Indications
Hernia with a minimum defect size of 3 cm
Symptomatic hernia
Contraindications
Bowel injury
Intestinal strangulation
Intolerance to general anesthesia
Uncontrolled coagulopathy
Closing the hernia orifice even under local anesthesia can treat small ventral hernias. This method is, of course, less invasive than laparoscopic mesh repair. An Italian group [9] reported the indication for laparoscopic ventral hernia to be a hernia with a minimum defect of 3 cm (Fig. 30.1). The site of the defect does not seem to influence the indications/contraindications [9]. In cases of simultaneous contamination, due for example to bowel injury or intestinal strangulation, use of prosthesis is basically contraindicated. Uncontrolled coagulopathy is a contraindication for laparoscopic hernia surgery, and because the procedure is usually performed under general anesthesia, inability to tolerate general anesthesia is also a contraindication. Old age itself is not a contraindication for this procedure [10], and obese patients are good candidates for laparoscopic ventral hernia repair, too [11]. The indications and contraindications are basically the same for both conventional and RPLHR.


Fig. 30.1
A typical incisional hernia indicated for reduced-port laparoscopic hernia repair
The advantages and disadvantages of RPLHR should be considered. The obvious advantage of fewer ports is better cosmesis, although equivalence in terms of clinical outcome is not well established. Informed consent must be obtained from patients in a careful manner.
30.3 Technique
The patient is placed in a supine position. Hair surrounding the incisional area is removed, and the skin surface is prepared in a routine manner. The region is covered with sterile drapes. To ensure adequate overlap of the prosthetic mesh, more than 10 cm should be added to the maximum measurements of the fascial defect in all directions.
A small incision of 2–3 cm is made on the hernia bulge along the previous surgical scar (Fig. 30.2). This incision is used for the first trocar and for the port to introduce surgical sponges and the mesh for the hernia repair (Fig. 30.3). The subcutaneous tissue is carefully dissected down to the abdominal cavity. Once the hernia sac is opened, the abdominal contents are placed back in the abdomen. If severe adhesions around the hernia sac are observed, dissection 2 cm from the edge of the incision line is enough to place the first port. A silicone wound protector (Lap Protector™ (Hakko Co., Nagano, Japan)) is used, and a silicone cap (EZ Access™ (Hakko)) designed for the use of several trocars is set. There are other methods of initial trocar placement [12]. The best technique is the one with which the surgeon is most experienced and comfortable. After 10-mmHg pneumoperitoneum is established, a 5-mm trocar is inserted at least 4 cm away from the fascial edge, usually in the lateral abdomen. At least two trocars of 5-mm are necessary to introduce the laparoscope and a tacker for fixation of the mesh. These two trocars may be placed in a single-port. However, the longer incision may be a risk factor for development of an incisional hernia. Therefore, reducing the size of the ports rather than the number of ports would be preferable in this setting. If the planned trocar site cannot be visualized laparoscopically due to intraperitoneal adhesion, adhesiolysis is carried out from the first port with the use of several trocars.

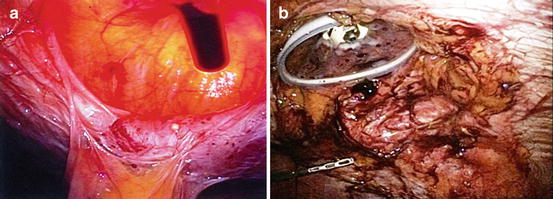

Fig. 30.2
Appearance of the surgical scar soon after reduced-port laparoscopic hernia repair
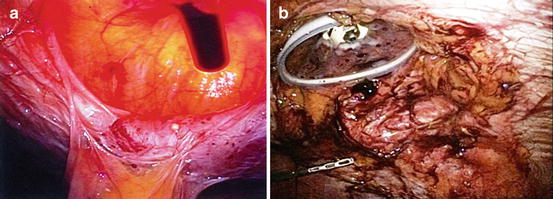
Fig. 30.3
The largest port through which the surgical sponges and mesh for hernia repair are introduced. This incision is made within the fascial defect
After complete detachment of all adhesions below the surgical scar, all incisional hernias must be evaluated, including small fascial defects (Fig. 30.4). Some surgeons prefer to close the edge of the fascial defect laparoscopically [13, 14]. The clinical merits of this technique are not well clarified. If the fascial defect is closed in patients with a large central defect, the “tension free” concept will be abandoned, and the risk of rupture of the closed hernia orifice and recurrence of the hernia may increase. However, the risk of seroma formation and mesh migration into the cavity will be minimized [15]. The mesh should be larger than the hernia defect with a margin of at least 3 cm in all directions. Some reports indicate that the overlap should be at least 5 cm. Indeed, the optimal amount of overlap depends on the size and the anatomical site of the hernia orifice.
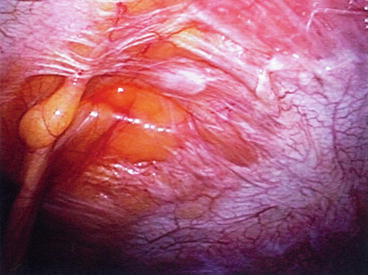
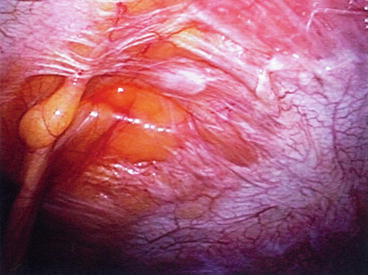
Fig. 30.4
All incisional hernias must be evaluated, including small fascial defects
Many prosthetic materials are now available for ventral hernia repair [16, 17]. We usually use Parietex™ Composite mesh (Covidien, New Haven, CT, USA), which has a reabsorbable collagen barrier on one side to limit visceral attachments and a polyester knit structure on the other [18]. The mesh is introduced through the largest port or a 12-mm trocar. With our procedure, the EZ Access™ silicone cap (Hakko) is opened, and the mesh is easily introduced through the wound protector and spread flat with the knitted side up. Pneumoperitoneum is re-established, and the collagen-covered surface is confirmed to be facing the viscera. After the mesh is successfully spread, the incision with the Lap Protector™ (Hakko) is closed. In patients with a relatively small hernia orifice, fascial separation is approximated before skin closure. Lifting stitches, which are connected to the edge of the mesh, are caught by a suture passer (EndoClose™ (Covidien)) and firmly fixed to the abdominal wall. With the use of fixation tacks [2], the edge of the mesh is circumferentially fixed to the abdominal wall (Fig. 30.5). Opinions vary on the method of mesh fixation, whether with a single or double crown of tacks, with or without defect closure [19]. We do not use the double crown configuration or defect closure routinely, although strong evidence supporting mesh fixation is lacking. A port site is carefully closed if the incision is longer than 5 mm. This is done to avoid development of an incisional hernia.


Fig. 30.5
The edge of the mesh is circumferentially fixed to the abdominal wall with fixation tackers
30.4 Tips and Tricks
To introduce the mesh into the abdominal cavity, a port of at least 12-mm in diameter is needed. This is a potential site of future incisional hernia. With our procedure, the largest incision through which prosthesis is inserted is made within the hernia defect and finally covered with the mesh prosthesis. One of the major advantages of RPLHR is improved cosmesis. Our method is reasonable in this respect because the longest incision is made on the previous surgical scar. All other ports are 5 mm or less in diameter.
For mesh fixation with a tacking device, a certain distance from the trocar to the edge of the mesh must be maintained to obtain an effective tacking angle. Therefore, at least two ports 5-mm in diameter should be placed, one on each side of the hernia. This limitation means that surgery performed through multiple small ports is preferable to that performed through a larger single-port. True RPLHR is possible for selected patients. The longer incision, however, may become a risk factor for an additional incisional hernia. Careful fascial closure of the large port site is essential. We usually place a port within the hernia bulge where the mesh will cover the incision. Other ports used for adhesiolysis and mesh fixation should be 5-mm at most.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








