Totally Extraperitoneal Inguinal Hernia Repair Using Fibrin Glue
Benjamin S. Powell
Guy R. Voeller
Inguinal hernia repair is one of the most common surgical procedures performed not only in the United States, but also around the world. It is estimated that between 15% and 30% of inguinal hernias are now fixed laparoscopically depending on geographic location. With the advent of new technology there are a variety of ways a surgeon can fix a reducible inguinal hernia. Most methods have literature supporting a very low recurrence rate when using a mesh in either an open or laparoscopic approach. We advocate fixing all symptomatic inguinal hernias if the patient can tolerate surgery. When we are referred a patient with an asymptomatic inguinal hernia we advise them of watchful waiting but often if the hernia is protruding the patient will elect to have surgery even if it is not causing symptoms. Most of the choices for which approach to perform are up to the judgment of the surgeon. We perform both laparoscopic and open repairs for inguinal hernia (about 200 per year) but believe that the laparoscopic approach requires a different skill set and expertise for excellent long-term results and should not be done by the surgeon that repairs 20 to 30 inguinal hernias per year unless most of these are done laparoscopically.
The only absolute contraindication for TEP inguinal hernia repair is the inability to tolerate general anesthesia. For these patients we recommend open repair under local anesthesia with a mesh. We also believe that in patients who have had previous preperitoneal surgery such as prostate removal, the TEP approach is too difficult and even though studies show that it is possible and has higher risks than an open operation in virgin tissues. In addition, if the hernia cannot be completely reduced such as large scrotal hernias we will opt for the easier to do open approach. We will perform the TEP repair in large, older teenagers if the hernia is significant in size and requires mesh.
Lastly, in men in whom there is concern about elevated PSA levels and prostate cancer, they should be told that the TEP may make preperitoneal prostate removal more difficult in some cases depending on the mesh used and the experience of the urologist. Even though studies show that in expert hands preperitoneal prostate removal is readily done after a previous TEP repair, this should be discussed at length with this patient population.
This chapter will discuss the technique of totally extraperitoneal (TEP) inguinal hernia repair with polyester mesh and fibrin glue. Some authors contend that TEP inguinal hernia repair is best used only for bilateral and recurrent inguinal hernias, but we believe that it is an excellent repair for unilateral hernias when the surgeon is an expert at the operation. In recurrent hernia there often is scarring in the preperitoneal space from the previous open repair that can make the TEP somewhat more difficult and the occasional TEP surgeon may struggle. In addition, until one is over the learning curve, doing bilateral repairs will take far too long and the surgeon will become frustrated and cease learning how to do the operation. For one to become a very good TEP surgeon, it is critical to do many unilateral repairs. The senior author has performed approximately 3,000 TEP repairs and new challenges are still frequently encountered to this day.
Unilateral, bilateral, and recurrent inguinal hernias
Contraindications:
Inability to tolerate general anesthesia
Previous preperitoneal surgery
Large scrotal hernias that cannot be reduced
Elevated PSA (relative)
Small, young children
Preoperative planning for TEP inguinal hernia repair typically revolves around the choice of whether the patient is a candidate for the repair. The decision should be dictated by the surgeon’s expertise and the indications and contraindications discussed in the previous section. Most all studies show that the laparoscopic approach has less intense immediate pain leading to quicker return to regular activity. In addition, recent studies show that in expert hands the TEP repair has less chronic long-term pain risk. However, the surgeon should do the repair that they do most often and if this is not TEP then it should not be offered. We stop any and all anticoagulation and if a heparin bridge is required until the day of surgery we make sure that it is not given the night before the surgery. Aspirin is stopped, but the operation can usually safely be done if the patient requires this drug.
We do not believe that each patient should have both groins addressed unless there is a good reason. If the patient is complaining of problems in a groin where no bulge can be palpated and is undergoing repair of the contralateral groin, we will evaluate the “non-impulse” side at the time of surgery. If the patient is undergoing a unilateral repair that turns out to be a direct defect at the time of surgery, we always look at the contralateral direct space. Direct hernia disease is a collagen problem and we almost always will repair the contralateral side unless it is absolutely perfect in appearance. We have found that if you do not do so in these patients, they will soon return for repair of this side. It is thus critical that a good inguinal exam of both groins be done preoperatively and documented well. We will obtain herniograms in patients if there is some question about a true hernia being present.
Pertinent Anatomy
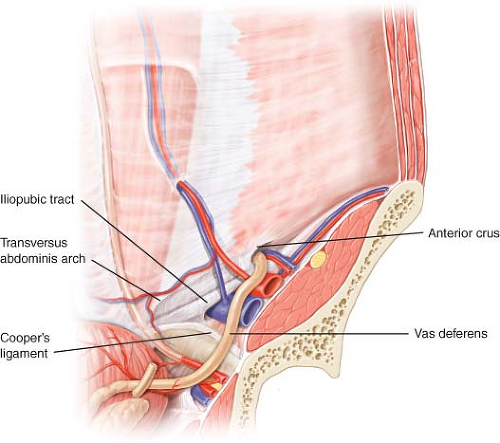
A thorough knowledge of preperitoneal anatomy is required to perform an excellent TEP. Adequate dissection in this space allows for complete visualization of the myopectineal orifice and any defects therein (Fig. 17.1). Initial dissection of
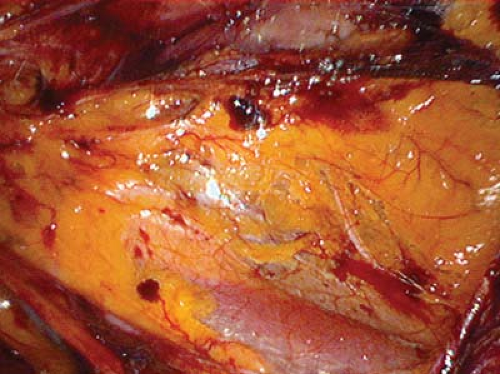
a TEP hernia begins in the posterior rectus space. Below the arcuate line, the posterior rectus sheath is attenuated and the preperitoneal space is then entered. This space is continuous with the space of Retzius of the pelvis. In the lower portion of the abdomen, dissection is fairly easy in regards to dissecting the cord structures free from the preperitoneal fascia surrounding them as well as the peritoneum. The phrases such as “triangle of pain” and “triangle of doom” we believe should be done away with since while the overall make-up of the myopectineal region is constant, there is quite a bit of variability of the location of the iliac artery in relation to the peritoneum and cord structures and the various nerves also have significant variability in location (Fig. 17.2). We believe that a thorough understanding of the entire myopectineal area and its variabilities is critical to avoiding serious disasters. In some 3,000 TEP repairs we have not had an injury to bladder, colon or iliac artery or vein showing that this operation can be done safely if the surgeon learns the anatomy. Understanding the anatomy depicted in Fig. 17.1 is the key to a successful TEP repair. Landmarks such as the pubic bone, Cooper’s Ligament, inferior epigastric vessels, and cord structures are the key in assisting the surgeon to stay oriented in this small and anatomically “busy” space.
a TEP hernia begins in the posterior rectus space. Below the arcuate line, the posterior rectus sheath is attenuated and the preperitoneal space is then entered. This space is continuous with the space of Retzius of the pelvis. In the lower portion of the abdomen, dissection is fairly easy in regards to dissecting the cord structures free from the preperitoneal fascia surrounding them as well as the peritoneum. The phrases such as “triangle of pain” and “triangle of doom” we believe should be done away with since while the overall make-up of the myopectineal region is constant, there is quite a bit of variability of the location of the iliac artery in relation to the peritoneum and cord structures and the various nerves also have significant variability in location (Fig. 17.2). We believe that a thorough understanding of the entire myopectineal area and its variabilities is critical to avoiding serious disasters. In some 3,000 TEP repairs we have not had an injury to bladder, colon or iliac artery or vein showing that this operation can be done safely if the surgeon learns the anatomy. Understanding the anatomy depicted in Fig. 17.1 is the key to a successful TEP repair. Landmarks such as the pubic bone, Cooper’s Ligament, inferior epigastric vessels, and cord structures are the key in assisting the surgeon to stay oriented in this small and anatomically “busy” space.
Positioning
Proper patient positioning is key for laparoscopic inguinal hernia repairs as with other laparoscopic techniques. The patient is placed supine on the operating room table with arms tucked at the side. We typically have a laparoscopic monitor placed at the foot of the table. We remove a stripe of hair, the width of the hair trimmer, in the midline from above the umbilicus to just below the pubic bone. We always place a Foley catheter since a fully decompressed bladder is key in direct hernias in allowing the mesh to be safely placed far down over the pubic bone as it must be in these defects. We only use 5cc of fluid in the Foley balloon since 10cc is very prominent during the repair. Some surgeons will have the patient empty their bladder prior to the operation, but we have found that the intravenous fluid given by anesthesia quickly fills the bladder and can limit the ability to place the mesh down over the pubic bone as far as possible. An alcohol-based prep is used and an Ioban™ is placed to prevent mesh contact with skin flora. The risk of mesh infection in TEP is almost non-existent. We have never had a mesh infection in our some 3,000 TEP repairs using the Ioban™ and thus prophylactic antibiotics are not indicated.
Operative Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree