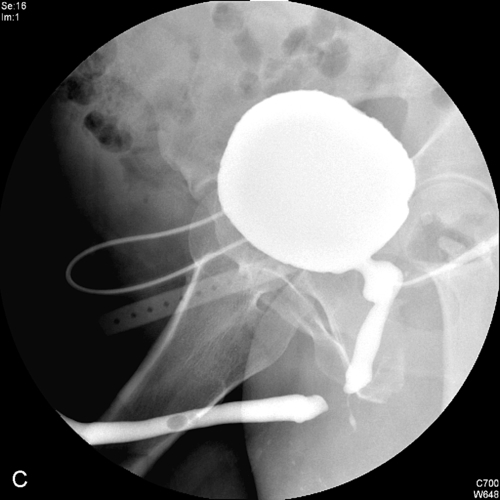
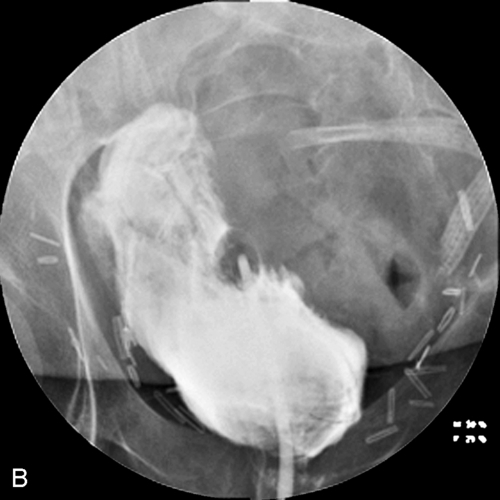
Chapter 2 The imaging technique used to evaluate the urinary tract is dictated by the indication for which the diagnostic evaluation is being performed. Modalities currently in use include conventional abdominal plain-film radiography, ultrasonography (US), computed tomography (CT), magnetic resonance imaging (MRI), radionuclide studies, and newer techniques such as positron emission tomography (PET). In this chapter, the role of these different imaging modalities in the management of patients will be addressed. X-ray films are rarely used in the developed world, having been entirely replaced by digital imaging in the United States and much of the west. Computed radiograph of the abdomen is one term used for an x-ray examination of the abdomen (KUB — kidney ureters, and bladder) performed without intravenous contrast, although it is inaccurate as a digital image is technically not a radiograph. Radiation exposure for an abdominal radiograph is low and is approximately 0.53 millisieverts (mSv). For comparison purposes, radiation exposure from natural background radiation is about 3 mSv per year. The primary indication for a radiograph of the abdomen is to assess for the presence of radiopaque calculi, assess the results of therapy for such calculi (shockwave lithotripsy or percutaneous techniques), and evaluate urinary stents for their position and complications such as encrustation. As bowel content overlies the renal fossae in a patient who has not received a laxative preparation (the usual situation for a plain radiograph), small or faintly opaque stones may be hard to identify through the overlying bowel. The identification of calculi overlying the bony pelvis may also pose a challenge. Oblique images are often helpful in problem solving in such cases because the obliquity allows the kidney or ureter to be rotated off of the overlying bowel or bone and thus allow small calculi to become visible. The intravenous urogram (IVU), also referred to as excretory urogram (EU) or intravenous pyelogram (IVP), was the basic diagnostic radiologic study to evaluate the upper urinary tract for many decades. Its role in the assessment of many urologic conditions is now very limited due to the advantages offered by cross-sectional imaging modalities. IVU requires intravenous injection of radiographic contrast medium, followed by a sequence of films. Radiation exposure for an IVU (6 images) is approximately 2.5 mSv. 1. Hematuria (macroscopic and microscopic) 2. Upper urinary tract surveillance in patients with a history of a urothelial malignancy, such as bladder cancer, or positive urine cytology (Figure 2-3) 3. Preoperative evaluation for select endourological procedures such as endopyelotomy 4. Postoperative evaluation following urologic procedures (Figure 2-4) 5. Complicated or unusual urinary tract infections (including tuberculosis) 6. Stone disease Radiographic contrast media (CM) consist of three atoms of iodine attached to a benzene ring. In the developed world, newer nonionic agents that are either of low osmolarity (LOCM — low-osmolarity contrast medium) or of iso-osmolarity, are used for intravascular administration. Contrast agents used in the past were of high osmolarity (HOCM) and are referred to as ionic contrast agents. Multiple studies have shown that the frequency of reactions is lower with the LOCM as compared to the HOCM when given intravenously in both the general population and in patients at higher risk for contrast reaction. The majority of injected contrast is excreted almost entirely by glomerular filtration. A small amount may be bound to serum albumin and is then excreted by the liver and biliary system and is known as vicarious excretion. Patients with renal insufficiency or obstruction frequently have vicarious excretion (Figure 2-5). 2. A plain film of the abdomen (also known as scout film, preliminary film, KUB film, abdominal flat plate) is obtained. 3. Contrast administration 4. Imaging sequence (Figure 2-6) 2. Relative contraindications a. Multiple consecutive contrast studies b. In patients with a documented allergic reaction to contrast such as urticaria (hives), cutaneous and subcutaneous edema (angioedema), upper airway (laryngeal) edema, bronchospasm, and hypotension with tachycardia, the indications for contrast administration should be carefully considered and other alternative studies performed, if possible. c. Patients at increased risk for adverse reactions include those with a history of prior contrast reactions (four times increased risk), or a history of allergies or asthma (two to three times increased risk) as compared to patients who do not have such histories. d. Multiple myeloma was long considered a risk factor for CIN with the cause believed to be precipitation of protein-contrast aggregates in the renal tubules. e. In patients with cardiac disease, contrast media administration can cause worsening of congestive heart failure due to the osmotic load. f. Patients who are on metformin, an oral hypoglycemic agent (trade names Glucophage, Glucovance, Avandamet, and Metaglip) should discontinue the drug when they receive contrast and not resume taking their medication until their renal function is documented to be normal 48 hours after the contrast administration. g. Delayed reactions, defined as those occurring more than 1 hour after contrast administration, can be seen with all contrast agents; they occur in 0.5% to 23% of patients and tend to be skin reactions. 2. To visualize the collecting systems and ureters when IVU is contraindicated (renal insufficiency or severe prior contrast reaction) 3. To demonstrate the collecting systems and ureters in their entirety when IVU or CTU fail to do so 4. To visualize the ureteral stump remaining after nephrectomy in a patient with hematuria, positive urinary cytology or history of urothelial cancer. 2. Patients who cannot or should not be cystoscoped (e.g., patients recovering from recent bladder or urethral surgery) 1. Preliminary cystoscopy is required. 2. A ureteral orifice is identified and catheterized with a catheter, usually 5 French in size. The catheter is advanced to the renal pelvis, and contrast is instilled. The same contrast agents employed for IVU or CT are used for retrograde pyelography. To opacify the ureter alone, the ureteral orifice is occluded with a bulb occlusion catheter and contrast injected while a film is obtained. 3. Images — a preliminary image is essential to document the position of the retrograde catheters. After contrast injection, fluoroscopic images are obtained to delineate unopacified or poorly seen portions of the collecting system or ureter in question. If obstruction is suspected, an image is also obtained several minutes after removal of the ureteral catheter to evaluate the drainage of the collecting system (Figure 2-7). 4. The use of fluoroscopy is an important adjunct to Retrograde pyeloureterography (RPG). In most hospital settings, however, this requires the placement of a ureteral catheter in the cystoscopy suite and the subsequent transport of the patient to the radiology department for catheter injection. 5. RPG may be impossible in some patients, such as those with very larger prostates, in whom the gland overlies the ureteral orifices, preventing proper catheter placement. At times, even though the orifice is identifiable, it may not be possible to catheterize it, such as may occur with tortuous ureters or after ureteral reimplantation in a native system or a renal transplant. 6. Radiation exposure with all fluoroscopic procedures varies with the equipment, size, and body habitus of patient, fluoroscopy times, and factors such as collimation and distance between x-ray source and the patient. 2. A too vigorous injection of contrast material in an infected urinary tract may disseminate bacteria into the bloodstream and kidney, causing bacteremia and rarely pyelonephritis. This risk increases in the presence of a urinary tract obstruction. Fortunately, the normal antegrade flow of urine is usually enough to wash out any bacteria that may have been introduced during the procedure. Patients usually receive prophylactic periprocedural antibiotics as well. 3. Absorption of contrast agent can occur if there is perforation of the collecting system or pyelosinus extravasation due to overdistention. In patients truly allergic to contrast media, the retrograde approach does not obviate a systemic contrast reaction, although reactions are much less common than after IV injection. Patients with a history of contrast allergy should receive premedication with corticosteroids and antihistamines. 2. In patients with a history of urothelial malignancy and high-grade obstruction of a collecting system, an antegrade pyelogram may be the only way to evaluate the urothelium of the collecting system and ureter. Contrast excretion in an obstructed system is impaired, and thus intravenous contrast administration for either an IVU or CTU will not depict the collecting system well enough to exclude upper urinary-tract urothelial lesions. 3. In patients with renal transplants who have azotemia in association with a dilated collecting system, antegrade pyelogram can help determine whether the transplant collecting system is obstructed or not. The ureteroneocystostomy created to drain a renal transplant is often difficult to cannulate cystoscopically. Bleeding diathesis The renal pelvis is percutaneously punctured with a 20- or 21-gauge thin-walled needle from a posterior or posterolateral approach. Localization is provided by means of contrast excreted after an IV injection or with ultrasound in a dilated collecting system. Contrast is injected, and images are exposed under fluoroscopic control. These are similar to a percutaneous nephrostomy (PCN). 2. Some extravasation usually occurs with many antegrade pyelograms. However, the puncture site is very small and seals rapidly after the needle is removed. 3. Entry into the nondilated collecting system may be difficult and time consuming and, on rare occasions, may fail completely. 2. Evaluation of fistulae involving the urinary bladder (Figure 2-8) 3. Evaluation of healing following bladder or distal ureteral surgery There are no contraindications to cystography itself. When a patient has sustained significant pelvic trauma, the integrity of the urethra must first be established before passing a ureteral catheter. This may often require that retrograde urethrography precede cystography. 2. Cystography may also be performed through an existing cystostomy tube or via suprapubic puncture. Complications of cystography are rare. Excessively forceful injection may result in disruption of a fresh suture line. Since most patients with significant abdominal or pelvic trauma undergo a CT scan for evaluation, the addition of a CT cystogram to assess the bladder is helpful in patients with significant pelvic injury. After the initial set of CT images have been obtained, diluted contrast is injected through an indwelling Foley catheter, and scanning is repeated through the pelvis. Most published reports indicate that CT cystograms and conventional cystograms have comparable sensitivity in detecting bladder injury. An advantage of CT is that the patient does not have to be turned into different projections (an obvious advantage in patients with pelvic fractures) for optimal evaluation, and a postdrain image is unnecessary because the entire bladder is well seen on a CT. When evaluating a patient for a suspected fistula involving the bladder, a CT cystogram helps in demonstrating the fistula well. CT is the most sensitive imaging technique in patients with suspected colovesical fistulae due to complications of diverticulitis. Voiding Cystourethrogram (VCUG) demonstrates the anatomy of the lower urinary tract during micturition and allows assessment for vesicoureteral reflux. 1. Recurrent urinary tract infections, especially in children, in whom reflux is not uncommon 2. Evaluation of the posterior urethra in the male and the entire urethra in the female 3. Evaluation of certain voiding dysfunctions (e.g., detrusor-external sphincter dyssynergia, neurogenic bladder) 4. For the evaluation of an ectopic ureter thought to insert into the urethra Acute urinary tract infection 1. This procedure is best performed under fluoroscopic control. 2. The bladder is catheterized and filled with water-soluble CM. HOCM is usually used for this study because a large amount of contrast is required (300 to 600 cc), and adverse reactions with contrast injection into the bladder are uncommon. When the patient has a strong desire to void, the catheter is withdrawn and the patient voids. Fluoroscopic images are obtained during voiding, and an estimate of the completeness of bladder emptying is made. In patients who have undergone recent bladder-neck or urethral surgery, voiding around an indwelling urethral catheter is initially performed to look for contrast extravasation. If none is seen fluoroscopically, the urethral catheter may be removed and another void documented fluoroscopically. 3. Although the bladder is filled with the patient recumbent, voiding is usually performed with the patient standing. These are the same as those listed under cystography. Retrograde urethrogram (RUG) provides detailed visualization of the anterior urethra in the male. The procedure has little or no application in the female. On a RUG, the posterior urethra is incompletely visualized because the closed external urethral sphincter resists the retrograde flow of contrast into the posterior urethra. Complete evaluation of the anterior and posterior urethra in a male requires both a VCUG and a RUG (Figure 2-10). Although the anterior urethra is seen on a VCUG, a diseased anterior urethra is better demonstrated on a RUG. 2. Suspected urethral trauma 3. Demonstration of urethral diverticula, fistulae, and neoplasms 1. Acute urethritis, as discussed below. 2. Patients who are allergic to contrast should be pretreated. LOCM should be employed in this situation. 2. LOCM is then injected, and fluoroscopic images of the fully distended urethra are taken. Reflux or intravasation of contrast from the urethra into the surrounding corpus spongiosum can occur during RUG. Such reflux is usually minimal and without clinical consequence except in the presence of urethritis when bacteria may be forced into the bloodstream. In patients with venereal warts, the procedure should not be performed until the active infection has been controlled, in order to avoid spreading the infection to the urethra. Spongiosal intravasation is more apt to occur in patients with high-grade urethral strictures. Anastomosis of the ureters to an isolated intact segment of ileum or transverse colon (loop) or to a detubularized large or small bowel segment (pouch) is the most common method of establishing permanent urinary diversion (Figure 2-11). The isolated bowel loop serves as a conduit to propel urine outward toward the stoma, and a urine collection bag is applied to the stoma to collect the urine. A detubularized pouch functions as a continent reservoir rather than a conduit. Pouches can be connected to a cutaneous stoma or be anastomosed to the urethra (orthotopic diversion). Cutaneous continent pouches require intermittent catheterization for emptying, whereas patients with orthotopic pouches void by increasing abdominal pressure to empty the pouch. Radiologic examination of urinary diversions is referred to as loopography or pouchography. 2. To visualize the upper urinary tract by reflux 3. To evaluate patients with loop diversion whose upper urinary tracts show deterioration on serial IVUs or ultrasonogram (i.e., worsening hydronephrosis, renal calculi, or renal scarring) or whose renal function is diminishing There are no contraindications to the retrograde study of a urinary conduit or reservoir other than active urinary tract infection. Because the urinary tract of patients with urinary diversions is usually colonized with bacteria, prophylactic antibiotics are administered prior to the procedure to prevent bacteremia after the procedure. 2. A continent urinary pouch or reservoir is also evaluated fluoroscopically. The stoma (for a cutaneous diversion) or urethra (for an orthotopic diversion) is catheterized and a Foley catheter placed into the reservoir. The reservoir is opacified with CM to capacity, which varies with time. At maturity, it should accommodate several hundred mL of fluid. Filling defects and leaks are documented if present. Nonopaque mucus in the reservoir is an expected finding. Although many pouches do not normally allow for ureteral reflux, reflux may be observed with a Studer pouch in which the ureters are anastomosed to an isoperistaltic afferent loop of ileum, which drains into a detubularized ileal pouch (see Figure 2-11). Although reflux does not occur in a normally functioning Studer pouch, the elevated intraluminal pressures generated during retrograde pouch opacification may fill the isoperistaltic afferent limb and diverted ureters. Pyelonephritis may accompany forceful reflux of infected urine. Angiography refers to the radiologic study of both the arterial and venous systems. Studies pertinent to the study of the urinary tract include: 1. Arterial: aortography, renal arteriography, and adrenal arteriography 2. Venous: inferior venacavography, renal phlebography, adrenal phlebography, and gonadal phlebography 2. Neoplasms 3. Renal trauma 4.
Diagnostic and Interventional Uroradiology
Diagnostic Uroradiology
Plain films (KUB plain radiography)
Indications
Intravenous urography
Indications
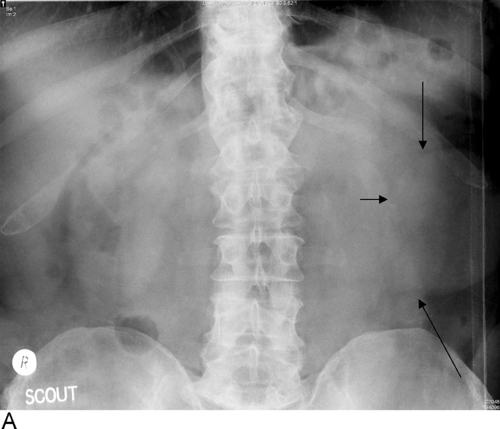
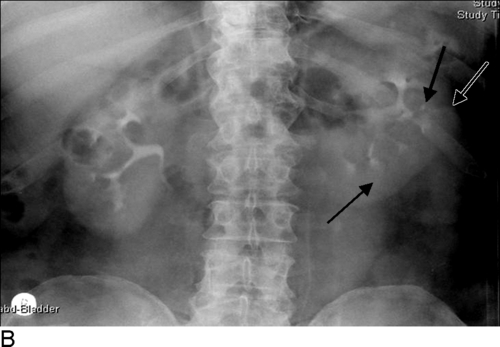
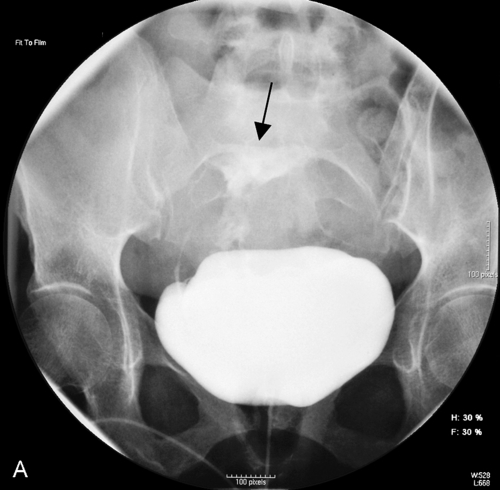
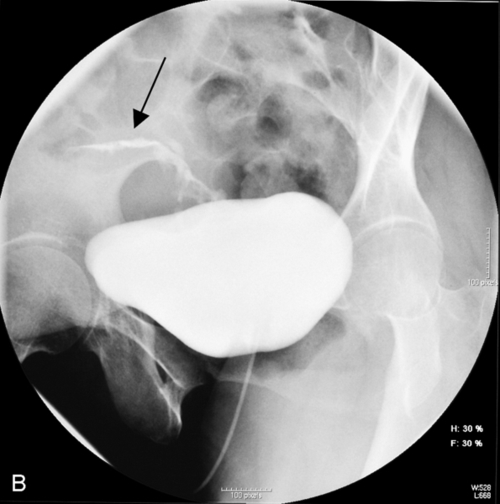
IVU provides evaluation of both the renal parenchyma and the collecting system in patents with gross or microscopic hematuria. However, CT is indisputably more sensitive for detecting renal masses compared to an IVU; although large masses are identifiable on an IVU, it is well recognized that renal masses smaller than 2 cm are often missed on an IVU (Figure 2-1). CT urography (CTU) is sensitive in detecting urothelial abnormalities and is the study most commonly used for a complete assessment of the urinary tract in patients with a history of hematuria. CT is also more sensitive than IVU in detecting urolithiasis; both small stones, and those that are faintly opaque are often not detectable on an IVU (Figure 2-2).



As mentioned above, CTU has superseded IVU for this indication in clinical usage.



However, CT is increasingly being used even for this indication as 3D reconstructions can be performed with high spatial resolution, allowing display of the vascular structures and their relationship to the collecting system. Additionally, the collecting system can also be displayed in a manner similar to that seen on an IVU.
An IVU is often performed 6-8 weeks after a urologic procedure to assess the urinary tract for complications, such as clinically unsuspected obstruction, and to have a baseline postoperative examination.


Patients who present with acute renal colic are best evaluated with noncontrast CT (no oral or intravenous contrast is necessary), which is acknowledged to be the most sensitive and specific study to exclude an obstructing ureteral calculus as the cause of the abdominal pain. This will be addressed further in the section on CT. IVUs are no longer performed in a patient with suspected renal colic because small and faintly opaque stones may not be discernible on an IVU, making it difficult to establish a conclusive diagnosis of stone-induced renal colic. Further, in patients with high-grade ureteral obstruction, it can take up to 24 hours for the collecting system and ureter to opacify densely enough to determine the level of ureteral obstruction. A limited IVU (two to three films obtained after contrast administration) was advocated for pregnant women with suspected urinary colic, but a low-dose CT or MRI is a preferable study in a pregnant woman presenting with abdominal pain.
IVU continues to have a role in the management of patients with known stone disease, to help assess what would be the best therapy for an individual patient, and in follow-up after treatment, with shockwave lithotripsy (SWL), ureteroscopy, or percutaneous methods (Box 2-1).
Radiographic iodinated contrast agents

Technique of IVU
This is an essential component of every radiographic examination of the genitourinary (GU) tract. Urinary tract calculi can be identified only on the KUB because most urinary calculi are obscured by excreted contrast, which has the same radiographic density as calculi. Important findings such as soft-tissue masses, calcifications, and bony changes will also be disclosed on the preliminary film.
CM can be administered intravenously as a rapid bolus injection, slow, steady injection, or drip infusion. This is more often an individual preference rather than a matter of scientific selection. At our institution, patients receive 1 mL contrast per pound of body weight, to a maximum of 150 mL.
Immediately after the contrast has been injected, nephrotomograms are made to visualize the renal parenchyma (nephrographic phase) and assess for renal masses. Within 3 minutes, contrast is usually visible in the collecting systems, and several images are taken to visualize the calyces, pelves, and ureters (pyelographic phase). Images of the bladder (often including a postvoiding film) conclude the examination.






Contraindications
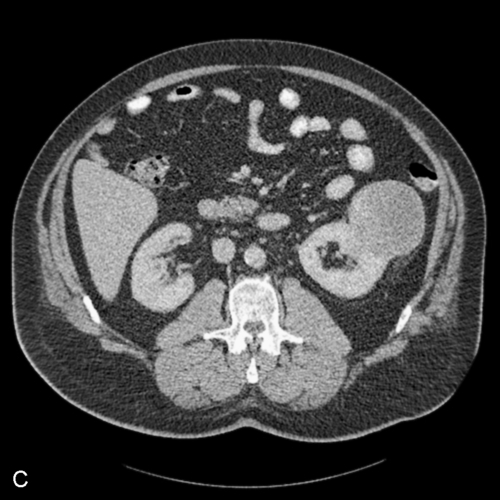
Patients who receive closely repeated doses of intravenous contrast are at greater risk for CIN. This risk is greater than the combined risk of two random contrast examinations. It is best to separate any two studies requiring parenteral contrast administration by at least 24 hours and preferably by 48 hours, during which time the patient should be thoroughly hydrated (see Figure 2-5)
If the decision to give contrast to such patients is made, premedication with corticosteroids and antihistamines is essential, and such patients should be given LOCM, as discussed above. One example of a premedication regimen in clinical use for an elective examination is prednisone 50 mg orally, given 12, 6, and 1 hour before the examination, and diphenhydramine 50 mg 1 hour before the examination, orally or by intramuscular injection. Patients have to be cautioned about the drowsiness that accompanies diphenhydramine administration and should not undertake activities such as driving or other dangerous tasks. For emergent contrast administration, 200 mg hydrocortisone is given intravenously immediately and then every 4 hours until the examination is complete.
Premedicating such patients prior to contrast administration is prudent. Symptoms of nausea, vomiting, or sensation of heat after contrast administration are considered to be side effects of the contrast and not allergic reactions; such symptoms are much less common with LOCM than with high osmolar contrast media (HOCM). Shellfish allergy has no particular significance for contrast administration and is managed the same way as other noncontrast allergies (e.g., allergy to bee sting, penicillin, or peanuts).
However, it is now acknowledged that myeloma does not increase the risk of CIN if the patient is well hydrated.
Although metformin itself does not have an adverse effect on renal function, patients who develop renal failure on the drug (possibly due to contrast administration or other causes) can rarely develop lactic acidosis that can be fatal.
Retrograde pyeloureterography
Indications
Contraindications
Techniques
Complications
Antegrade pyelography
Indications
Contraindications
Techniques
Complications
Cystography
Indications
Contraindications
Technique
Complications
Modifications of cystography
CT cystogram
Voiding cystourethrogram
Indications
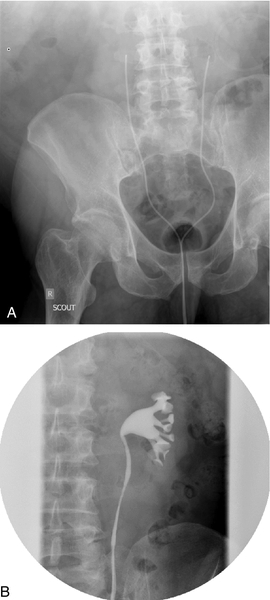
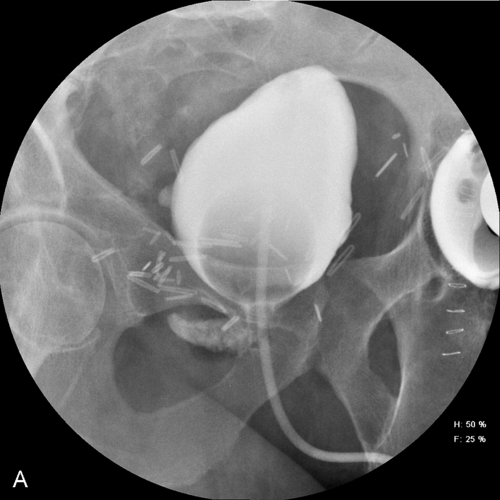
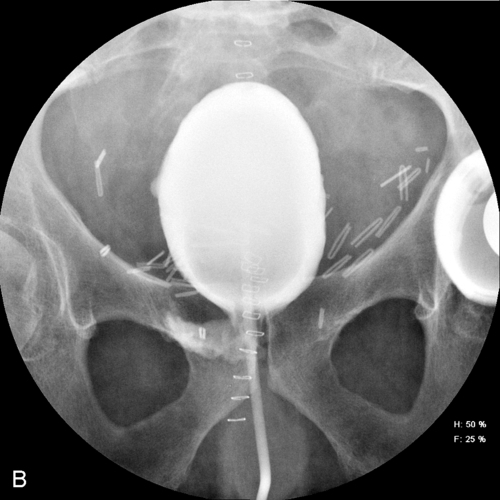
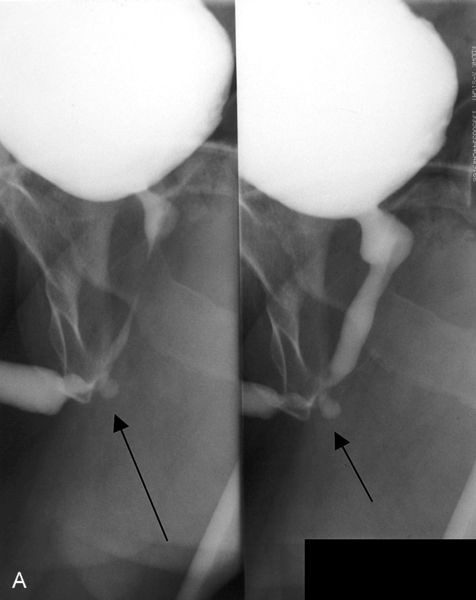
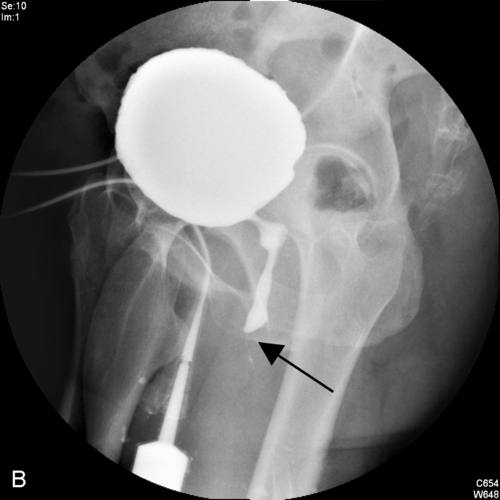
VCUG is used to evaluate urethral stricture disease, posterior urethral valves in the infant male, and the postoperative urethra (Figure 2-9). In the female, it is a primary method of evaluating for suspected urethral diverticula.
VCUG can be combined with simultaneous pressure-flow recordings for a study known as videourodynamics.
Reflux into such ectopic ureters is fairly common.
Contraindications
Techniques
Complications
Retrograde urethrogram
Purpose
Indications
RUG should be routinely performed before attempting passage of a urethral catheter in a male patient with a pelvic fracture.
Contraindications
Technique
Complications
Loopogram and pouchogram

Indications
Reflux is normal with ileal conduits but unpredictable in continent diversions. If a patient with a continent diversion requires urothelial evaluation beyond that provided by an IVU or CTU, antegrade pyelogram is usually the next step.
In such patients, the absence of reflux from the ileal loop into the ureters may indicate ureteroileal obstruction.
Contraindications
Technique
Complications
Angiography
Indications for renal arteriography
Since the development of CT and MRI, angiography is almost never used in the diagnosis of renal masses. It is still used occasionally for the preoperative embolization of large, hypervascular renal cell carcinomas and for prophylactic embolization of angiomyolipomas that are larger than 4 cm in size, to prevent spontaneous hemorrhage.
Most traumatic parenchymal and vascular lesions can be satisfactorily imaged by CT. Angiography is usually reserved to demonstrate an arterial bleeder or arteriovenous communication prior to embolization.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



