Chapter 50 Biliary Intervention in Acute Gallstone Pancreatitis
Gallstones are the most common cause of pancreatitis, accounting for approximately 35% of cases of acute pancreatitis (AP) in the United States and Europe1,2 and up to 65% of cases in Asia.3 The majority of patients with acute gallstone pancreatitis (AGP) will follow a benign clinical course. However, up to 25% of patients will progress to severe acute pancreatitis (SAP), which confers a significant increase in morbidity and mortality.4 Although the exact mechanism by which gallstones cause AP remains elusive, the correlation between gallstones and AP is well documented. Gallstones were found in the stool of approximately 90% of patients with recent AGP, whereas they were found in only 10% of patients with cholelithiasis without AP.5 In addition, persistent obstruction of the ampulla by a common bile duct (CBD) stone is believed to result in more severe pancreatic injury.6 Endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (ES) are effective tools for removal of an obstructing stone and reestablishment of biliary drainage,3,7,8 with success rates exceeding 90%. However, performing an ERCP is not without risk of adverse events, especially if performed emergently in patients with acute pancreatitis in less than ideal circumstances (Box 50.1).
Box 50.1
Key Points
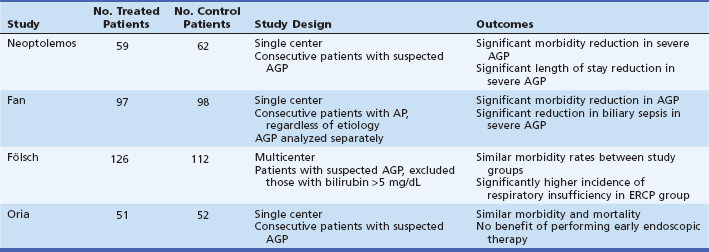
 Four randomized studies addressing the role of ERCP in acute gallstone pancreatitis (AGP) were evaluated.
Four randomized studies addressing the role of ERCP in acute gallstone pancreatitis (AGP) were evaluated.
 Two studies demonstrated a benefit for those patients who underwent early ERCP and two demonstrated no significant difference between the early intervention and the conservative management group.
Two studies demonstrated a benefit for those patients who underwent early ERCP and two demonstrated no significant difference between the early intervention and the conservative management group.
 Two meta-analyses of these studies and a Cochrane review confirmed that the morbidity benefit of early ERCP is seen only in those patients with severe AGP.
Two meta-analyses of these studies and a Cochrane review confirmed that the morbidity benefit of early ERCP is seen only in those patients with severe AGP.
Diagnosis of Acute Gallstone Pancreatitis
Serum amylase levels have been shown to be higher in patients with AGP in comparison to those with alcohol-related AP and authors have postulated that a serum amylase level greater than 1000 indicates a biliary cause of AP.9,10 The presence of elevated liver chemistries has been evaluated and meta-analysis of these studies demonstrated that elevations of alanine aminotransferase (ALT) levels greater than threefold are suggestive of AGP.11 This study also found that total bilirubin level and alkaline phosphatase level were not useful and that aspartate aminotransferase (AST) level was no more useful than ALT level in diagnosing AGP. In addition, once AGP is established, patients with rising serum pancreatic enzymes or liver tests carry a fourfold risk of persistent CBD stones and approximately a threefold risk of adverse events when compared to patients with stable or declining laboratory values.12
Demonstration of cholelithiasis by imaging can further support the diagnosis of AGP. Abdominal ultrasound is the preferred initial imaging study given its high sensitivity and specificity (>95%) for gallstones.13 In the setting of AP, however, this sensitivity can be reduced due to presence of overlying air-filled loops of bowel.14 A more recent study found that abdominal ultrasound in the setting of AP remains a very sensitive test (86%) and, when combined with an elevation of ALT greater than 80 IU/L, is 98% sensitive and 100% specific for a biliary etiology.15 The lack of biliary dilation on ultrasound does not exclude choledocholithiasis as the cause of AP, especially in the first 48 hours of an attack.
The attendant risks of ERCP, the gold standard for detecting choledocholithiasis, have prompted the study of magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) as alternative diagnostic modalities. MRCP has been shown to have high sensitivity (84% to 95%) and high specificity (96% to 100%) for the diagnosis of common duct stones.16–18 The most common cause of a false negative MRCP was gallstone size of less than 5 mm.17 A prospective study comparing multiple imaging modalities (abdominal ultrasound, computed tomography [CT], MRCP, ERCP, and intraductal ultrasound) showed an 80% sensitivity of MRCP at detecting choledocholithiasis with a 90.6% agreement between ERCP and MRCP.19 EUS demonstrates equivalent accuracy to MRCP for the detection of choledocholithiasis.18 EUS can detect choledocholithiasis at a sensitivity of 98% with 99% specificity, and may safely replace diagnostic ERCP.20,21 In a recent analysis the results of EUS were helpful in identifying a biliary cause for acute pancreatitis in half of the patients with unknown etiology and negative imaging.22
Assessment of Severity of Acute Pancreatitis
Early recognition of patients with SAP is crucial, as these patients will require intensive care management and will likely benefit from early endoscopic intervention.3,8,23 Several clinical and radiographic parameters have been used to evaluate the severity of AP: the presence of organ failure; prognostic indices; and the presence of local adverse events such as pancreatic necrosis, abscess, or fluid collection by cross-sectional imaging. With these parameters, the Atlanta Classification of 1992 categorized AP into mild or severe. Furthermore, it standardized the definition of SAP as the presence of local adverse events and/or organ failure (Table 50.1), or an Acute Physiology and Chronic Health Evaluation II (APACHE II) (Table 50.2) score greater than 8, or Ranson criteria greater than 3.24
Table 50.1 Definition of Severe Adverse Events Requiring Intensive Care Unit Monitoring and Treatment
| System | Adverse Event |
|---|---|
| Pulmonary | Mechanical ventilation; pneumonia with hypoxemia (PaO2 ≤60 mm Hg); hypoxemia (PaO2 ≤60 mm Hg) or dyspnea requiring frequent assessment of need for intubation |
| Cardiovascular | Hypotension requiring pressor support; ischemia or acute myocardial infarction noted on electrocardiogram or cardiac enzymes; new-onset arrhythmia other than sinus tachycardia |
| Infectious | Sepsis of any origin |
| Renal | New-onset oliguric or nonoliguric renal failure or new-onset dialysis |
| Hematologic | Disseminated intravascular coagulation and platelet counts <50 × 109/L |
| Neurologic | Glasgow Coma Scale score ≤9 and diminished responsiveness or agitation (requiring significant sedation) with need for frequent airway monitoring |
| Gastrointestinal | Stress ulcer with hematemesis or melena tract (requiring >2 U of blood per 24 hours) |
Reproduced with permission from Meek K, Toosie K, Stabile BE, et al. Simplified admission criterion for predicting severe complications of gallstone pancreatitis. Arch Surg. 2000;135(9):1048-1052.
Table 50.2 The APACHE II Scoring System*
| Physiologic Variable | Reference Range |
|---|---|
| Rectal temperature (°C) | 36 to 38.4 |
| Mean arterial pressure (mm Hg) | 70 to 109 |
| Heart rate (ventricular response) (beats/min) | 70 to 109 |
| Respiratory rate (breaths/min) | 12 to 24 |
| Oxygenation (mm Hg) | PaO2 − PaO2 <200 or PO2 >70 |
| Arterial pH | 7.33 to 7.49 |
| Serum sodium level (mmol/L) | 130 to 149 |
| Serum potassium level (mmol/L) | 3.5 to 5.4 |
| Serum creatinine level (µmol/L [mg/dL]) (double point score for acute renal failure) | 0.6 to 1.4 (53 to 123) |
| Hematocrit | 0.30 to 0.46 |
| Leukocyte count (× 109/L) | 0.003 to 0.015 |
| Glasgow Coma Scale (GCS) score | 15—actual GCS score |
*To calculate the Acute Physiology and Chronic Health Evaluation (APACHE) II score, the 12 physiologic variables are assigned points between 0 and 4, with 0 being normal and 4 being the most abnormal. The sum of these values is added to a point weighting for patient age (≤44 years = 0; 45 to 54 years = 2; 55 to 64 years = 3; 65 to 74 years = 5; >75 years = 6) and a point weighting for chronic health problems. PaO2 − PaO2 indicates alveolar-arterial difference in partial pressure of oxygen.
Data from Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818-829.
Over the past two decades the Atlanta Classification of 1992 has come under significant criticism as the understanding of the pathophysiology of the disease process and therapeutic options improved. The Classification lacked differentiation between transient and persistent organ failure and definitions of local adverse events (e.g., fluid collections, necrosis, and pseudocysts), which led to its inconsistent use.25 A recent review of 447 studies showed significant variations in the use of the classification system in both research and clinical settings.26 This has led the Acute Pancreatitis Classification Working Group to formulate a new set of tools for assessment and definition of severity of AP incorporating scoring systems such as the Marshall scoring system and the Sequential Organ Failure Assessment (SOFA) score. The differences in the classification schemes are outlined in Fig. 50.1. However, the revised criteria have not been validated and consensus needs to be established between radiologists and clinicians before using them.
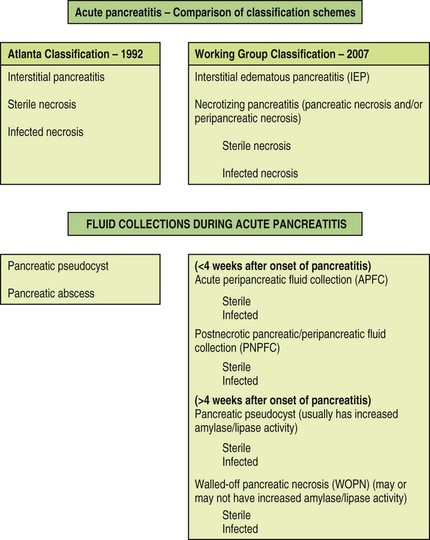
Fig. 50.1 Comparison of classification schemes for acute pancreatitis.
(Adapted from the Acute Pancreatitis Classification Working Group.)
Organ failure, particularly persistent or worsening organ failure, is a strong determinant of mortality in patients with SAP.27,28 Though many definitions of organ failure have been used, more recent studies use the multiple organ dysfunction syndrome (MODS) score or the systemic inflammatory response syndrome (SIRS) score to ensure that findings can be generalized.29,30 Mortality in the setting of AP with organ failure can range from 20% to as high as 50% and is dependent on the duration, severity, and number of organ systems in failure.23,24,31 Prognostic indices have been formulated to predict which patients are more likely to develop severe AGP and to direct appropriate care toward that group. These include Ranson criteria (biliary version), modified Glasgow criteria, Bedside Index for Severity in Acute Pancreatitis (BISAP), Harmless Acute Pancreatitis Score (HAPS), blood urea nitrogen levels, and APACHE II score.32–34 Radiologic scores such as the Balthazar score and the modified CT severity index, which are based on the extent of pancreatic necrosis and fluid collections, have been shown to correlate with mortality.35,36 Several biochemical markers of inflammation have been studied to predict SAP, but serum C-reactive protein level greater than 150 mg/L at 48 to 72 hours after symptom onset remains the standard.37 Recent data suggest that a genetic polymorphism that confers an enhanced chemokine response to an inflammatory stimulus is a risk factor for progression to SAP.38 The search continues for a biochemical marker that can be measured easily in the first 24 hours of AP and reliably predicts progression to severe disease.
Treatment of Acute Gallstone Pancreatitis
The mainstay of initial therapy for all forms of AP remains supportive care, including aggressive hydration, adequate nutritional support, pain control, and often an intensive care unit (ICU) in case of SAP.39 Persistent biliary obstruction or stone impaction at the ampulla was thought to worsen the course of pancreatitis. For this reason, in the 1980s, early surgery and biliary decompression were advocated as the treatment of choice in patients with AGP.40 However, clinical trials showed that the morbidity and mortality was increased in patients with severe AGP who underwent early surgery.41,42 During the last 30 years, ERCP has provided a less invasive approach to biliary diseases. Numerous papers have been published evaluating the role of ERCP in early biliary pancreatitis, which will be discussed in this section.
Early ERCP with or without ES in AGP: the Studies
Multiple studies, including randomized controlled trials (RCTs), have been published in the past 3 decades pertaining to early ERCP-guided therapy of AGP. Of note are four randomized controlled trials, two meta-analyses, and a Cochrane review conducted to better define the role of early ERCP and ES.3,7,8,43–46 These studies differ on the assessment of pancreatitis severity, timing to ERCP, exclusion criteria, and possibly endoscopic expertise. The four RCTs designed to assess the safety and benefit of early ERCP in AGP are described below and summarized in Table 50.3.
In 1988, Neoptolemos et al. published a landmark study comparing early ERCP and ES to conservative management of AGP.8 This study was performed from 1983 through 1987 and published in 1988. The investigators randomized 121 of 146 consecutive patients who presented to a single institution with suspected AGP to receive either conservative management or early ERCP within 72 hours of admission. The diagnosis of AGP was established by ultrasound and laboratory data. The severity of pancreatitis was predicted within 48 hours of admission using the modified Glasgow criteria.47 If choledocholithiasis was found on ERCP, an ES with stone extraction was performed. Outcome measures included mortality, length of stay, local adverse events, and organ failure. Predicted SAP was present in 44% of all patients enrolled (25 of 59 in the ERCP group and 28 of 62 in the conservative management group). ERCP was successful in 94% of mild disease cases and 80% of severe disease cases. One ERCP-related adverse event, a case of vertebral osteomyelitis, was cited. There were no cases of ERCP-related hemorrhage, cholangitis, or perforation.
In 1993, Fan and colleagues published a trial randomizing 195 patients with AP of all etiologies to undergo urgent ERCP within 24 hours of hospital admission or conservative management followed by selective ERCP for clinical deterioration.3 The authors used this approach of selecting all patients with pancreatitis to minimize selection bias. Analysis of the subgroup of patients with AGP revealed that 127 of the 195 randomized patients (65%) had biliary stones. Sixty-four of the 97 patients randomized to early ERCP were found to have biliary stones and 38 of these required ES for CBD or ampullary stones. Of the 98 patients in the conservative therapy group, 63 had biliary stones and 27 of these patients required ERCP for clinical deterioration. Ten of these patients were found to have CBD or ampullary stones. Cholangitis remained a significant confounding factor in the study population.
In 1997 the German Study Group on Acute Biliary Pancreatitis conducted a prospective multicenter study. In this study Fölsch et al. randomized 126 patients with AGP to early ERCP within 72 hours of the onset of symptoms and 112 patients with AGP to conservative management.7 The inclusion criteria in this study were distinct from the previous studies in that patients with obstructive jaundice (total bilirubin >5 mg/dL) were excluded. In doing so the investigators sought to determine the effect of early ERCP on AGP independent of its known benefit in patients with cholangitis.48 In these patients with AP the diagnosis of AGP was made if gallstones were seen on imaging or if two of three serum liver chemistry values (ALT, alkaline phosphatase, and/or total bilirubin) were abnormal. The severity of pancreatitis was predicted by the modified Glasgow criteria. Early ERCP was successful in 96% of the treatment group and 46% of the patients in this group were found to have choledocholithiasis. Elective ERCP was required in 20% of the conservative treatment group and 59% of those patients were found to have bile duct stones.
In 2007, Oria et al. published a randomized clinical trial testing the hypothesis that early endoscopic intervention performed on patients with AGP and biliary obstruction reduces systemic and local inflammation.43 This was a single center randomized clinical trial performed in Argentina between 2001 and 2005. Consecutive patients presenting to the emergency room within 48 hours after onset of AGP were enrolled. The diagnosis was made based on presence of abdominal pain, elevated serum amylase to three or more times normal, choledocholithiasis on ultrasound, CT evidence of pancreatitis, and absence of other causes of AP. Included patients had a bile duct diameter ≥8 mm on admission ultrasound and a bilirubin ≥1.2 mg/dL. Patients were excluded if they could not undergo endoscopy or if they had acute cholangitis. Patients that met these criteria were randomized to receive either early endoscopic intervention (n = 51) or early conservative management (n = 52). All patients received antibiotics. Severity of attack was predicted using the APACHE II scale. The primary outcome of the study was to determine whether early endoscopic therapy could reduce organ failure scores during the first week after admission and limit the extension of pancreatic and peripancreatic lesions. SOFA score was also calculated. CT findings were graded using the CT severity index.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree