Fig. 37.1
No visible scar

Fig. 37.2
Eversion of the umbilicus

Fig. 37.3
Port in place
Surgical Procedure
The first step of MGB is the creation of the gastric pouch of about 10-cm in length, measured from the angle of His. A perigastric dissection is carried out with the use of Ligasure Blunt Tip® (Covidien) coupled to a Endo Grasp Roticulator® (Covidien) that keeps traction on the stomach. These instruments cross each other at the navel allowing the creation of triangulation to exert traction and counter traction so typical of traditional laparoscopy. In this case the main trunk of the left gastric artery and the branches of the vagus nerve (the Latarjet) are preserved. Once the opening is made a 45-mm blue or purple cartridge EndoGIA® (Covidien) is fired and the first transverse section of the stomach is done (Fig. 37.4). During these maneuvers the instruments are crossed at the level of the port, so the stomach is maintained in tension by an Endo Grasp Roticulator® (Covidien), which appears into the right side of the screen but is controlled by the left hand of the surgeon. A 13-mm (outer diameter) orogastric probe is brought forward filling the pouch and is used for calibration; the stapler is applied as close as possible to the probe to ensure the small volume of the pouch. The stomach is transacted vertically (Fig. 37.5). Retraction of the left lobe of the liver was achieved with a transfix stitch, applied on the right crus and suspended from outside (Fig. 37.6). It is therefore unnecessary to use any dedicated tool. Several (3–5) applications of 60-mm blue or purple cartridges EndoGIA® (Covidien) are necessary to join the angle of His. Before completely dividing the pouch from the stomach you should find some short vessels that may need to be coagulated before inserting the stapler (Fig. 37.7). Moreover, this dissection allows for certainty of the separation of the pouch from the stomach. The pouch is made narrow and long, similar to the one done in sleeve gastrectomy. This method allows you to stay away from esophagus and helps when performing the gastroenteric anastomosis by decreasing the distance, and thus the tension, between the pouch itself and the intestine. Once the pouch is completed, the gastrotomy is opened. The hole is made on a free portion of the pocket, away from the rhymes of suture to avoid ischemia, on either the front or rear wall. The orogastric tube is withdrawn by 10-cm to avoid being accidentally caught in the coming anastomosis. The hole is enlarged with a small bowel clamp to facilitate the future introduction of the stapler. In this case you use regular scissors and straight clamp coupled with an articulated grasper. In the almost horizontal position, you perform the measurement of the bowel (Fig. 37.8): the omentum is shifted upward and to the left of the screen, the mesocolon is put under tension by pulling on an epiploic appendix in proximity of the left colic flexure, where it is thin enough and relaxed enough to allow easy exposure the ligament of Treitz. The biliary limb is measured up to 200-cm from the Treitz’s ligament. After the enterotomy is done (Fig. 37.9) an articulated 30-mm blue cartridge EndoGIA® (Covidien) (anvil) is introduced into the bowel, and then the stapler is closed and approaches the gastric pouch: the direction of the joint is changed and the head of the stapler is rotated by 180°. At this point the cartridge of the stapler presents itself ready in proximity to the gastrotomy. The patient is put back into an anti-Trendelemburg position and using both the stapler and an articulated grasper the pouch is retrieved. The pouch is pulled down and the gastroenteric anastomosis is performed (Fig. 37.10). Its wedge shape facilitates the insertion of the cartridge in the stomach. The service opening is closed with a hand-made suture carried out with the Endostitch® (Covidien) (Fig. 37.11): it consists of an initial extra mucous layer and a second serosal layer in polysorbate 2/0. The anastomosis is checked with the methylene-blue test while two clamps close both the afferent and efferent loops. The last step of the procedure is the creation of an anti-reflux mechanism (Fig. 37.12): the firsts 5- to 6-cm of the afferent loop are sutured to the pouch vertically, and so provide a preferential way for food and liquid progressing toward the alimentary/efferent limb and thus reduce the risk of reflux of bile into the pouch.
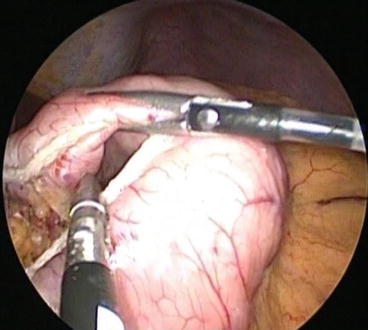
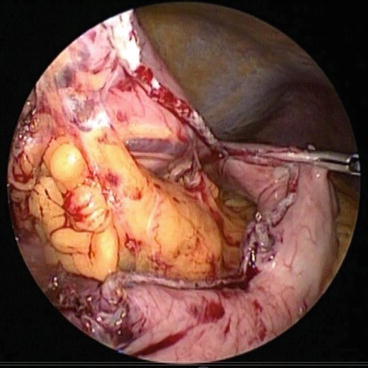
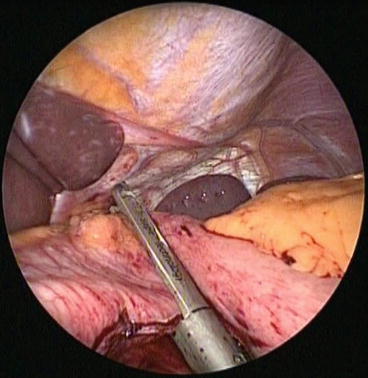
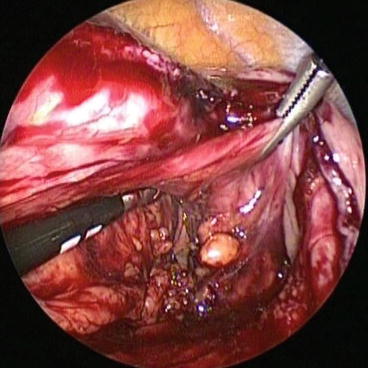
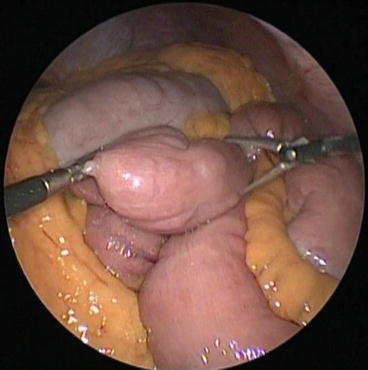

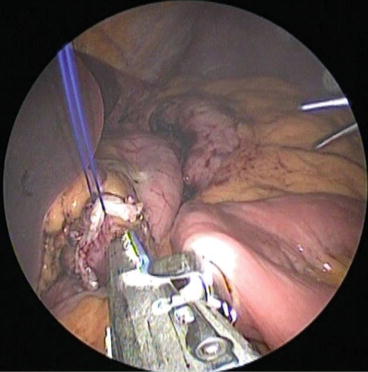
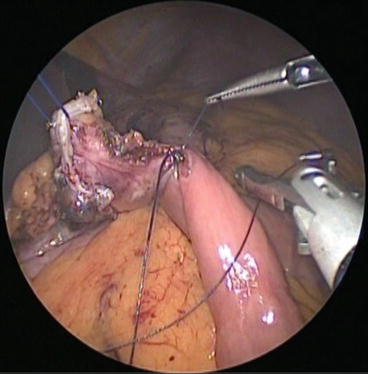
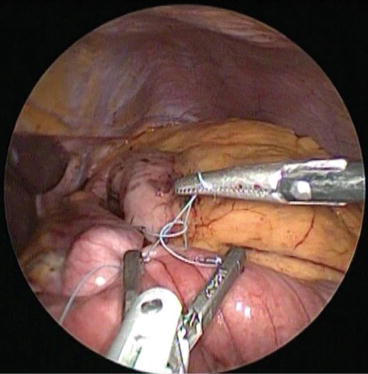
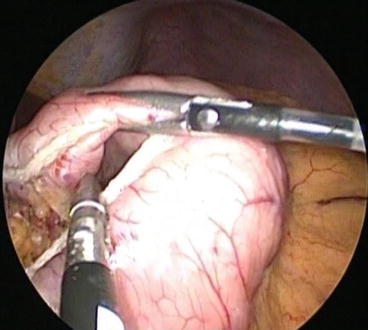
Fig. 37.4
Horizontal transverse section of stomach
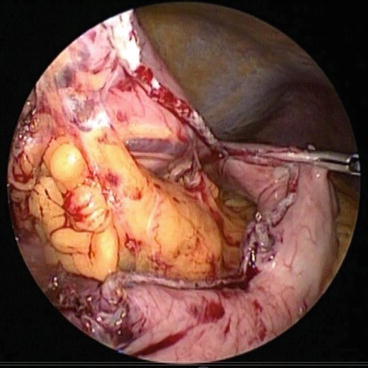
Fig. 37.5
Vertical stapling along calibration orogastric tube
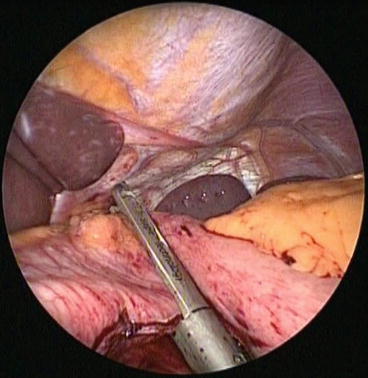
Fig. 37.6
Liver retraction
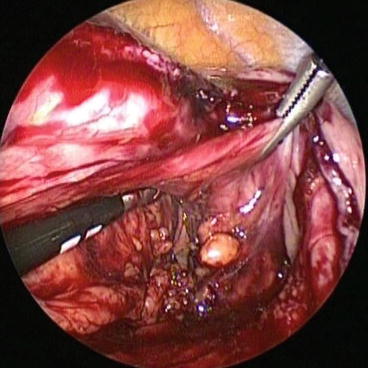
Fig. 37.7
Ensure complete division
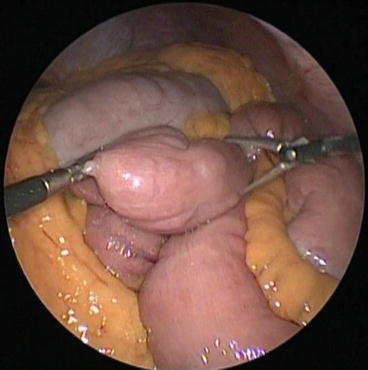
Fig. 37.8
Small bowel measurement

Fig. 37.9
Enterotomy
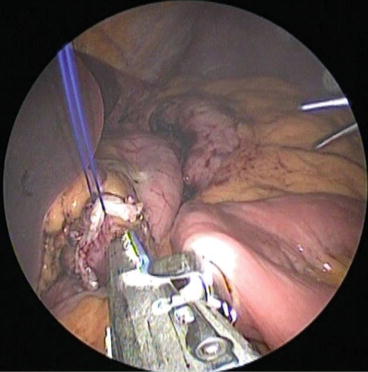
Fig. 37.10
Gastroenteric anastomosis
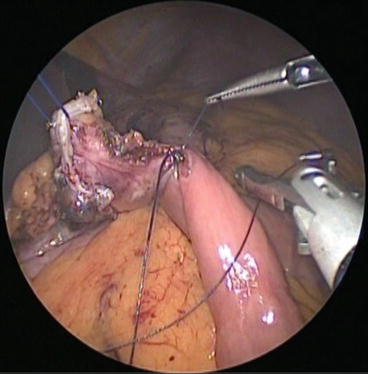
Fig. 37.11
Closing of the service opening
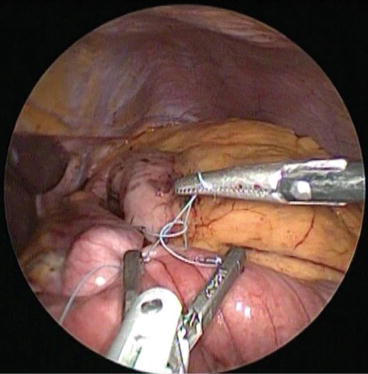
Fig. 37.12
Afferent loop sutured to the gastic pouch
A last stitch will fix the efferent limb to the antrum (Fig. 37.13).
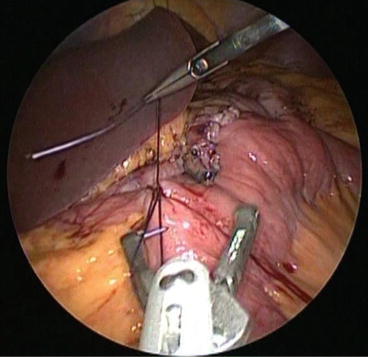
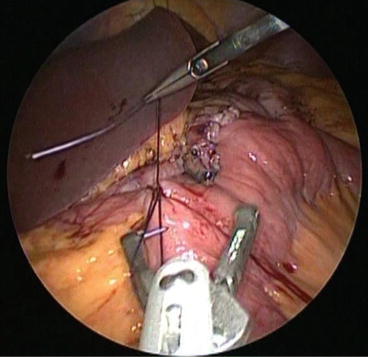
Fig. 37.13
Efferent loop sutured to the gastric antrum
Roux-en-Y Conversion
A Roux-en-Y reconstruction may be accomplished, if necessary, in an easy way after the gastroenteric anastomosis is done, with the “double loop” technique: at about 10-cm from the gastroenteric anastomosis along the biliary limb an enterotomy is made for the next entero-enteric anastomosis. The second loop (alimentary limb) is measured starting from the gastroentero anastomosis just completed toward the ileocecal valve and the enteroenteric anastomosis is performed. With this technique the surgical field of view is very restricted and the movements are minimized thus facilitating the implementation of the intervention and reducing the risk of twisting the mesentery. The last step of the intervention is the interruption of continuity between the two anastomosis to create the Roux-en-Y: a passage into the mesentery near the intestinal wall is made without using coagulation, being careful not to cause vascular damage to prevent ischemia; a 60-mm white cartridge EndoGIA® (Covidien) is inserted in the passage created and the stapler is fired.
No drainage was left in place. The operation ends with the evacuation of the pneumoperitoneum and the removal of the port. The fascia is closed with an absorbable suture and the navel is reinstated in its original position [2].
37.1.3 BPD
The BPD as originally described by Scopinaro [11] has in the years undergone several modifications that however have not altered the fundamental working principle: limited absorption of fat and carbohydrates.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








