Fig. 18.1
Patient positioning
Fig. 18.2
Operation room set-up
18.3.2 Access Device
A 3.5-cm incision is made at the umbilicus. We prefer use of the Lap-protector FF1010™ and the EZ access™ for the protector (Hakko Co. Ltd., Nagano, Japan) (Fig. 18.3), which can be assembled as an umbilical access device (Fig. 18.4). A 12-mm trocar and three 5-mm trocars are inserted through the EZ accessTM device. A 5-mm, 30-degree endoscope, both of the surgeon’s forceps, and the assistant’s forceps are inserted through the respective trocars (Fig. 18.5). The energy device, stapler, and gauze are inserted and removed through the 12-mm trocar.


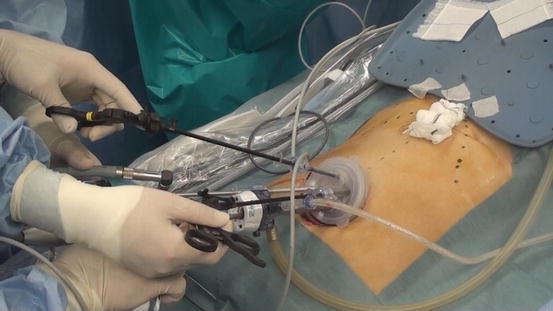

Fig. 18.3
The Lap protector FF1010™ (Hakko) and EZ access™ (Hakko) for FF1010 are assembled

Fig. 18.4
Desktop simulation
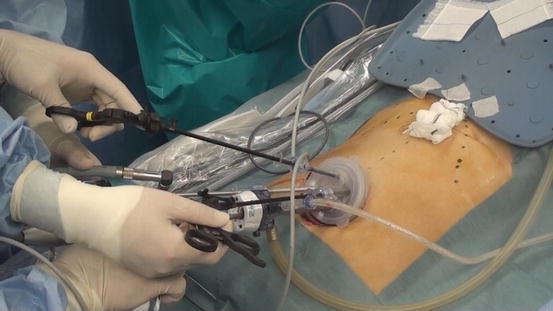
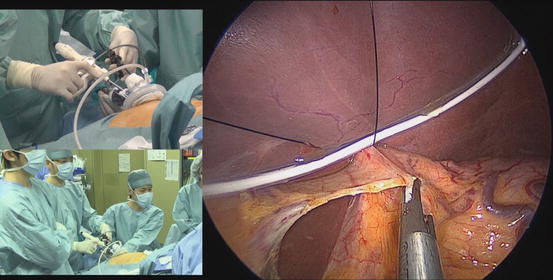
Fig. 18.5
External view of the single-port at the umbilicus
18.3.3 Liver Retraction
The liver retraction procedure is important for gastrectomy. We retract the left lobe of the liver in two steps without the use of a trocar or retractor (Fig. 18.6). The round ligament of the liver is lifted with 2-0 nylon thread attached to a straight needle that has been inserted percutaneously into the abdominal cavity. The needle is passed over the round ligament and then out through the skin. A medium size silicon-disc (Hakko Co.) is introduced into the abdominal cavity and placed under the left lobe of the liver. The straight needle with the 2-0 nylon thread is introduced by percutaneous puncture, directed through the front side of the disc, the central tendon of the diaphragm at the dorsal side of the disc, and again through the disc on the patient’s right, withdrawn percutaneously, and tied extracorporeally. With experience, this series of step is performed within 5 min. We believe this method of liver retraction without scaring is effective and that it prevents postoperative transaminase elevation.
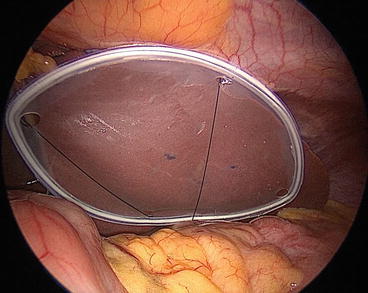
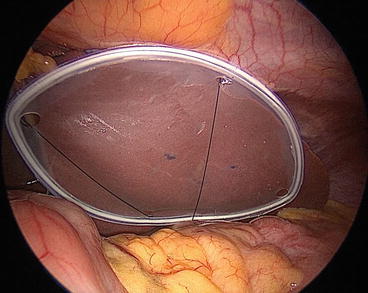
Fig. 18.6
A silicon disc is placed for liver retraction
18.3.4 Procedure
Dissection of the left side of the greater omentum: the lymph nodes are dissected in the same manner as in CLDG. The difference between SPLG and CLDG is how the tissue is manipulated. In SPLG, two forceps are used instead of three. To begin laparoscopic insufflation, the operation table is tilted into the head-up position (Fig. 18.7).


Fig. 18.7
Dorsosacral and head-up tilt position
The first surgical step is opening the greater omentum. The greater curvature of the middle stomach is grasped by the assistant and lifted upward, and the middle portion of the greater omentum is cut with a bipolar sealing device toward the origin of the left gastroepiploic artery and vein (Fig. 18.8), which are then clipped and cut (Fig. 18.9). The short gastric arteries and veins are then coagulated and cut with the use of a bipolar sealing device and no clips (Fig. 18.10). The gastro-splenic mesentery should be carefully treated during dissection, otherwise bleeding can occur.
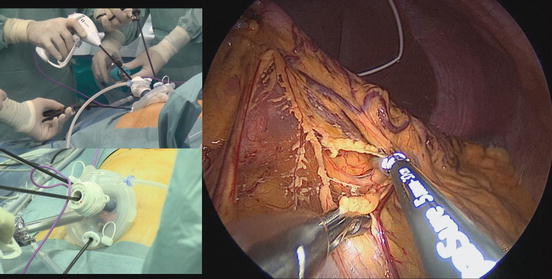
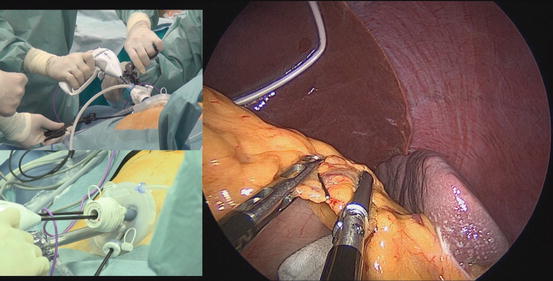
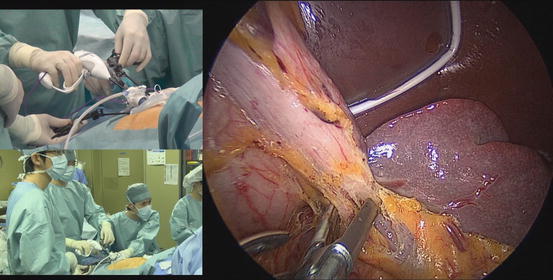
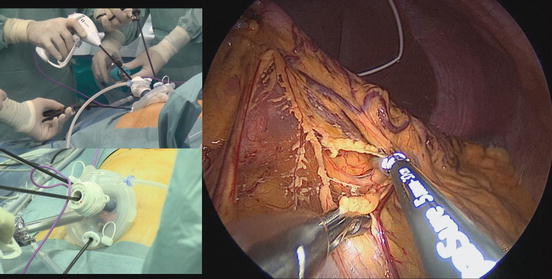
Fig. 18.8
The middle portion of the greater omentum is opened
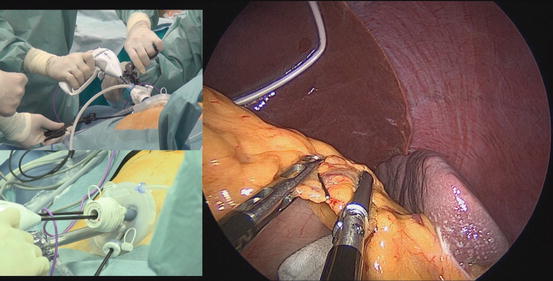
Fig. 18.9
The origins of left gastroepiploic artery and vein are clipped and cut with a bipolar sealing device
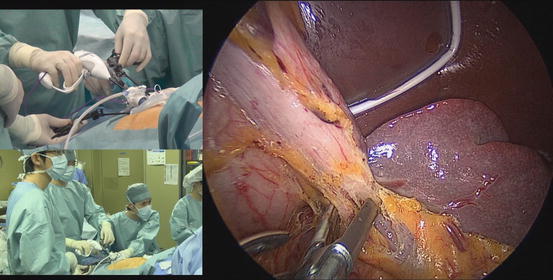
Fig. 18.10
Short gastric arteries and veins are coagulated and cut with a use of a bipolar sealing device and no clips
Dissection of the right side of the greater omentum: the central portion of the greater omentum is cut with a bipolar sealing device toward the right side of the omentum (Fig. 18.11). This means the greater omentum is taken off the transverse mesocolon. The goal of the right-side dissection is the wall of the descending duodenum. In dissection around the root of right gastroepiploic artery and vein in the pyloric area, the assistant grasps the peripheral part of the gastroepiploic vessels, and the surgeon creates traction by applying gauze and pushing downward on the mesocolon. The artery and vein are clipped and cut, and the remaining tissue, including No. 6 lymph node, is completely dissected (Fig. 18.12). An ultrasonically activated device (USAD) is generally used for precise dissection. In using a USAD, the surgeon must take care to avoid cavitation, which can occur at the tip of the active USAD blade. To avoid cavitation, it is important to incline the pedicle of the gastroepiploic artery and vein to both sides in a flag-like motion, freeing the tip of the active blade from other vessels and pancreatic tissue. A titanium clip is used in the same manner.
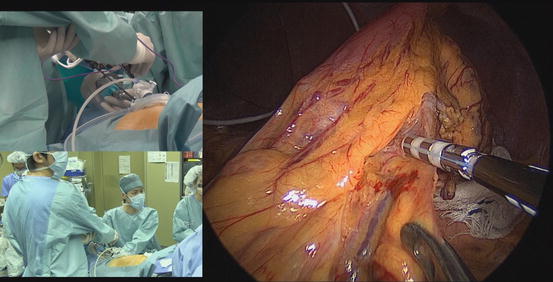
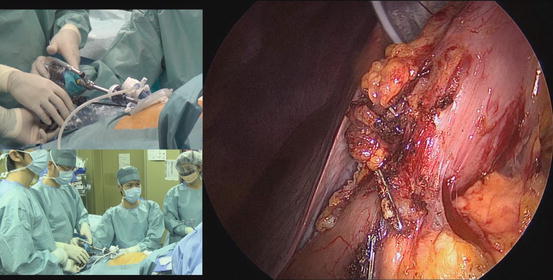
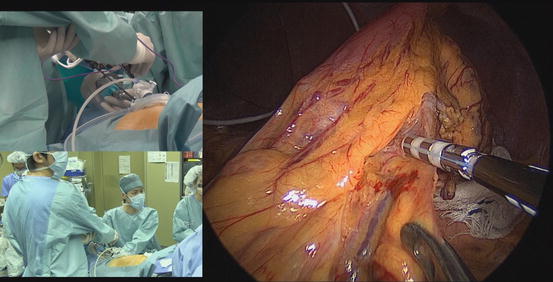
Fig. 18.11
The right side of the greater omentum is opened
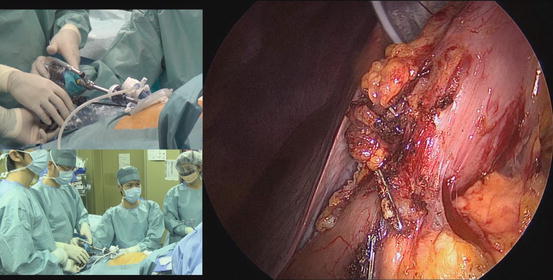
Fig. 18.12
No. 6 lymph node is completely dissected
Dividing the duodenum: before dividing duodenum, we open the lesser omentum around the pyloric area (Fig. 18.13). The stapler is inserted through the 12-mm trocar (Fig. 18.14), the cartridge should be appropriately articulated for identification of the staple line, and the duodenal bulb is divided (Fig. 18.15).
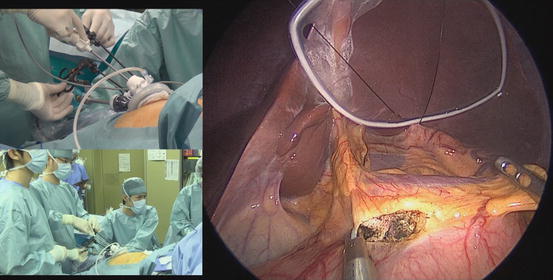
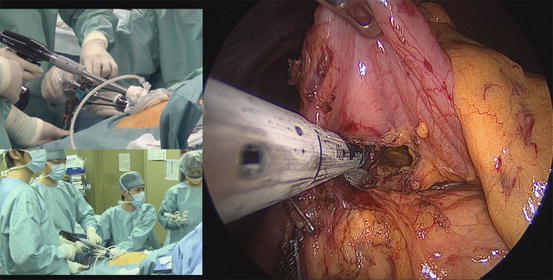
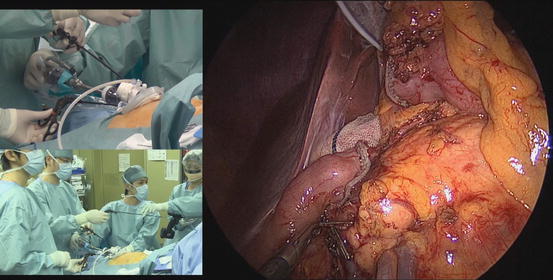
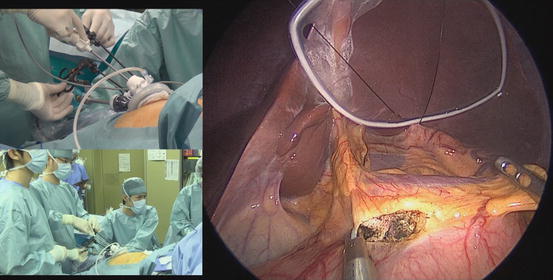
Fig. 18.13
The lesser omentum is opened around the pyloric area
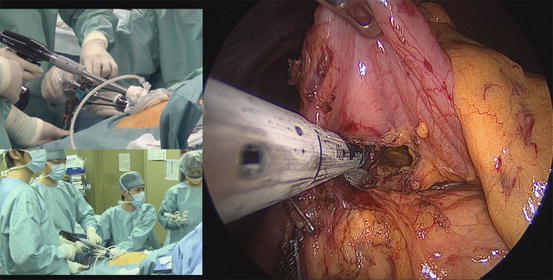
Fig. 18.14
Duodenal dividing with a liner stapler
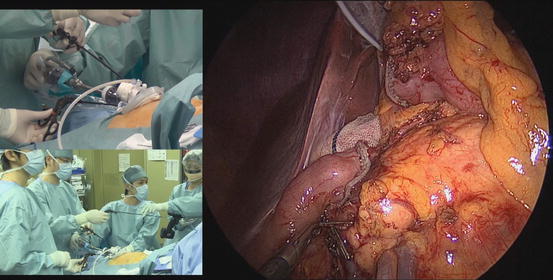
Fig. 18.15
Appropriate duodenal dividing
Dissection around the hepato-duodenal ligament: after division of the duodenum, the field around the hepato-duodenal ligament, including the root of the right gastric artery and vein, can be clearly seen. Dissecting along the surface of the gastro-duodenal artery, we first cut the serosa along the proper hepatic artery and open the lesser curvature up to the crura of the diaphragm (Fig. 18.16). In case of early gastric cancer, we preserve the hepatic branch of the vagus nerve. We then look for the surface of the neural layer around the common hepatic artery (Fig. 18.17), which is referred to as the “outer-most layer” [5], or “dissectable layer.” The outer-most layer should be preserved during the next step, dissection around the suprapancreatic area. The root of the right gastric artery and vein is encircled, clipped, and divided (Fig. 18.18). The lymph node at the left of the portal vein is appropriately dissected or preserved, according to the level of nodal dissection planned.