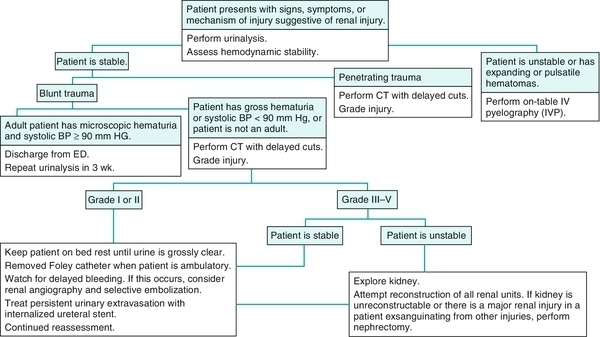
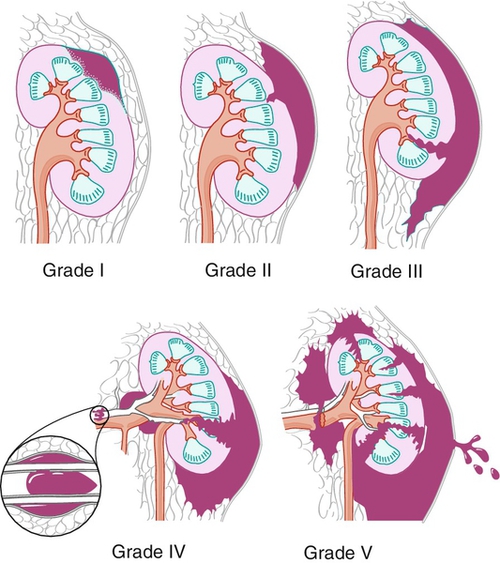
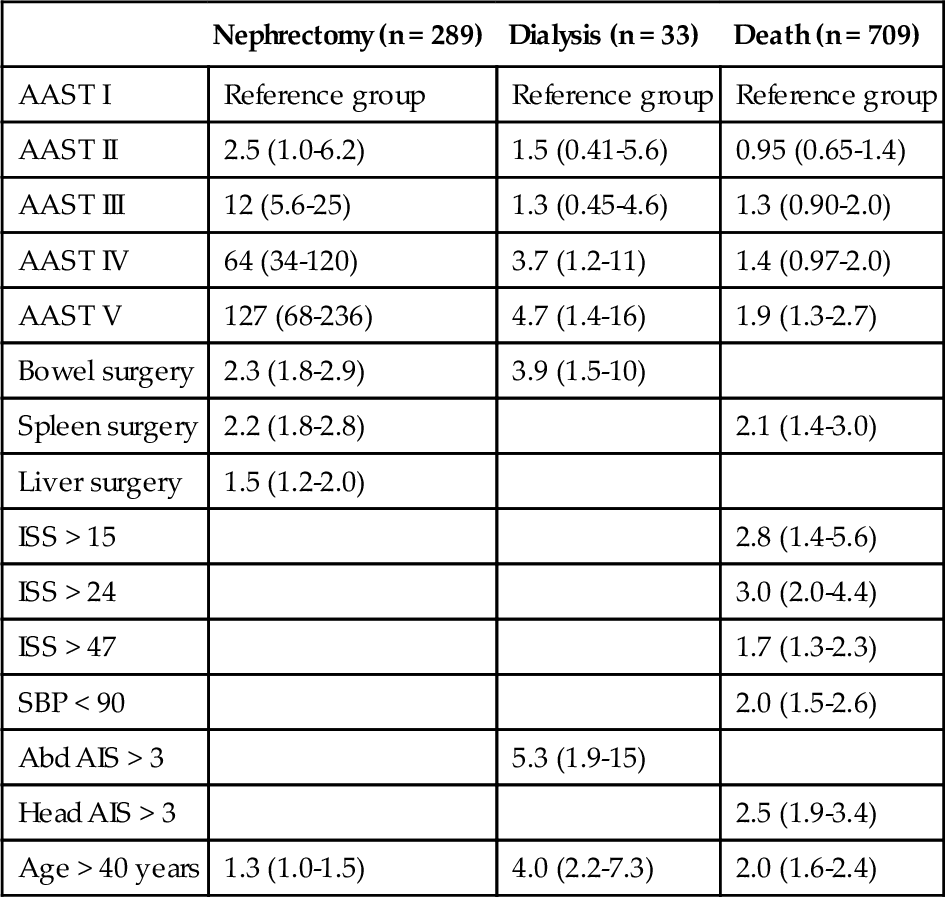
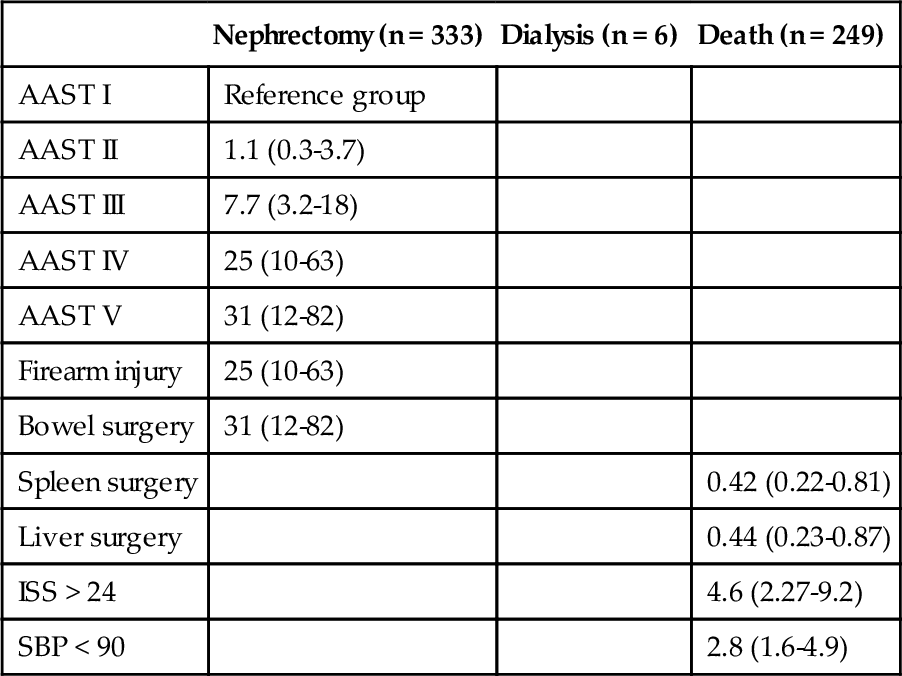
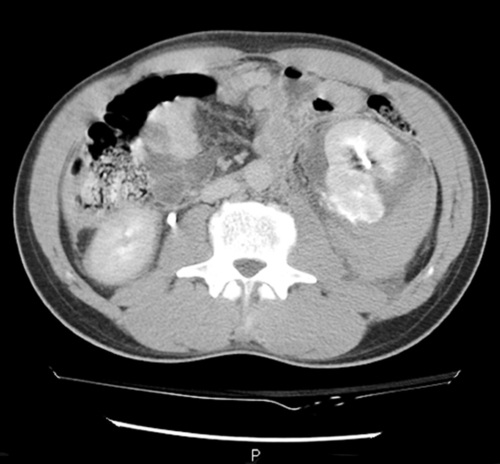
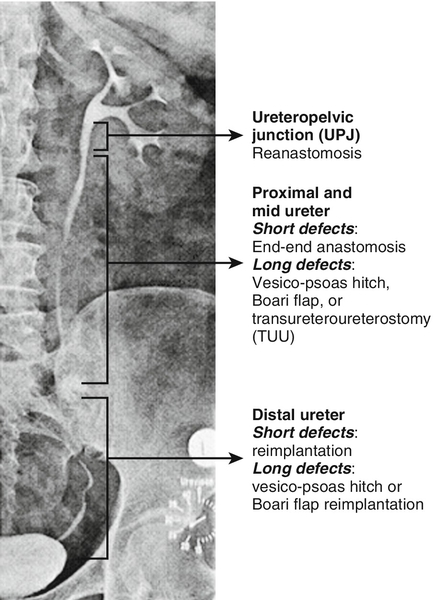
Chapter 10 Robert C. Kovell, MD; Jonathan L. Wright, MD, MS, FACS; Hunter Wessells, MD, FACS Trauma remains the leading cause of death among young persons, and disability far exceeds mortality. Injuries are responsible for 8% of global mortality and 13% of global disability adjusted life years. One out of every 14 deaths in the United States is the result of trauma, and genitourinary injuries occur in approximately 10% of all trauma cases. Whereas kidney injuries cause acute hemorrhage and can be immediately life threatening, lower urinary tract and genital trauma may lead to lifelong disability and impaired quality of life. Renal injuries, occurring in 1% to 5% of all trauma patients, are the most commonly observed genitourinary injuries. Advances in radiographic imaging, trauma care, and endovascular modalities have allowed significantly more renal traumas to be managed nonoperatively. After stabilization, gross inspection of the urine and urinalysis should be performed because hematuria is often an early indicator of renal trauma. Any trauma patient presenting with hematuria must be evaluated for renal injury (Figure 10-1). However, the degree of hematuria correlates poorly with renal injury severity. Patients with renal artery thrombosis, ureteropelvic junction (UPJ) disruption, or renal pedicle avulsion may not have hematuria. A high degree of suspicion for renal trauma is required for patients who do not meet the hematuria criteria for imaging but who have experienced a fall from a height, a high-speed motor accident, or a direct blow to the flank. Patients with preexisting renal abnormalities are also at higher risk for traumatic renal injury. Hemodynamically stable patients with suspected renal injury and clinical indications such as blunt trauma with gross hematuria, microscopic hematuria associated with shock, rapid deceleration injuries, major associated injuries, or penetrating trauma to the abdomen, flank, or lower thorax should undergo prompt imaging. Stable patients with microscopic hematuria and no reported hypotension can be observed clinically without renal imaging. For most renal trauma patients, the imaging modality of choice is contrast-enhanced computed tomography (CT) to identify active arterial bleeding and parenchymal lacerations followed by a 10- to 15-minute delayed excretory phase to identify urinary contrast extravasation. Hemodynamically unstable patients often require emergent stabilization and/or laparotomy. If the patient requires immediate laparotomy, on-table, one-shot intravenous urography (IVU) can provide useful information (see Management section). Angiography may be useful where selective embolization is considered. The American Association for the Surgery of Trauma (AAST) Organ Injury Scale is widely used to classify blunt and penetrating renal injuries based on either direct operative exploration or CT scan appearance (Figure 10-2). Multiple studies have shown that increasing AAST score correlates with increasing morbidity (need for nephrectomy, renorrhaphy, dialysis) and mortality (Tables 10-1 and 10-2). Table 10-1 Multivariate Predictors of Morbidity and Mortality for Blunt Renal Trauma* AAST, American Association for the Surgery of Trauma; AIS, Abbreviated Injury Scale; ISS, injury severity score; SBP, systolic blood pressure. ⁎ Blank cells indicate the parameter was not an independent predictor for that particular outcome. Table 10-2 Multivariate Predictors of Morbidity and Mortality for Penetrating Renal Trauma* AAST, American Association for the Surgery of Trauma; ISS, injury severity score; SBP, systolic blood pressure. ⁎ Blank cells indicate the parameter was not an independent predictor for that particular outcome. There were too few patients with dialysis (n = 6) for a meaningful prediction model. Increasingly, renal trauma management is nonoperative with multiple series showing successful renal preservation despite high-grade injury. Nonoperative therapy has a low failure rate and a lower rate of nephrectomy than immediate operative management. The absolute indications for operative exploration in renal trauma include hemodynamic instability, life-threatening hemorrhage, pedicle avulsion, or an expanding, pulsatile, or uncontained retroperitoneal hematoma. Complications that once required open surgery can often be managed nonsurgically: Active arterial bleeding and arterial pseudoaneurysms are controlled with selective angioembolization, and perinephric abscesses and urinomas can be treated with percutaneous drainage and/or indwelling ureteral stents. Currently, 20% to 50% of all penetrating renal injuries and fewer than 10% of blunt injuries require operative management. Grade I-III renal injuries, regardless of mechanism, are generally managed with observation alone. In hemodynamically stable patients, many grade IV (Figures 10-3 and 10-4) and selected grade V injuries can be managed nonoperatively with close monitoring, hydration, serial hematocrit measurement, and repeat imaging with a high success rate. Patients are kept on bed rest until the urine is grossly clear. Foley catheter drainage is necessary only until other injuries are stable and the patient can void spontaneously. Thrombosis of the renal artery or its branches is treated nonoperatively unless the contralateral kidney is absent or severely injured, in which case emergency revascularization is indicated. Renal exploration often leads to nephrectomy, either as damage control in the exsanguinating patient or unnecessarily by surgeons unfamiliar with renal reconstructive techniques. Other predictors of nephrectomy include the AAST renal injury scale, the Injury Severity Score (ISS), transfusion requirements, and operations on other intraabdominal organs. A significant number of patients with a penetrating injury and a minority of those with blunt trauma require immediate laparotomy before radiographic evaluation. If a major renal injury is suspected based on the size of the perinephric hematoma, a one-shot intraoperative IVU is recommended before renal exploration to confirm the presence of a contralateral functioning kidney and potentially to rule out major injury. A 2 mL/kg bolus of contrast material is administered 10 minutes before obtaining a single plain abdominal film. Abnormalities of the affected kidney, including poor visualization, require operative exploration. In the critically ill patient with multiple injuries, renal exploration is indicated if a pulsatile or expanding hematoma is present, in which case a rapid nephrectomy is often necessary. Less severe injuries can be managed with renorrhaphy, partial nephrectomy, perinephric drains, embolization, and damage control techniques described later. In most cases, renal reconstruction and salvage is possible; however, if the patient is unstable and has a normal contralateral kidney, rapid nephrectomy may be prudent. Selective renal embolization via angiography may be considered when no other injury requires immediate surgical exploration and conservative measures have failed to control hemorrhage. This strategy has demonstrated high success rates and low complication rates for grade IV injuries but often fails for grade V injuries. Operative management of grade III and IV injuries consists of hemorrhage control first, followed by repair of the collecting system and parenchymal closure. In blunt grade V injuries requiring exploration, nephrectomy is almost always the preferred treatment except in solitary kidneys or bilateral renal injuries. A midline transabdominal incision permits exploration of the kidneys, allows complete inspection of the intraabdominal contents, and provides optimal access to the renal hilum. Isolation of the renal artery and vein is recommended and should be achieved by opening the posterior peritoneum medial to the inferior mesenteric vein or by reflecting the ipsilateral colon (provided that the perinephric hematoma is left undisturbed). Early vascular control appears to increase the rate of renal salvage. Once the renal vessels are isolated, Gerota fascia is opened. If massive bleeding occurs when the hematoma is entered, Rummel tourniquets or vascular clamps are applied to the renal artery and vein. The principles of renal reconstruction include complete exposure, debridement of devitalized tissue, achievement of hemostasis, watertight collecting-system closure, coverage of the defect, and drainage. Bleeding points must be controlled using figure of eight sutures of fine absorbable monofilament. Once hemostasis is satisfactory, collecting-system openings are closed with 4-0 absorbable sutures. The defect in the parenchyma can be filled with folded absorbable gelatin sponges as the capsule is closed over the bolsters. For polar injuries, partial nephrectomy can be considered instead. The addition of hemostatic agents such as Floseal may also be helpful. If the renal capsule has been destroyed, coverage options include an omental or perinephric fat flap, a patch of polyglycolic acid or peritoneum, or an entire sac of polyglycolic acid wrapped around the kidney, with the parenchymal edges kept well apposed. Gerota fascia is not reapproximated. Closed-suction drainage of the ipsilateral retroperitoneum is recommended. Internalized stents are reserved for complex injuries (e.g., large lacerations of the renal pelvis or the UPJ). Prompt nephrectomy is generally advised in the rare case of major renovascular injuries because salvage rates after renal vascular reconstruction are low. In unstable patients, damage control with renal packing and planned reevaluation in 24 hours can also be considered in an attempt to avoid nephrectomy. The risk of complications increases with each increasing grade of renal injury. The most significant early complications are delayed bleeding, infection, and urinary leakage. For grade IV-V injuries managed nonoperatively, follow-up imaging at 48 to 96 hours after the initial scan minimizes the risk of missed complications. For lower grade injuries, repeat imaging can be safely omitted unless signs of infection, decreasing hematocrit, persistent hematuria, and persistent flank plan are present. Urinary extravasation can often be managed with systemic antibiotics and close observation. If the extravasation persists, internalized ureteral stenting is indicated, especially in the setting of obstruction or infection. The urinary bladder should be drained with a Foley catheter until any extravasation resolves, which can take days to weeks. Ultrasonography is useful for following such collections and for reducing the patient’s radiation exposure. If the perinephric fluid collection is large enough to compress the ureter or becomes infected, additional percutaneous drainage is required. Delayed bleeding is a rare, life-threatening complication of major lacerations. Pseudoaneurysm formation and arteriovenous malformation (AVM) are the most common causes of delayed bleeding and usually occur within 2 weeks post injury. Selective arterial embolization is an effective treatment in most instances. Hypertension is a rare late complication of renal injuries that is usually renin mediated from an ischemic segment of parenchyma. This occurs in about 5% of renal trauma patients. Etiologies include renal arterial injury leading to stenosis, extrinsic compression from urinary or blood extravasation (Page kidney), an ischemic parenchymal fragment, or arteriovenous fistula. Angiography, decortication, excision of the nonperfused segment, or nephrectomy may be required in these rare cases. Long-term blood pressure monitoring is often necessary. Most ureteral injuries are iatrogenic, primarily resulting from gynecologic, general surgical, or urologic procedures. External ureteral trauma is relatively rare, accounting for approximately 1% of all genitourinary injuries. Ureteral injuries more commonly occur with penetrating trauma and deceleration injuries, and patients usually have multiple associated abdominal injuries. Patients with ureteral injuries have a mortality rate of 6% to 10% as a result of associated injuries, which reflect the penetrating trauma and high-velocity motor vehicle crash mechanisms. A high index of suspicion is thus necessary to prevent a delay in diagnosis with resultant late consequences such as urinoma, sepsis, stricture, and nephrectomy. Hematuria may be absent in 25% to 45% of patients with ureteral injury, which contributes to a delay in diagnosis. Stable patients with suspected ureteral injuries should undergo CT with intravenous contrast and delayed images to evaluate for urinary extravasation. If further clinical information is needed, retrograde pyeloureterography can be used to more accurately define the extent of the injury (Figure 10-5). Ureteral injury at the UPJ or near the iliac vessels can occur after severe deceleration or ejection from a high-speed vehicle, particularly in children, in whom the hyperextensibility of the spine leads to UPJ avulsion. Medial or circumrenal contrast extravasation on CT scan should raise suspicion for UPJ disruption. Unstable patients taken to the operating room without imaging can be evaluated intraoperatively with a one-shot IVU, although this proves nondiagnostic for ureteral injuries in 33% to 100% of cases. Indications for exploration include a retroperitoneal hematoma and a projectile trajectory that put the ureter at risk. In meta-analysis from 16 large trauma centers, 89% of ureteral injuries were identified at the time of exploratory laparotomy. Gentle instillation of 1-2 mL of methylene blue or indigo carmine into the collecting system may help to identify sites of laceration or avulsion. Management depends on the degree of injury, the location of the ureteral injury (Figure 10-6), and the timing of diagnosis. Injuries recognized initially should be surgically repaired. If a patient is not stable, ligation of the ureter and nephrostomy tube drainage or exteriorization of a ureteral stent allows elective repair at a later time. If diagnosis is delayed, percutaneous nephrostomy and ureteral stenting, followed by delayed definitive management, avoids the risk of nephrectomy associated with operative exploration. Nephrectomy should be considered in cases where concomitant vascular repair using prosthetic material may be complicated by urine leakage.
Urinary and Genital Trauma
Introduction
Kidney injuries
Initial evaluation
Classification
Nephrectomy (n = 289)
Dialysis (n = 33)
Death (n = 709)
AAST I
Reference group
Reference group
Reference group
AAST II
2.5 (1.0-6.2)
1.5 (0.41-5.6)
0.95 (0.65-1.4)
AAST III
12 (5.6-25)
1.3 (0.45-4.6)
1.3 (0.90-2.0)
AAST IV
64 (34-120)
3.7 (1.2-11)
1.4 (0.97-2.0)
AAST V
127 (68-236)
4.7 (1.4-16)
1.9 (1.3-2.7)
Bowel surgery
2.3 (1.8-2.9)
3.9 (1.5-10)
Spleen surgery
2.2 (1.8-2.8)
2.1 (1.4-3.0)
Liver surgery
1.5 (1.2-2.0)
ISS > 15
2.8 (1.4-5.6)
ISS > 24
3.0 (2.0-4.4)
ISS > 47
1.7 (1.3-2.3)
SBP < 90
2.0 (1.5-2.6)
Abd AIS > 3
5.3 (1.9-15)
Head AIS > 3
2.5 (1.9-3.4)
Age > 40 years
1.3 (1.0-1.5)
4.0 (2.2-7.3)
2.0 (1.6-2.4)
Nephrectomy (n = 333)
Dialysis (n = 6)
Death (n = 249)
AAST I
Reference group
AAST II
1.1 (0.3-3.7)
AAST III
7.7 (3.2-18)
AAST IV
25 (10-63)
AAST V
31 (12-82)
Firearm injury
25 (10-63)
Bowel surgery
31 (12-82)
Spleen surgery
0.42 (0.22-0.81)
Liver surgery
0.44 (0.23-0.87)
ISS > 24
4.6 (2.27-9.2)
SBP < 90
2.8 (1.6-4.9)
Management

Operative management
Complications
Ureteral injuries
Initial evaluation

Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



