Chapter 91B Vascular reconstruction techniques
Overview
Improvements in our understanding of the anatomy and function of the liver, expertise stemming from liver transplantation, and the advances of hepatic imaging have allowed extension of the surgical limits in the area of hepatic resection. Extensive liver resection for malignant tumors, which requires a sufficient functional liver remnant volume for patient recovery, may be performed with concomitant vascular reconstruction to ensure oncologically adequate resection and adequate liver function (see Chapter 94). Parenchymal resection can be performed with caval, portal, and, exceptionally, arterial resection to improve resectability of many tumor types. Hepatic vein (HV) reconstruction has been more recently emphasized for improving postoperative liver function and regeneration.
Vena Cava and Hepatic Vein Resection
Complete Obstruction of the Inferior Vena Cava
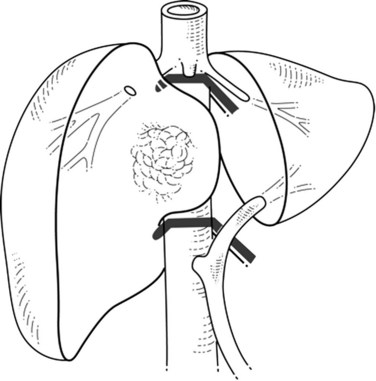
When liver tumor is associated with complete inferior vena cava (IVC) obstruction, collateral circulation usually provides sufficient venous drainage (Fig. 91B.1), therefore obstruction symptoms, such as edema of the lower extremity, are uncommon. Leiomyosarcoma of the retrohepatic IVC is the main etiology of a complete obstruction of the IVC. In this situation, liver resection with concomitant IVC resection is appropriate, providing preservation of the collaterals can be performed without restoration of caval flow. IVC replacement is considered in patients who have poor development of collateral circulation and in those who require wide retroperitoneal resection for lymph node dissection, which can disrupt preexisting venous channels and reduce collateral venous return (Beck & Lalka, 1998; Yoshidome et al, 2005).
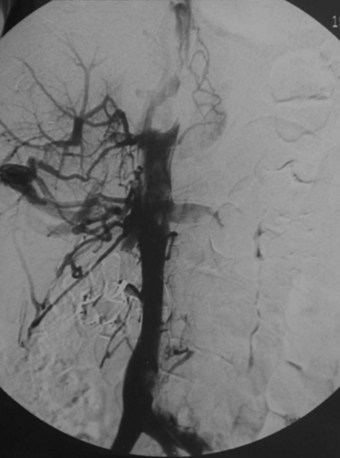
FIGURE 91B.1 Complete obstruction of the inferior vena cava with development of collateral circulation.
After IVC resection, lower-limb venous thrombosis occurs in about 25% of patients, and reduction of the collateral circulation may increase this risk (Mingoli et al, 1991). After caval flow interruption, postoperative renal dysfunction occurs in 0% to 40% (Daylami et al, 2010). Because the left renal vein has multiple collateral venous developments—gonadal, adrenal, and lumbar—ligation of the left renal vein is not deleterious (Griffin & Sterchi, 1987); however, the right renal vein has few collateral venous systems, and its ligation can be harmful and often necessitates reimplantation into the IVC or into the left renal vein.
Partial Obstruction of the Inferior Vena Cava
Colorectal liver metastasis and intrahepatic cholangiocarcinoma (see Chapters 50A and 81A), which are best treated by R0 resection, may involve the IVC. Preoperative morphologic assessments are generally inaccurate to differentiate malignant infiltration of the vena cava wall from a simple tumoral adhesion; therefore concomitant hepatic and IVC/HV resection should be considered when tumor involvement of the IVC or the venous confluence is suspected. Invasion of the vena wall is found in 22% to 72% of patients and can be assessed intraoperatively by palpation, ultrasonography, or even by intravascular ultrasonography (Azoulay et al, 2006; Hemming et al, 2002; Kaneko et al, 1996; Kikumori et al, 2003). Experience in living donor liver transplantation (LDLT) has shown that congestion of the remnant liver territory is underestimated (Scatton et al, 2008). Impairment of venous outflow of the remnant liver has deleterious consequences on postoperative liver function and regeneration, emphasizing the need for reconstruction of the corresponding draining HV, especially when the volume of the remnant liver is marginal (Nakamura et al, 1990). In addition, maintaining the normal anatomy of the hepatic veins in the remnant liver may be beneficial to preserve the possibility of repeat hepatectomy for tumor recurrence, particularly in patients resected for colorectal liver metastasis (Pessaux et al, 2006).
Many studies report the technical aspects of vascular resection with hepatectomy, but few report the long-term results with survival rate. Venous involvement is a poor prognostic factor, but given the poor results of nonsurgical treatment, aggressive surgical resection that includes major vascular resection offers the best results in selected patients (Aoki et al, 2004; Miyazaki et al, 1999).
Hepatocellular carcinoma (HCC) has a strong propensity for vascular invasion and direct intravascular extension (see Chapter 80). Autopsy series report IVC involvement from 9% to 26% and right atrium involvement from 2.4% to 6.3% (Sung et al, 2008). Most patients are seen initially with symptoms of portal hypertension or right-sided heart failure (diuretic-resistant lower extremity edema). Efficient treatment requires liver parenchymal resection associated with vascular resection and thrombectomy under vascular exclusion (see Chapter 91A). This procedure, which requires expertise in both vascular and liver surgery, usually includes simultaneous hepatectomy and thrombectomy under vascular exclusion (Sung et al, 2008). Major bleeding and difficult vascular reconstruction are associated with the risk of thrombus migration into pulmonary arteries (Shirabe et al, 2001). When tumor thrombus extends to the right atrium, liver resection associated with cardiopulmonary bypass should be considered.
Resection
According to the extent and location of the IVC involvement, various approaches, including thoracoabdominal access, have been described (Torzilli et al, 2007). Because complete mobilization of the liver could be hazardous, an anterior approach to the IVC can be performed (Liu et al, 2000). After extrahepatic control of the IVC below and in the upper liver, the anterior approach includes initial liver resection toward the IVC.
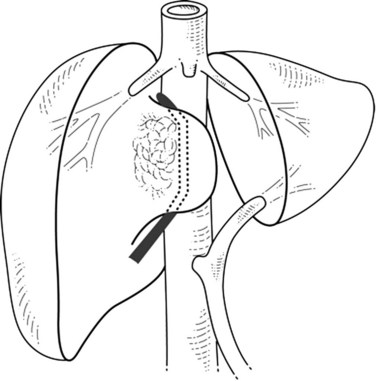
If the portion of the IVC involved by the tumor is below the hepatic veins, the hepatic parenchyma is divided using intermittent inflow occlusion if necessary (Belghiti et al, 1999). Once the IVC is exposed, portal inflow occlusion is released if used, the patient is volume loaded, and clamps are placed above and below the area of tumor involvement (Fig. 91B.2; see Chapter 91A). This caval clamping allows resection of the portion of the liver involved by tumor with the portion of vena cava involved by tumor, followed by partial or total reconstruction of the IVC. Positioning the clamps below the hepatic veins allows perfusion of the remnant liver and minimizes ischemic time.
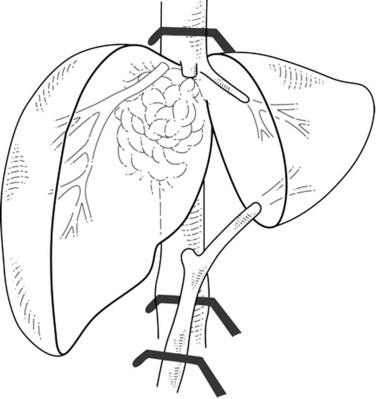
In cases of lateral IVC involvement, a single clamp may be applied tangentially to the IVC to preserve a vena caval flow (Fig. 91B.3), but this procedure is not applicable when the tumor involves the whole hepatocaval confluence. In such cases, are two different approaches may be applied. The first one includes a total vascular exclusion of the liver with subsequent infrahepatic IVC, pedicular, and suprahepatic IVC clamping (Fig. 91B.4; see Chapter 91A). Total vascular exclusion induces a decrease of 40% to 50% in the cardiac index and may be not well tolerated in some patients (Azoulay et al, 2006; Hemming et al, 2004). The second one includes use of an active venovenous bypass between the portal and axillary vein and between IVC and axillary vein can also be used (Azoulay et al, 2006; Hemming et al, 2004). When a biopump is used, in situ hypothermic perfusion of the liver parenchyma can be added to prevent postoperative liver failure as a result of prolonged ischemia (Azoulay et al, 2006; Hemming et al, 2004; see Chapter 94).
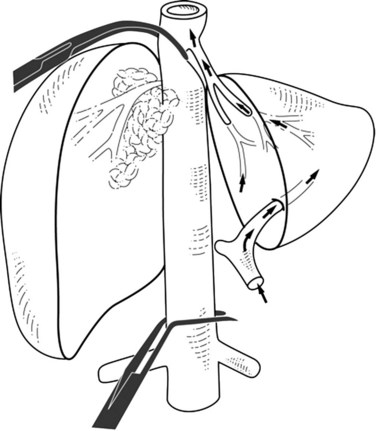
Extrahepatic control of the IVC can be attained without using total hepatic vascular exclusion (Varma et al, 2007). The suprahepatic IVC is taped just below the diaphragm, the common trunk of the left and middle hepatic veins is dissected, and a previously deployed suprahepatic tape is rotated to the right side between the vena cava and common trunk; this isolates the right hepatocaval confluence and juxtahepatic vena cava, leaving the common trunk and the rest of IVC free. The infrahepatic IVC is clamped, and concerning the suprahepatic IVC, a clamp is placed obliquely to occlude the right hepatocaval confluence and juxtahepatic vena cava (Fig. 91B.5). When right the hepatocaval junction is uninvolved, this procedure can be used in patients with left-sided neoplasms by reversing the caval tape to the left side (Maeba et al, 2001). The remnant liver receives complete inflow with uninterrupted outflow through the uninvolved hepatocaval confluence, the patency of which is maintained. This technique may also be used when synchronous involvement of the IVC and any one of the hepatocaval confluences is apparent, with at least one HV being free of tumor. This procedure has the potential disadvantage of incomplete vascular control during parenchymal transection in the presence of large veins from the caudate lobe, which leads to backflow venous bleeding. This problem can be overcome by associated resection of segment I.
Advances in liver transplantation techniques have allowed expansion of the ex vivo procedure in selected resections (see Chapter 94). This challenging technical procedure, described by Pichlmayr and colleagues (1988), is seldom performed (Hemming & Cattrall, 1999; Miyazaki et al, 2007b; Yanaga et al, 1993
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree