radiopaque, soft red Robinson catheter permits visualization of the vesicourethral segment and its anatomic relationships. Two exposures with the patient in the absolute lateral position, first relaxed and then with maximum straining (Figs. 35-1 and 35-2), will demonstrate the extent of mobility and thus the effectiveness of the support to the vesicourethral segment. This study permits evaluation of both the normal resting position and the extent of mobility. If the resting position is abnormal (lower than normal), if the mobility of the vesicourethral segment is excessive (Fig. 35-3), or if both conditions are present, the lateral cystogram will confirm the anatomic basis for the existing and clinically established fact of SUI. It must be emphasized that this cystographic study does not permit the diagnosis of SUI but demonstrates the presence of the basic anatomic abnormality responsible for genuine SUI.
Surgical repair should attempt to restore normal position and support without compression or obstruction. SUI is encountered frequently in multiparous women after middle age as a result of pelvic floor weakness, which might have begun earlier in life but has progressed and become manifest. As mentioned earlier, the intrinsic sphincteric mechanism is essentially normal. However, because of the laxity of the pelvic floor and the weakness of the normal mechanism of support to the vesicourethral segment, the latter tends to lie abnormally low and exhibits excessive mobility with increased intra-abdominal pressure (see Fig. 35-3) or with assumption of the upright position. The intrinsic sphincteric mechanism can be restored to normal function once this anatomic abnormality is corrected, without any need to plicate, constrict, or otherwise directly interfere with the sphincteric unit itself.
It is imperative to avoid the creation of any obstruction or damage to the delicate intrinsic sphincteric muscular element. If this principle is adhered to, the sphincter will regain and maintain its effectiveness, and the repair will be permanent. In my opinion, the suprapubic approach is the best way to achieve this goal.