Chapter 76C Distal splenorenal shunt
Background
The distal splenorenal shunt (DSRS) was developed by Warren and colleagues in 1967 to achieve selective variceal decompression to prevent recurrent variceal bleeding. Selective variceal decompression combines the benefit of a decompressive shunt to control bleeding with maintenance of portal hypertension and portal flow to the cirrhotic liver to help maintain liver function. The original, classic article on selective variceal decompression described the animal work leading up to the initial clinical data on DSRS (Warren et al, 1967). Proof of concept was shown in the animal studies and in the results of the first six patients in whom DSRS was performed. The unique prior experiences of Warren and Zeppa led to the evolution of this concept: Warren had seen that total shunts control variceal bleeding, but at the cost of liver failure, whereas Zeppa had seen devascularization procedures maintain portal perfusion, but at a cost of significant risk of rebleeding.
Over the next 4 decades, DSRS became the most widely used operation to control variceal bleeding, with a worldwide following (Orozco et al, 2007). The technique continued to evolve, with greater degrees of portal azygos disconnection improving its effectiveness (Henderson et al, 1989). However, in the 1990s, the evolution of improved endoscopic therapy with banding (see Chapter 75B), introduction of transjugular intrahepatic portosystemic shunting (TIPS; see Chapter 76E), and coming of age of liver transplantation (see Chapter 97A, Chapter 97B, Chapter 97C, Chapter 97D, Chapter 97E ) left few indications for shunt surgery for variceal bleeding (see Chapter 76A).
Indications for DSRS
• Patients with variceal bleeding refractory to endoscopic and pharmacologic therapy who have well-preserved and stable liver function
• Patients with portal hypertension and normal livers, such as those with portal vein thrombosis, who have refractory bleeding and a patent splenic vein
• Patients in some geographic locations, where there is only one chance to control bleeding, and they cannot return for the multiple visits required for management with endoscopy or TIPS
Patient Evaluation
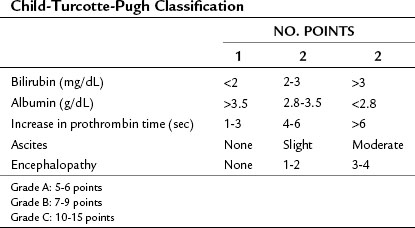
Liver function is assessed from clinical findings and laboratory studies. Jaundice, ascites, and encephalopathy are the three clinical signs and symptoms of advanced liver disease and indicate that patients are not candidates for surgical decompression. Laboratory measurements of serum bilirubin, albumin, serum creatinine, and prothrombin time prolongation are the most useful studies to assess the status of cirrhosis. Combining the clinical and laboratory parameters to discern the Child-Turcotte-Pugh (CTP) class and/or Model for End-Stage Liver Disease (MELD) score gives an objective assessment of risk (Table 76C.1 and Box 76C.1).
Box 76C.1 Model for End-Stage Liver Disease Score for Liver Disease Severity
Score = 0.957 × loge creatinine (mg/dL) + 0.378 × loge bilirubin (mg/dL) +1.120 loge INR
1 Hepatic venous pressure gradient (HVPG)
2 Left renal vein anatomy and drainage (this is abnormal in 20% of the population)
3 Superior mesenteric, portal, and splenic vein patency, flow direction, and venous anatomy on the venous phase of the arterial study
4 Major variceal inflow paths on the same study as in number 3 above
Technique for Distal Splenorenal Shunt
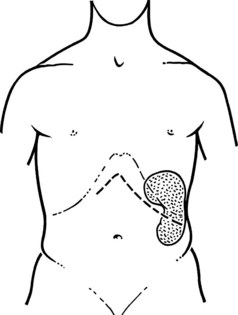
The steps in DSRS are illustrated. The preferred incision is a long left subcostal incision, extended across the right rectus muscle (Fig. 76C.1). Coagulating diathermy should be used extensively in patients with portal hypertension to achieve hemostasis in dividing tissues. If present, ascites should be aspirated and cultured, and a liver biopsy specimen should be obtained to document the status of the liver at the time of the procedure.