Fig. 1
Standardized section of the antrum. Antral area is outlined
The relationship between the antral area as measured by ultrasound and the amount of fasting gastric content quantitated by aspiration through the gastroscope and the increment of the antral area after ingestion of graded volumes of water were highly reproducible, with small variations within 1 h and from day to day, and there was a highly significant correlation between the ultrasonographically measured antral area and the amount of fasting gastric juice and between the increase in the antral area and amounts of ingested water (Hveem et al. 1994).
Recent studies have shown that fasting and postprandial antral areas increase in patients with functional dyspepsia and diabetes mellitus compared with normal subjects (Undeland et al. 1997; Hveem et al. 1996). The antral area, and hence antral distention, is a significant determinant of postprandial fullness (Hausken et al. 1992).
3 Gastric Emptying
Scintigraphy is at present the “gold standard” for clinical measurement of gastric emptying. Scintigraphy provides quantitative information about total stomach emptying and intragastric meal distribution of both solid and liquid meals (Collins et al. 1988). With the use of a gamma-camera, the rate of gastric emptying of a standardized test meal marked with a radioisotope can be calculated. Scintigraphy requires expensive equipment that is often not readily available, is associated with a radiation burden, and cannot detect individual episodes of transpyloric flow.
Using ultrasound, gastric emptying has typically been assessed by changes in either the antral cross-sectional area or diameter (Bolondi et al. 1985; Holt et al. 1986). In order to establish ultrasound as an acceptable or even preferred method in assessing gastric emptying, studies have been conducted to compare ultrasound with scintigraphy.
In order to do so, the subjects are usually seated with their back against the gamma camera and the ultrasound transducer is positioned in the region of the umbilicus. The first measurement is performed within 1 min of meal ingestion, followed by subsequent images at intervals depending on which meal is used. Ultrasound T50 is defined as the time when the antral area is decreased to half its maximum (Horowitz et al. 1993).
With a high- and low-nutrient liquid meal, scintigraphic and ultrasonographic 50 % emptying times (T50′s) were comparable and longer for dextrose (300 kcal) than for meat soup (20 kcal) (dextrose 107 ± 16 min vs. 108 ± 18 min, soup 24 ± 4 min vs. 23 ± 5 min). A close correlation was found between scintigraphic and ultrasound T50 and the T50, and the limits of agreement were good (Hveem et al. 1996).
Other comparative studies between ultrasound and scintigraphic measurements of gastric emptying have shown a very close relationship between the two methods (Bolondi et al. 1985; Holt et al. 1986). The intra–individual variation in gastric emptying of liquids in normal subjects, however, is relatively large.
4 Proximal Stomach and Gastric Accommodation
We have developed a sonographic method to monitor postprandial size of the proximal stomach. A proximal gastric area in a sagittal section (Fig. 2) is outlined by tracing from the top margin of the fundus and 7 cm downward along the axis of the stomach as described by Gilja et al. (1995). Diameter on the fundus (Fig. 3), defined as the maximal diameter in an oblique frontal section kept within 7 cm along the axis of the proximal stomach, is chosen as the second measure. The subjects are scanned in a sitting position with a 3.25-MHz transducer after ingestion of 500 ml meat soup and the measurements are performed 10 and 20 min postprandially.
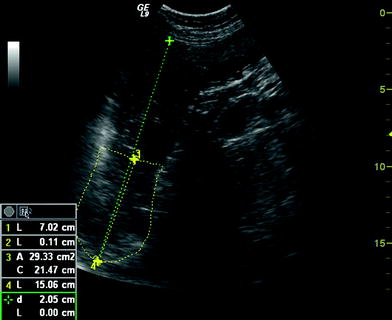

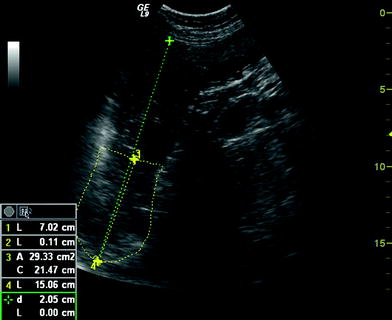
Fig. 2
A proximal gastric area in a sagittal section is outlined by tracing from the top margin of the fundus and 7 cm downward along the axis of the stomach

Fig. 3
A fundal diameter defined as the maximal diameter in an oblique frontal section kept within 7 cm along the axis of the proximal stomach
The soup emptied from the proximal stomach in a linear manner with a moderate day-to-day variation, low intra- and interobserver error, and the method allowed estimation of initial emptying fractions of the proximal stomach (Gilja et al. 1995).
Ultrasound of the proximal stomach has shown that patients with functional dyspepsia and diabetes have a smaller proximal stomach than healthy subjects (Gilja et al. 1996; Undeland et al. 1998). Sublingual glyceryl trinitrate improves accommodation of the proximal stomach to a meal as measured by ultrasound and reduces postprandial symptoms in a group of patients with functional dyspepsia (Gilja et al. 1997a, b).
In reflux esophagitis patients, the sagittal area of the proximal stomach was significantly larger after a meal, and the patients experienced more epigastric fullness (Tefera et al. 2001, 2002). The findings with both 2D and 3D ultrasound methods in gastroesophageal reflux disease (GERD) patients are consistent with the results of other recently published studies. Zerbib et al. (1999) found a more pronounced relaxation of the proximal stomach in GERD patients using a barostat, and observed an inverse correlation between maximal postprandial relaxation and severity of disease. Penagini et al. (1998) found delayed recovery of proximal gastric tone after intake of a combined solid and liquid meal in GERD patients.
The “gold standard” to study gastric accommodation after a meal has been the barostat. The barostat measures gastric wall relaxation and from that one can infer gastric tone. However, introducing the barostat balloon into the gastric lumen may influence the gastric motility patterns (Moragas et al. 1993; Ropert et al. 1993), and furthermore the examination is invasive and unpleasant. Neither the barostat nor scintigraphy allows estimation of the size of the proximal stomach. On the contrary, ultrasound and SPECT scanning can detect changes in gastric volume in a noninvasive manner. Like ultrasound, SPECT scanning is a noninvasive alternative to the barostat in evaluating gastric relaxation. However, in comparison with meal-induced volume increase, SPECT scanning failed to detect the profound gastric relaxation following glucagon infusion. These findings suggest that SPECT scanning is less suitable than the gastric barostat in detecting gastric relaxation and rather detects the volume of the intragastric contents after meal intake.
An important question is whether imaging methods, such as MRI, SPECT, or ultrasonography, can actually be compared to the measurements made by the barostat. We believe that imaging methods and the invasive barostat method do not measure the same aspects of the gastric accommodation process. Thanks to its close contact with the gastric wall, the barostat bag adjusts to changes in proximal gastric pressure by changing the intrabag volume. Thus, changes in volume are believed to reflect changes in muscle tone of the wall. However, the quantitative change in volume seen during barostat examinations is only valid during barostat studies using exactly the same equipment and positioning technique. Imaging methods, however, visualize directly the size of the gastric compartments, thus giving an indirect measure of relaxation and contraction. The volume change seen using imaging can thus be explained by additional secretion, air retention, or most probably changes in gastric emptying.
The gastric meal accommodation process has two components: passive meal distension of the gastric compartments and active muscle relaxation of the gastric wall. The first component is best measured with imaging methods, whereas the barostat is best suited for studying the second component. Imaging methods, at this stage, do not distinguish between enlargements of the stomach due to reflex relaxation or due to meal-induced distension; it just measures the totally accommodated volume. Accordingly, it may not be adequate to compare imaging methods to the barostat for validation of gastric accommodation. Gastric accommodation depends on neuromuscular factors and hence it is also a matter of evaluation of the mechanical properties of the stomach. In this sense, the barostat merely detects the existence of change in wall tone, but cannot, like imaging methods, provide data on the distribution of the volume and the normal behavior of the gastric wall. In biomechanics, it is essential to understand the geometry of the organ and the forces and deformation in different directions in order to better understand the active–passive muscle function and mechano-sensation in health and in diseases such as the functional disorders. This warrants 2D and 3D image analysis of the gastric compartments.
The different imaging methods exhibit different spatial and temporal image resolution and these factors strongly influence accuracy in volume calculation. MRI, and in particular SPECT, imaging have poor spatial and temporal resolution compared to ultrasonography. Ultrasonography can provide temporal resolution above 100 fps, if necessary, and a spatial resolution at submillimeter level. Also, the “stress-factor” of the imaging methods should be considered in this context because dyspeptic patients in general, and vagal reflexes in particular, are very sensitive to psychological stress. Anyone who has been inside a narrow, noisy MR scanner knows how frightening this can be. Naturally, the stress-factor is also substantially involved in studies using the barostat. Simply because functional disorders are so strongly associated with psychological factors, the examination should be performed in a quiet and relaxing atmosphere with a minimum of distress. Ultrasonography satisfies these criteria as it is noninvasive and does not in itself distort the physiological response in stress-responsive individuals. Moreover, due to gravity playing a central role in the propulsion of gastric content, the study of meal accommodation should preferably be performed in a “natural position” such as sitting in a chair. Therefore, methods that enable patients to be seated have an advantage over methods requiring patients to be in a supine position during the examination.
5 Antral Peristalsis
Antral contractions (3 per minute) are responsible for mixing and grinding of a solid meal into smaller particles (<5 mm) that can pass onto the duodenum. These antral contractions can easily be seen at ultrasonography. The contractions can be occlusive or nonlumen-occlusive. An antral contraction is defined as an indentation of the gastric wall greater than one antral wall thickness, which is not due to respiration, pulsation transmitted from the aorta or heart, or to movements of adjacent intestine.
A lumen-occlusive contraction is defined as a contraction in which the ultrasound image shows the gastric walls to come into apposition at some point along the imaged antrum.
Amplitude of antral contractions is measured as a fraction of relaxed area and the motility index is calculated as the amplitude multiplied by frequency.
The motility index as measured by ultrasound was reduced in patients with functional dyspepsia (FD). The effects of acute mental stress on gastric antral motility were reduced by mental stress in the healthy individuals, but not in FD patients (Hausken et al. 1993).
Manometry is the most widely used method for measuring gastric motility (Malagelada and Stanghellini 1985; Husebye 1999). Manometric studies have demonstrated that the patterns of luminal pressure waves are complex both in the fasting and fed states. So far, only two studies assessing concurrent ultrasound and high-resolution manometry have been published.
In the study by Hausken et al. (2002), in the pre- and postprandial period, a total of 44 % of antral contractions were not detected by manometry, and only 1/5 of nonoccluding contractions.
Hveem et al. (2001) found that only 53 % of antral contractions seen ultrasonographically had a temporally associated pressure event in the manometric reference channel. The lumen-occlusive contractions had, in 69 %, an associated pressure event. Of the nonlumen-occlusive contractions, only 20 % were associated with a pressure event.
The median amplitude of the pressure events in the manometric reference channel was 16 mmHg (range 4–98 mmHg) for lumen-occlusive, and 7 mmHg (range 4–23 mmHg) for nonlumen-occlusive contractions. However, a substantial overlap exists between the two categories of contraction.
In about 50 % of antral contractions observed by ultrasound, the corresponding pressure events are not identified in the manometric reference channel. This more than indicates that the knowledge of gastric mechanics, based solely on manometry, is at the least inadequate, missing almost half of the information given by ultrasound with regard to antral contractions.
6 Flow of Luminal Contents
Information concerning movement of luminal contents in humans can be obtained by fluoroscopy, scintigraphy, MRI, impedance, and duplex sonography.
Studies based on scintigraphy and standard ultrasound of the stomach and duodenum will indirectly measure overall rates of gastric emptying, but these methods do not have the temporal resolution to assess on a second-to-second basis. However, promising new MRI methods are being developed. Echo planar imaging, an ultrafast variant of MRI, can provide excellent images of both gastric wall movements and movements of solid and liquid meals.
Ultrasonographic studies by King et al. (1984) using test meals containing bran particles showed that gastric emptying occurred in episodes lasting a few seconds in healthy subjects. The emptying period usually started immediately after relaxation of the antro-pyloro-duodenal segment and was finished before the next peristaltic contraction approached the distal antrum. A brief episode of duodenogastric reflux occurred in about 60 % of the peristaltic cycles shortly before the terminal antral contraction. A similar type of reflux was shown in dogs by Malbert and Ruckebusch (1991), who used operatively implanted electromagnetic flow meter probes. Hausken et al. (1992) showed that using pulsed Doppler combined with real-time ultrasonography (duplex sonography), it is possible to visualize antroduodenal motility and transpyloric flow simultaneously. Antegrade and retrograde transpyloric flow is visualized using bidirectional velocity curves. Most contractions of the proximal duodenal bulb precede closure of the pylorus (and the terminal antrum), and duodenal bulb contraction is often accompanied by a short burst of duodenogastric reflux occurring immediately before closure of the pylorus.
Studies of the antro-pyloro-duodenal region are performed with the ultrasound probe positioned at the level of the transpyloric plane, and the antrum, the pylorus, and the proximal duodenum are visualized simultaneously. The subjects are studied in a seated position, with a 3.5 to 5-MHz transducer.
In order to study the relation between motility and flow in detail, techniques with a high temporal and spatial resolution are required for the assessment of antro-pyloro-duodenal pressure waves and transpyloric flow. Subjects have to be intubated with a manometric assembly, which is introduced transnasally and positioned in the antro-pyloro-duodenal region using fluoroscopy. The Doppler/ultrasound and manometric recordings have to be synchronized (Hausken et al. 2002).
First gastric emptying is defined as the first occurrence of gastric emptying after drinking of the soup is initiated. An episode of gastric emptying is defined as flow across the pylorus with a mean velocity of more than 10 cm/s lasting more than 1 s.
Occluding peristaltic-related transpyloric emptying is defined as gastric emptying associated with contractile activity in which the ultrasound image shows an occlusion of the stomach wall. Nonoccluding peristaltic-related emptying is defined as transpyloric emptying of gastric contents associated with contractile activity of the gastric wall which does not occlude the lumen. During maximal contractions, transpyloric flow can still be seen passing back and forth through the open pylorus.
Nonperistaltic-related transpyloric emptying is defined as transpyloric emptying of gastric contents, without contractions detected on ultrasound or manometry.
Gastric emptying of a low caloric liquid meal follows sequences of emptying-reflux-emptying pulses. About half of the sequences are peristaltic related, but both nonoccluding, peristaltic-related, and nonperistaltic-related emptying sequences occur. Nonperistaltic-related flow sequences often have more alternating emptying-reflux episodes than those associated with peristalsis, and the duration of nonperistaltic-related emptying and reflux pulses are longer. The pressure gradients for all types of emptying are low and the pressure gradients during nonperistaltic-related emptying are significantly lower than during peristaltic-related emptying.
Flow can only occur in the presence of an open pylorus. Transpyloric flow can be classified into flow associated with a local increase in the pressure gradient between antrum and duodenum (Pa–Pd) due to antral propagating pressure waves. The second type of flow is independent of peristalsis and is likely to be caused by changes in gastric tone, or by pressure changes outside the stomach such as aortic pulsation and inspiration (Hausken et al. 2002).
The method can be used to study normal physiology and pathophysiology of the gastro-pyloro-duodenal segment and to monitor the effect of medications on transpyloric flow.
Patients with functional dyspepsia often experience early satiety and discomfort after a meal. Using duplex sonography it is possible to relate timing of symptoms and early postprandial emptying in patients with functional dyspepsia (Hausken et al. 1998). Meal-related discomfort was experienced after commencement of transpyloric emptying. An inverse relationship was found between the duration of the tasting period and symptom intensity, suggesting that the time allowed for duodenal tasting might be too short in patients with functional dyspepsia.
Currently available methods for studying gastric emptying do not provide quantitative information about the movement of gastric contents. A new noninvasive method for evaluating stroke volumes using three-dimensional (3D) guided digital color Doppler imaging might help the investigator to quantify net gastric emptying and to estimate the amount of duodenogastric reflux (Hausken et al. 2001). The technique involved color Doppler digital images of transpyloric flow in which the 3D position and orientation of the images were known by using a magnetic location system. In vitro, the system was found to slightly underestimate the reference flow (by average 8.8 %). In vivo (five volunteers), stroke volume of gastric emptying episodes lasted on average only 0.69 s with a volume on average of 4.3 ml (range 1.1–7.4 ml), and duodenogastric reflux episodes on average 1.4 s with a volume of 8.3 ml (range 1.3–14.1 ml). It was concluded that with the appropriate instrument settings, orientation determined color Doppler can be used for stroke volume quantification of gastric emptying and duodenogastric reflux episodes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








