Fig. 1
Ileocecal tuberculosis. Transverse sonogram of the right lower abdomen shows diffuse thickening of the terminal ileum (TI) and cecum (C)
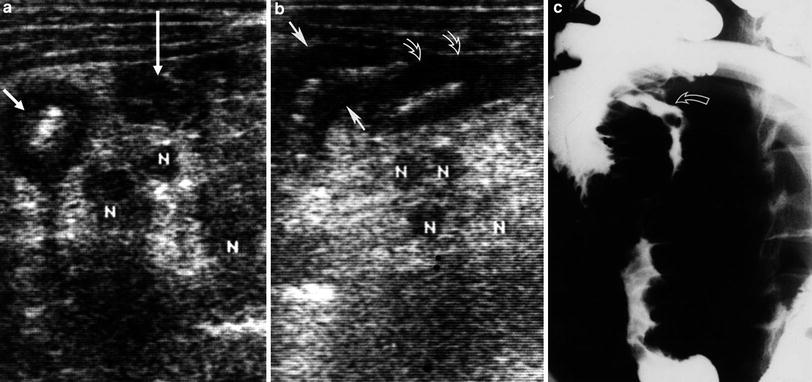
Fig. 2
Ileocecal tuberculosis and associated mesenteric lymphadenitis (reproduced with permission, Lim et al. 1994). a Transverse sonogram of ileocecal region shows thickening of the wall of the cecum (short arrow) and terminal part of the ileum (long arrow). Note enlarged mesenteric lymph nodes (N) and thickened mesentery around lymph nodes. b Longitudinal sonogram shows thickening of the cecum (solid arrows) and terminal part of the ileum (open arrows) and enlarged lymph nodes (N). c Barium examination shows irregular narrowing of the terminal part of the ileum and cecum. Note longitudinal ulcer (curved arrow) at the terminal part of the ileum. Mucosal folds are markedly thickened and irregular
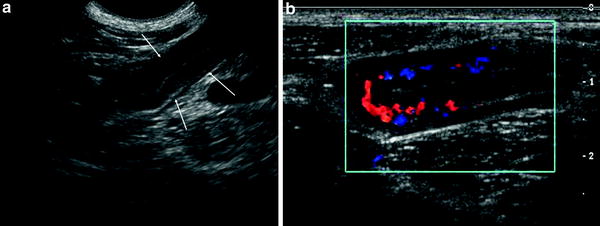
Fig. 3
Ileal tuberculosis. a Transverse sonogram of right low quadrant abdomen shows diffuse mural thickening of the terminal ileum. The terminal ileum shows concentric thickening (arrows). The thickness of the anterior and posterior walls is the same. b Transverse color Doppler sonogram of the terminal ileum shows numerous color signals
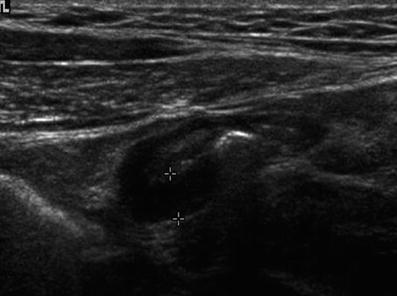
Fig. 4
Ileal tuberculosis. Transverse sonogram of the right lower quadrant abdomen discloses eccentric thickening of the posterior wall of the terminal ileum
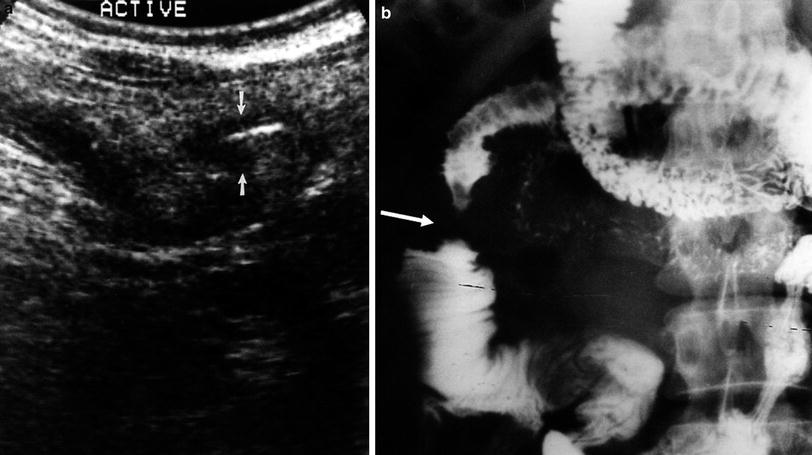
Fig. 5
Jejunal tuberculosis. a Transverse sonogram of the right upper abdomen shows a short segmental wall thickening of the jejunum (arrows). b Small bowel follow-through examination shows a segmental stricture of the jejunum (arrow). Note thickening of the mucosal folds at the proximal loop
Ultrasonography detects ulceration within the thickened wall in only a few cases, whereas it is seen frequently during small bowel follow through examination or barium enema studies. This low sensitivity for the detection of ulcers on sonography may be due to the associated spasm (Kedar et al. 1994). Lymphoid tissue involvement in the ileal wall with ulceration, necrosis, fibrosis and often with extensive granulomatous infiltrate can be observed (Khaw et al. 1991). In a few cases of intestinal tuberculosis, a spasm of the cecum is identified by a collapsed lumen and irritability of the thickened wall (Lee et al. 1993).
3.2 Hyperemia
Although subjective, color Doppler imaging is helpful for distinguishing active inflammatory changes in the thickened bowel wall from other pathologies (Fig. 3) (Wilson 1998; Teefey et al. 1996). Power Doppler imaging may improve the visualization of intramural gastrointestinal vascularity (Clautice-Engle et al. 1996). Thus, recent advances in color Doppler and power Doppler imaging improve the accuracy of sonography by allowing the detection of hyperemia of the inflamed bowel wall and of adjacent inflamed fat.
3.3 Stricture
In the active stage of intestinal tuberculosis, bowel wall thickening is usually accompanied by luminal narrowing, which results from spasm and edema. Later, fibrosis and scarring lead to permanent stricture (Fig. 5). However, it is difficult to detect stricture during sonographic examinations (Kedar et al. 1994).
3.4 Mesenteric Lymphadenitis
In active tuberculosis, enlarged mesenteric nodes are frequent. Lymphadenopathy is mainly located at the mesentery around the ileum (Fig. 2) (Lee et al. 1993), but sometimes found at the periportal (Fig. 6), peripancreatic, mesenteric, and upper periaortic regions (Malik and Saxena 2003). However, the retroperitoneal lymph node is rarely involved, which can be explained by the fact that mesenteric lymph nodes drain directly into the thoracic duct via the cisterna chyli (Jain et al. 1995). Enlarged lymph nodes are hypoechoic, round to ovoid, and variable in size. Sometimes the nodes may be calcified (Malik and Saxena 2003; Kedar et al. 1994); calcification in healing tuberculosis is seen as a discrete reflective arc with posterior shadowing.
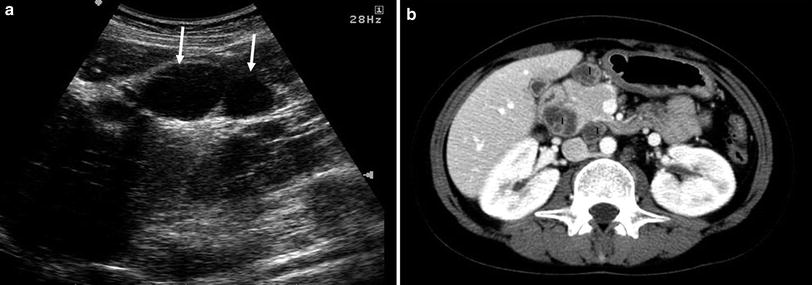
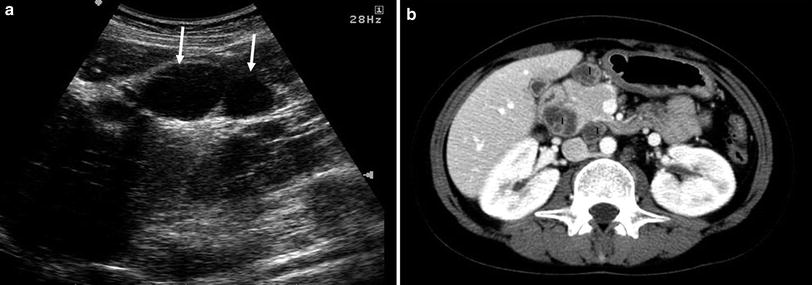
Fig. 6




Tuberculous lymphadenitis. a Transverse sonogram of the right upper quadrant abdomen shows hypoechoic lymph node enlargement at porta hepatic (arrows). b Abdominal CT shows multiple peripancreatic lymph node (l) enlargement. The enlarged lymph nodes show central low attenuation with marginal rim enhancement due to central caseous necrosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








