Fig. 1.1
Structure of the nasolacrimal drainage system
Secretory system (main and minor lacrimal glands, eyelids) that forms the tear film and hand it out on the ocular surface
1.2 Embryology
Knowledge of the embryology is necessary to understand congenital abnormalities of the lacrimal drainage system.
The lacrimal gland develops at one and a half month’s gestation as solid epithelial buds arise from the ectoderm of the superior conjunctiva fornix; at 13–14 weeks of gestation, arborization of the glandular parenchyma begins and the gland organizes itself in glandular lobe [1, 2]. The development continues until 3–4 years after birth.
At 32 days of embryonic gestation, the maxillary and frontonasal prominences appear and a groove forms between them (Fig. 1.3a). Ectoderm from the floor of the groove becomes entrapped between the prominences and detaches from the surface ectoderm as a cord of epithelium.
Fig. 1.3
Development of the canaliculi, lacrimal sac, and nasolacrimal duct
The inferior part of this cord forms the nasolacrimal duct while the superior one will enlarge to form the lacrimal sac and gives off two columns of cells that grow into the eyelid margins to become the canaliculi (Fig. 1.3b–c). Canalization of the epithelial cords begins at 4 months of gestation proceeding first in the lacrimal sac, then in the canaliculi and at last in the nasolacrimal duct [3]. Rapid growth of the maxillary bone in relation to the frontal bone results in greater lateral stretching of the inferior canaliculus with a subsequent lateral position of the inferior punctum with respect to the superior punctum. Remnants of epithelium within the cords form valve-like folds (Fig. 1.3d) A membranous covering consisting of conjunctival and canalicular epithelium remains over the puncta, and a covering consisting of nasal and nasolacrimal epithelium (called membrane of Hasner) remains over the nasolacrimal duct outlet. Punctal membranes open at full-term; however, the membrane of Hasner remains imperforate in up to 70 % of newborns. This usually opens within the first month but may remain imperforate for a longer time, resulting in epiphora or mucopurulent discharge.
1.3 Secretory System
1.3.1 Lacrimal Glands
Tears are produced by main and accessory lacrimal glands.
The main lacrimal gland is an almond-shaped gland of 20 × 12 × 5 mm in size, situated in the lacrimal fossa in the upper outer portion of the orbital cavity. It is not an encapsulated structure but rather it is an aggregated collection of lobules of secretory tissue set in the superotemporal orbital fat, with interlobular ducts converging into the main excretory ducts in the superotemporal fornix. The acini are made up of serous secretory cells laying on basal myoepithelial cells. Myoepithelial cells are not present in the terminal intralobular ductules or in the interlobular ducts (Fig. 1.4) [4].
Fig. 1.4
Microscopic structure of the lacrimal gland
The main lacrimal gland is split into two lobes, the palpebral and the orbital one, by the lateral horn of the levator aponeurosis. The palpebral lobe measures about one-third the volume of the orbital lobe; it is placed under the levator aponeurosis in the lateral part of the superior eyelid. The orbital lobe lies within its fossa, a concavity in the lateral portion of the orbital roof. Fibrous septa known as Sommering’s ligaments run from the gland to attach it more firmly to the periosteum of the lacrimal gland fossa. Whitnall’s ligament also adds support for lacrimal gland suspension.
The orbital lobe has 2–6 secretory ducts which pass through the palpebral lobe and join with palpebral lobe ones to form 6 to 12 tubules which drain the secretion in the superior fornix (Fig. 1.5) [4].
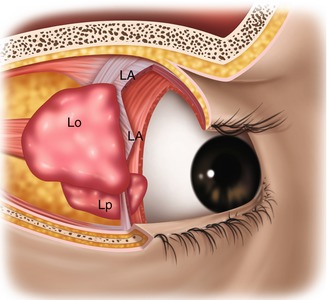
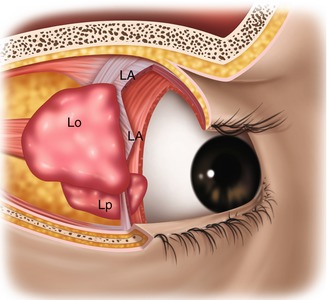
Fig. 1.5
Orbital and palpebral lobes of the lacrimal gland. Lo orbital lobe, Lp palpebral lobe, LA levator aponeurosis (From Zide and Jelks [17])
Accessory lacrimal glands are described in the following [5]:
Krause’s glands are mucous glands placed underneath the eyelid where the upper and lower conjunctivae meet; there are about 20–40 ones in the upper lid and 10–20 in the lower lid. They produce tears for the surface of the conjunctiva.
Wolfring’s or Ciaccio’s glands (2–5 in number) are found along the superior tarsal border of the upper eyelid.
Popov’s glands are located within the substance of the caruncle.
The lacrimal glands produce only the aqueous part of tear film. Two additional components are present:
The outer lipid layer is produced by the meibomian glands, which form excavations within the tarsus and open at the eyelid margin, and by minor contributions from the glands of Zeis and Moll of the eyelash (follicle).
The inner mucin layer is made by the conjunctival goblet cells.
The arterial supply of the lacrimal gland is primarily from the lacrimal artery with smaller contributions from the recurrent meningeal artery and a branch of the infraorbital artery. The blood is drained by the lacrimal vein, an afferent vein of the superior ophthalmic vein.
The lacrimal gland receives innervations from cranial nerve V, parasympathetic fibers, and sympathetic ones from the superior cervical ganglion (Fig. 1.6) [6].
Fig. 1.6
Innervation of the lacrimal gland (sensory fibers, parasympathetic fibers, sympathetic fibers)
Sensory stimuli are carried by the lacrimal gland of the ophthalmic division of the trigeminal nerve.
Preganglionic parasympathetic secretomotor fibers originate in the lacrimal nucleus of the pons; they synapse in the sphenopalatine ganglion. Here, postganglionic fibers form the sphenopalatine nerve that reaches the gland.
Sympathetic stimulation derives from the sympathetic center of the thoracic cords and appears to have little effect on tear secretion but does act to adjust blood flow in the arterioles of the gland.
1.3.2 Eyelids
The primary function of the eyelid is the protection of the eye, but eyelids also contribute to the lacrimal pump, and their blinking action helps eliminate tears from the lacrimal lake.
The eyelids are divided into anterior and posterior lamellae separated by a multilayered septum. The anterior lamella includes skin and orbicularis oculi muscle. The posterior lamella includes the tarsus and the attachment and the conjunctiva.
Also in the eyelid margins, it is possible to distinguish (Fig. 1.7):
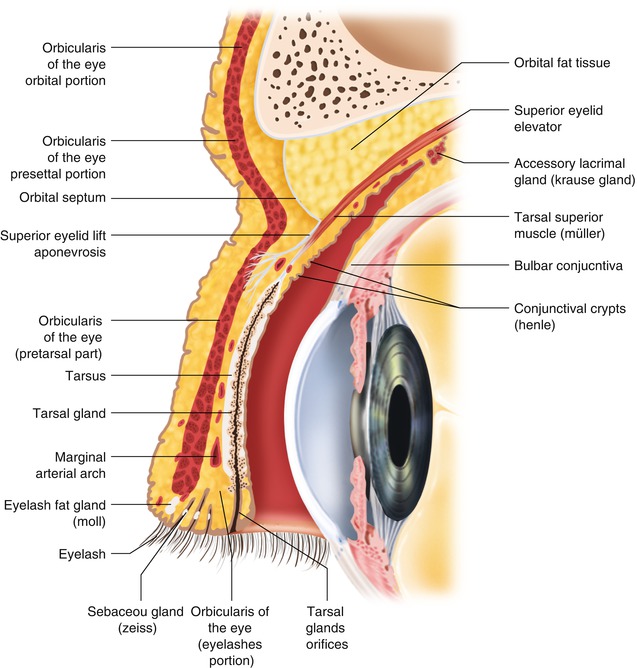
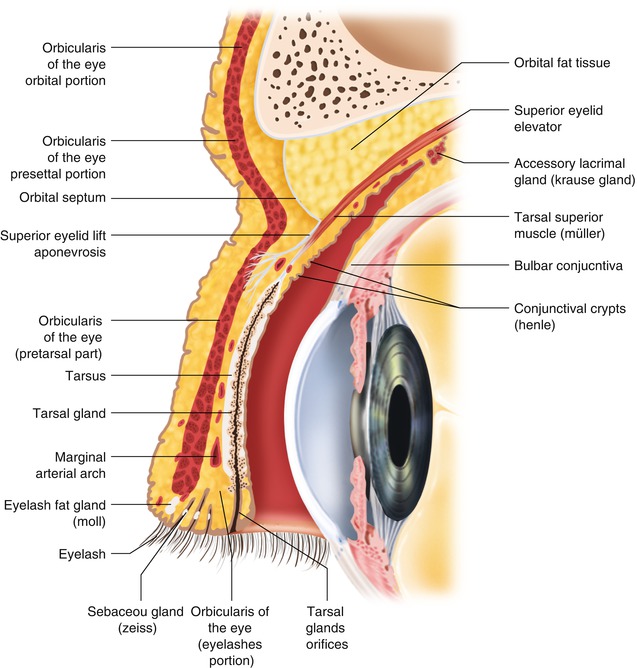
Fig. 1.7
Structure of the eyelid
The anterior part that is the site of origin of cilia and in which Zeis’ and Moll’s gland are situated. Behind them, there is the gray line corresponding to the pretarsal portion of the orbicularis muscle.
The posterior part formed by the tarsal plate that provides the structural framework of the eyelid. It is composed of condensed fibrous and elastic tissue but contains no cartilage. Meibomian glands are present at that level. Behind, tarsus bulbar conjunctiva is present.
Different muscles allow eyelid movements:
Tendon of the levator palpebral muscle, inserted in the anterior tarsal margin, and superior tarsalis muscle, inserted into the superior tarsalis margin, contribute to the upper eyelid elevation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









